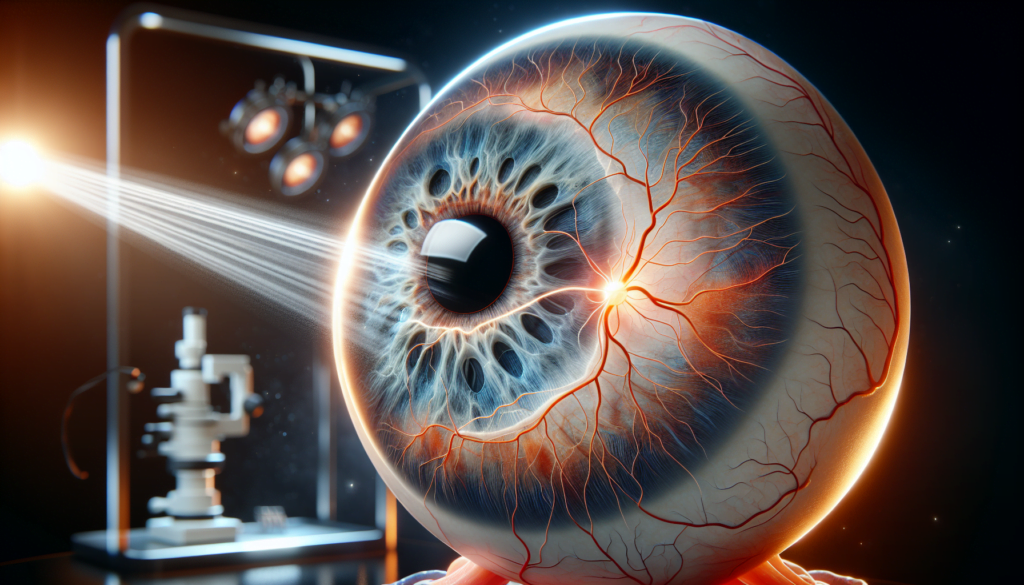
Retinal detachment is a serious eye condition that requires immediate medical attention. This vision-threatening emergency occurs when the retina, the light-sensitive layer at the back of the eye, separates from its supporting tissue. Prompt recognition of retinal detachment symptoms and swift action in seeking retinal detachment treatment are crucial to prevent permanent vision loss. Understanding the causes, diagnosis, and available treatments can make a significant difference in the outcome for patients facing this challenging condition.
This article delves into the complexities of retinal detachment, exploring its various causes and the journey patients undergo during diagnosis. It examines different retinal detachment treatments, comparing their effectiveness and suitability for different cases. Additionally, the article sheds light on the recovery process and what patients can expect in the aftermath of retinal detachment surgery. By providing comprehensive information on this critical eye condition, readers will gain valuable insights to help them navigate the challenges of retinal detachment and its treatment options.
Causes of Retinal Detachment
Several factors can lead to retinal detachment, ranging from age-related changes in the eye to trauma and underlying health conditions. Understanding these causes is crucial for identifying risk factors and taking preventive measures.
Age-Related Factors
As people age, the vitreous gel inside the eye can change in texture and shrink. This process can cause the vitreous to pull on the retina, potentially leading to tears or detachment. Aging is the most common cause of rhegmatogenous retinal detachment, which happens when fluid enters through a retinal tear and separates the retina from the back of the eye. Patients over 50 are at a higher risk of developing this type of retinal detachment.
RELATED: Throat Cancer: Key Symptoms and Effective Treatments
Trauma and Injury
Eye injuries are another significant cause of retinal detachment. Blunt trauma, such as a strong blow to the eye from a ball or fist, can cause the retina to detach due to the force of the impact. Penetrating injuries from objects like glass shards or metal fragments can also directly damage the retina. Rapid acceleration or deceleration, as experienced in car accidents, and explosive or shock wave injuries can exert force on the retina, potentially causing detachment.
Underlying Health Conditions
Certain health conditions can increase the risk of retinal detachment. Diabetic retinopathy, an eye condition associated with diabetes, can cause scar tissue formation on the retina. As the scars grow, they can pull the retina away from the back of the eye, leading to tractional retinal detachment. Other eye diseases like lattice degeneration and retinoschisis can cause thinning or separation of the retina, making it more susceptible to detachment. Extreme nearsightedness (high myopia) and previous eye surgeries, particularly cataract removal, are also risk factors for retinal detachment.
The Diagnostic Journey
Initial Consultation
When a patient experiences symptoms of retinal detachment, such as sudden flashes of light, floaters, or a curtain-like shadow in their visual field, an initial consultation with an eye care professional is crucial. During this visit, the doctor will take a detailed medical history and ask about the onset and duration of symptoms. This information helps the doctor determine the urgency of the situation and the likelihood of retinal detachment.
Specialized Tests
To confirm the diagnosis of retinal detachment and assess the extent of the condition, the doctor will perform a comprehensive eye exam using specialized tests. These may include a dilated fundus examination, where the doctor uses eye drops to widen the pupil and examines the retina using a special lens. An ultrasound of the eye may be necessary if the view of the retina is obscured by bleeding or clouding. Optical coherence tomography (OCT) is another non-invasive imaging test that provides detailed cross-sectional images of the retina, helping to identify areas of detachment or tears.
