Spider veins are a common cosmetic concern that affects millions of people worldwide. These small, dilated blood vessels appear close to the skin’s surface, often resembling a web-like pattern of red, blue, or purple lines. While they typically don’t pose serious health risks, spider veins can cause discomfort and self-consciousness for those who have them.
This article delves into the causes and symptoms of spider veins, shedding light on why they develop and how to spot them. It also explores the various treatment options available, from conservative approaches to cutting-edge medical procedures. By understanding these aspects, readers will gain valuable insights to help them make informed decisions about managing and treating spider veins effectively.
Understanding Spider Veins



Definition and Appearance
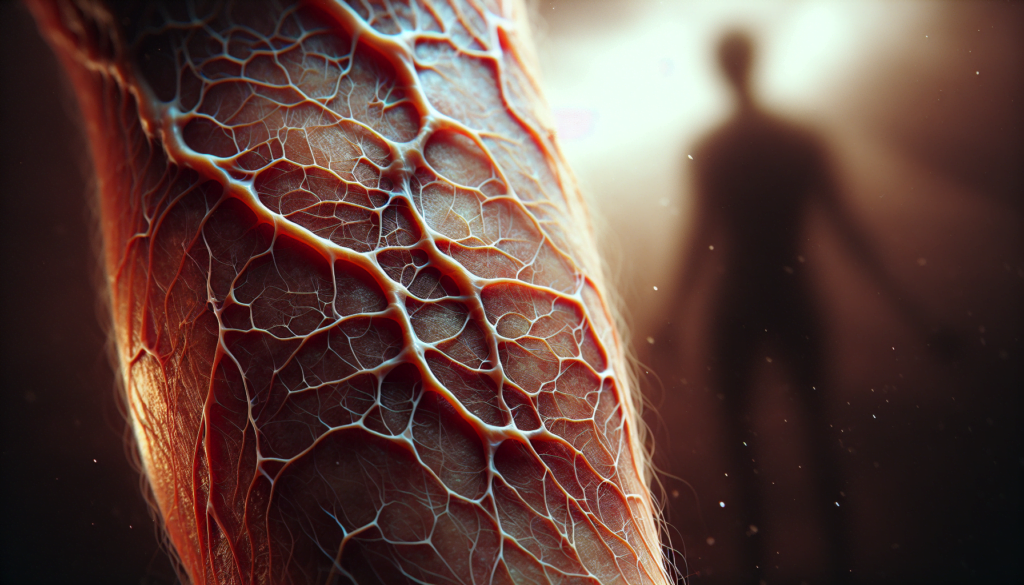
Spider veins, medically known as telangiectasias, are small, damaged blood vessels that appear close to the skin’s surface. They typically look like thin, red, blue, or purple lines that branch out in a web-like pattern. These damaged capillaries, venules, and arterioles are usually less than 1 mm in diameter and can be flat or slightly raised.
Types of Spider Veins
There are different types of spider veins, classified based on their appearance. Simple linear spider veins appear as single, thin lines, while spider-shaped ones radiate from a central point. Arborizing spider veins resemble tree branches, and papular ones look like small, round spots. The appearance can vary depending on the location and the underlying cause.
RELATED: Polio: Historical Outbreaks and Modern Vaccine Efforts
Difference from Varicose Veins
Although often confused, spider veins and varicose veins are distinct conditions. Varicose veins are larger, typically more than 3 mm in diameter, and often appear as bulging, twisted cords. They are usually deeper in the skin compared to spider veins. While spider veins are primarily a cosmetic concern, varicose veins can cause discomfort and lead to more serious complications if left untreated.
It’s important to note that the presence of spider veins does not necessarily indicate an underlying venous disorder. However, in some cases, they may be an early sign of chronic venous insufficiency (CVI). A healthcare provider can assess the overall venous health and determine if further evaluation or treatment is necessary. Understanding the characteristics and differences between spider veins and varicose veins can help individuals make informed decisions about their vein health and cosmetic concerns.
Causes and Risk Factors
Genetic Predisposition
Genetics play a significant role in the development of spider veins. If a person has a family history of this condition, they are more likely to develop spider veins themselves. Recent research has focused on identifying specific genetic markers associated with an increased risk of developing spider veins. Understanding these genetic factors can help healthcare providers identify individuals at higher risk and develop targeted prevention and treatment strategies.
Hormonal Changes
Hormonal fluctuations, particularly in estrogen and progesterone levels, can influence the formation of spider veins. Women are more susceptible to spider veins during certain life stages, such as pregnancy and menopause, when hormonal changes are more pronounced. Estrogen is believed to weaken vein walls, making them more prone to dilation and the development of spider veins. Additionally, the use of hormone replacement therapy or birth control pills containing estrogen may increase the risk of developing spider veins.