Creating a Treatment Plan
Once the diagnosis of retinal detachment is confirmed, the doctor will discuss treatment options with the patient. The choice of treatment depends on factors such as the location and extent of the detachment, the presence of retinal tears or holes, and the patient’s overall health. The doctor will explain the risks and benefits of each retinal detachment treatment approach, which may include laser surgery, cryotherapy, scleral buckling, or vitrectomy. Together, the doctor and patient will develop a personalized treatment plan to address the retinal detachment and preserve vision.
Comparing Treatment Approaches
Non-Surgical vs. Surgical Options
Retinal detachment treatment options can be broadly categorized into non-surgical and surgical approaches. Non-surgical methods, such as laser photocoagulation and cryotherapy, are suitable for treating small retinal tears or holes before they progress to a full-blown detachment. These procedures seal the tear by creating a scar around it, preventing fluid from entering the space behind the retina. On the other hand, surgical interventions become necessary when a significant portion of the retina has detached. The choice between non-surgical and surgical treatment depends on factors like the extent of the detachment, the presence of retinal tears, and the patient’s overall health.
RELATED: Understanding Systemic Inflammatory Response Syndrome (SIRS)
Factors Influencing Treatment Choice
Several factors influence the decision-making process when choosing the most appropriate retinal detachment treatment. The location and size of the detachment play a crucial role, as detachments involving the macula or a large area of the retina often require surgical intervention. The presence and number of retinal tears also impact treatment selection, with multiple or large tears usually necessitating surgery. Patient characteristics, such as age and general health status, are considered to determine the most suitable approach. Additionally, the surgeon’s expertise and the availability of specialized equipment may influence the treatment choice.
Success Rates
The success rates of various retinal detachment treatments vary depending on the specific technique and the complexity of the case. Laser photocoagulation and cryotherapy have high success rates in preventing the progression of small retinal tears to full detachment. For surgical interventions, the anatomical success rate, defined as the complete reattachment of the retina, ranges from 80% to 90%. However, the functional success rate, which takes into account the improvement in vision, may be lower, especially in cases where the macula was involved or the detachment was longstanding. Prompt diagnosis and timely treatment are key factors in achieving the best possible outcomes in retinal detachment.
Life After Retinal Detachment Surgery
Short-term Recovery Process
After retinal detachment surgery, patients should expect some discomfort, swelling, and redness in the treated eye. These symptoms gradually improve over the first few weeks. Patients may also experience floaters, flashing lights, and blurry vision during this time. Eye drops or ointments prescribed by the doctor help reduce pain, swelling, and the risk of infection. It is crucial to rest and limit physical activity for the first two weeks after surgery. Patients should avoid bending below the waist, moving suddenly, straining, or lifting more than 20 pounds. If a gas bubble was injected into the eye during surgery, patients must maintain a specific head position, often face down, for several days to a week or more. This positioning helps the bubble float to the right location and hold the retina in place. Patients should also avoid sleeping on their back until the bubble has dissipated or the oil is removed surgically.
RELATED: Sinus Headache Guide: From Diagnosis to Treatment Options
Long-term Vision Outlook
Vision typically starts to improve within 4-6 weeks after retinal detachment surgery. However, it can take months for vision to stabilize fully. In many cases, patients can recover their pre-detachment vision, especially when the detachment is caught and treated early. The retina may take a year or more to heal completely. Factors influencing the long-term vision outlook include the extent of the detachment, the involvement of the macula, and the time between the onset of retinal detachment symptoms and treatment. Regular follow-up visits with the doctor are essential to monitor the healing process and address any complications that may arise.
Preventing Future Detachments
While retinal detachment surgery is highly successful, with around 90% of retinas being successfully reattached, patients must take steps to prevent future detachments. This is particularly important for those with risk factors such as high myopia, a history of retinal detachment in the other eye, or a family history of the condition. Patients should attend all scheduled follow-up appointments with their eye doctor to monitor the health of their retina. They should also be aware of the warning signs of retinal detachment, such as sudden flashes of light, floaters, or a curtain-like shadow in their visual field. If any of these retinal detachment symptoms occur, patients should seek immediate medical attention to prevent vision loss. Maintaining a healthy lifestyle, protecting the eyes from trauma, and managing underlying health conditions can also help reduce the risk of future retinal detachments.
Conclusion
Retinal detachment is a serious eye condition that requires prompt attention and treatment to prevent permanent vision loss. This article has explored the causes, diagnostic process, treatment options, and recovery journey for patients facing this challenging condition. By understanding the risk factors and recognizing the symptoms early, individuals can take swift action to seek medical help, increasing their chances of a successful outcome.
The journey through retinal detachment diagnosis, treatment, and recovery can be complex, but with advancements in medical technology and surgical techniques, the outlook for patients is increasingly positive. Regular eye check-ups, awareness of symptoms, and a proactive approach to eye health are key to preventing and managing retinal detachment. In the end, the goal is to preserve vision and maintain a high quality of life for those affected by this condition.