RELATED: Quick Solutions for Pimples: Home Remedies and Treatments
Lifestyle Factors
Certain lifestyle factors can contribute to the development of spider veins. Obesity, for example, can amplify an individual’s genetic predisposition to spider veins by placing extra strain on the circulatory system. Maintaining a healthy weight through a balanced diet and regular exercise can help mitigate this risk. A sedentary lifestyle, characterized by prolonged periods of sitting or standing, can also increase venous pressure and exacerbate the genetic likelihood of developing spider veins. Engaging in regular physical activity and taking frequent breaks to move around can help promote healthy circulation and reduce the risk of spider veins.
Age and Gender
Age is another significant risk factor for spider veins. As people get older, their veins naturally lose elasticity, and the valves that regulate blood flow may weaken. This can lead to an increased likelihood of developing spider veins, especially in the legs. Women are more prone to spider veins than men, partly due to hormonal influences and the effects of pregnancy on the circulatory system. However, it is important to note that spider veins can affect individuals of any age and gender, particularly if they have a strong genetic predisposition or are exposed to other risk factors.
Symptoms and Diagnosis
Common Symptoms
While spider veins are primarily a cosmetic concern, some individuals may experience symptoms such as itching, burning, or a feeling of heaviness in the affected area. In rare cases, spider veins can cause discomfort or cramping, particularly after prolonged periods of standing or sitting. However, most people with spider veins do not experience any significant symptoms, and the presence of these damaged blood vessels does not necessarily indicate an underlying health issue.
When to Seek Medical Attention
Although spider veins are generally harmless, it is important to consult a healthcare provider if you notice any accompanying symptoms or changes in the appearance of your skin. Seek medical attention if you experience persistent pain, swelling, or skin ulcers near the affected veins. These symptoms may indicate a more serious underlying condition, such as chronic venous insufficiency, which requires prompt evaluation and treatment to prevent complications.
Diagnostic Procedures
Diagnosing spider veins typically involves a visual examination of the affected area by a healthcare professional. During the examination, the provider will assess the size, location, and extent of the spider veins. They may also inquire about any symptoms you are experiencing and your medical history to determine if there are any underlying factors contributing to the development of spider veins.
In some cases, additional diagnostic tests may be necessary to evaluate the overall health of your venous system. Duplex ultrasound, a non-invasive imaging technique, can be used to assess blood flow and check for any abnormalities in the deeper veins. This test can help identify if there are any underlying venous disorders, such as venous reflux or blood clots, which may require further treatment.
Treatment Options
Conservative Treatments
Conservative treatments for spider veins include lifestyle changes and compression stockings. Maintaining a healthy weight, exercising regularly, and avoiding prolonged periods of standing or sitting can help alleviate symptoms and prevent the progression of spider veins. Wearing compression stockings applies gentle pressure to the legs, promoting better blood circulation and reducing the appearance of spider veins. These stockings come in various lengths and compression strengths, with the most frequently prescribed being European standard class II for symptoms of venous hypertension.
Sclerotherapy
Sclerotherapy is considered the gold standard treatment for spider veins, particularly on the legs. This minimally invasive procedure involves injecting a sclerosing agent directly into the affected veins using a fine needle. The sclerosing agent causes the vein walls to collapse and seal shut, redirecting blood flow to healthier veins. Over time, the treated veins fade and are reabsorbed by the body. Sclerotherapy is effective for both small and large spider veins, although multiple treatment sessions may be necessary to achieve the desired results. Common side effects include bruising, swelling, and temporary skin discoloration.
RELATED: Phobias Uncovered: Types, Symptoms, and How to Treat Them
Laser Therapy
Laser therapy is a non-invasive treatment option for spider veins, especially those on the face or in patients who are allergic to sclerosing agents or have a fear of needles. This method uses targeted light energy to heat and destroy the damaged veins without harming the surrounding skin. Various types of lasers are available, each with specific wavelengths and pulse durations suitable for different skin types and vein sizes. While laser therapy can effectively treat smaller spider veins, it may be less effective for larger veins compared to sclerotherapy. Side effects may include temporary redness, swelling, and skin discoloration.
Radiofrequency Ablation
Radiofrequency ablation (RFA) is a minimally invasive procedure that uses heat generated by radiofrequency energy to seal off and eliminate spider veins. A thin catheter is inserted into the affected vein, and the radiofrequency energy is delivered to the vein walls, causing them to collapse and close. The treated vein is then reabsorbed by the body over time. RFA is particularly effective for larger spider veins and can be performed under local anesthesia in an outpatient setting. Potential side effects include temporary bruising, swelling, and numbness in the treated area.
Conclusion
Spider veins, while primarily a cosmetic concern, can have a significant impact on an individual’s self-esteem and quality of life. Understanding the causes, symptoms, and available treatment options is crucial to make informed decisions about managing this condition. From genetic predisposition to lifestyle factors, various elements contribute to the development of spider veins, highlighting the importance of a holistic approach to prevention and treatment.
The range of treatment options, from conservative methods to advanced medical procedures, offers hope to those seeking to address their spider veins. Whether opting for compression stockings, sclerotherapy, laser therapy, or radiofrequency ablation, individuals can work with healthcare providers to find the most suitable solution for their specific needs. As research in this field continues to advance, new and more effective treatments may emerge, providing even better outcomes for those affected by spider veins.