Urethritis is a common but often overlooked condition that affects millions of people worldwide. This inflammation of the urethra, the tube that carries urine out of the body, can cause discomfort and pain during urination. While it may seem like a minor issue, urethritis can have a significant impact on a person’s quality of life and sexual health if left untreated.
Understanding urethritis is crucial for early detection and proper treatment. This guide aims to provide comprehensive information on the causes, diagnosis, and management of urethritis. It will cover the different types of urethritis, common symptoms to watch out for, and the various testing procedures used to confirm the condition. Additionally, the guide will explore effective treatment approaches and potential complications, as well as prevention strategies to help reduce the risk of developing urethritis.
What is Urethritis?
Definition and Anatomy
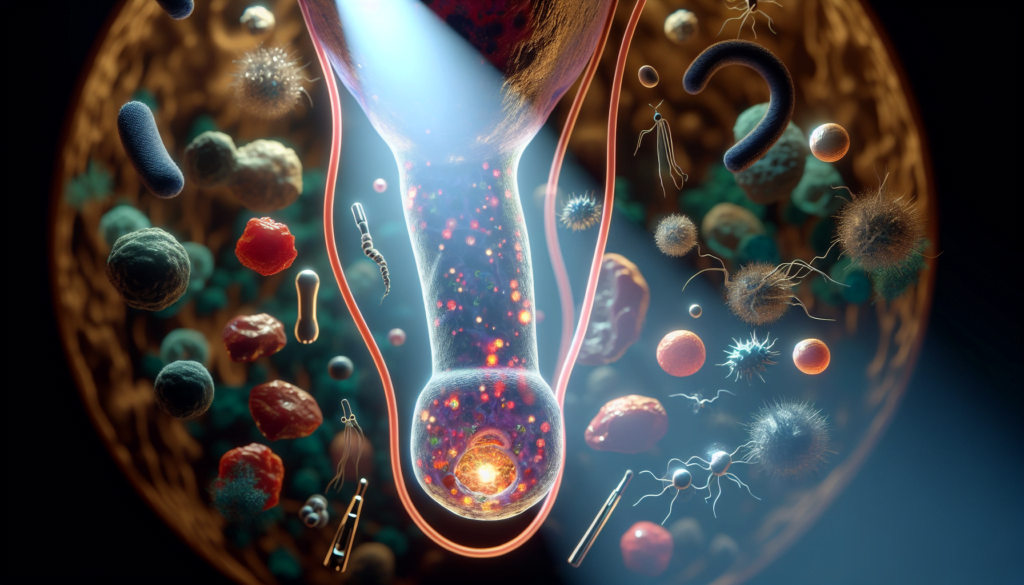
Urethritis is an inflammation of the urethra, the tube that carries urine from the bladder to the outside of the body. The urethra is lined with mucous membranes, which can become irritated and swollen due to various causes, such as bacterial or viral infections, chemical irritants, or physical trauma. In males, the urethra is longer and runs through the penis, while in females, it is shorter and opens just above the vagina.
Difference Between Urethritis and UTIs
Although urethritis and urinary tract infections (UTIs) share some similarities, they are distinct conditions. Urethritis specifically refers to the inflammation of the urethra, whereas a UTI can affect any part of the urinary system, including the bladder, ureters, and kidneys. However, the same bacteria that cause UTIs, such as E. coli, can also lead to urethritis. It is important to distinguish between the two conditions as they may require different treatment approaches.
RELATED: Metabolic Syndrome: A Complete Overview of Symptoms and Treatments
Risk Factors
Several factors can increase the risk of developing urethritis. These include having multiple sexual partners, engaging in high-risk sexual behavior, and having a history of sexually transmitted infections (STIs). Women are more prone to urethritis due to their shorter urethra, which allows bacteria to enter the urinary tract more easily. Other risk factors include the use of spermicides, contraceptive jellies, or foams, which can cause irritation to the urethra. In some cases, injury or trauma to the urethra can also lead to inflammation and the development of urethritis.
Common Causes of Urethritis
Sexually Transmitted Infections
Sexually transmitted infections (STIs) are the most common causes of urethritis. Chlamydia trachomatis is the most prevalent bacterial STI responsible for urethritis, accounting for up to 50% of cases. It is easily transmitted through unprotected sexual intercourse and has an incubation period of 1-4 weeks. Neisseria gonorrhoeae, the second most common bacterial cause of urethritis, is also transmitted via unprotected sexual contact and has a shorter incubation period of 1-10 days. Other STIs that can lead to urethritis include Mycoplasma genitalium, Trichomonas vaginalis, and Herpes simplex viruses 1 and 2.
Non-STI Bacterial Causes
In some cases, urethritis can be caused by bacteria that are not sexually transmitted. These include Ureaplasma urealyticum, which has been associated with urethritis in men with high bacterial loads, and Haemophilus influenzae, which can be transmitted to the urethra through oral sex. However, the role of these bacteria in causing urethritis is still under investigation, and they are considered less common than STIs.
Viral and Other Causes
Viral infections, such as Adenovirus, can cause urethritis in a small percentage of cases (2-4%). Adenovirus-associated urethritis is most likely transmitted through unprotected oral sex and typically presents with symptoms of meatitis, dysuria, and clear or mucoid discharge. In rare instances, urethritis may be caused by non-infectious factors, such as chemical irritants, physical trauma, or urinary tract infections. These non-STI causes of urethritis should be considered when STIs have been ruled out, and symptoms persist despite appropriate antibiotic treatment.
Diagnosis and Testing Procedures
Physical Examination
A physical examination is crucial in diagnosing urethritis. Healthcare providers will examine the urethral meatus for signs of inflammation, such as redness, swelling, or tenderness. They will also check for the presence of urethral discharge, which can be purulent or mucopurulent. Palpating along the urethra can help identify areas of fluctuance, warmth, or firmness, suggesting an abscess or foreign body. In male patients, the testes and epididymis should be examined for swelling or tenderness, which may indicate orchitis or epididymitis. The prostate should also be palpated to check for tenderness or bogginess, suggestive of prostatitis.
Urine Tests
Urine tests can be helpful in diagnosing urethritis. A positive leukocyte esterase test from a first-void urine sample or the presence of ≥ 10 white blood cells per high-power field (WBC/hpf) in the sediment of a spun first-void urine sample can indicate urethritis. However, urinalysis is not always a reliable diagnostic tool, as more than 30% of patients with nongonococcal urethritis may not have leukocytes in their urine specimens.
RELATED: Mesothelioma: In-Depth Look at Symptoms, Causes, and Treatments
Swab Tests
Endourethral swabs are essential for diagnosing urethritis caused by sexually transmitted infections (STIs). Gram staining of urethral secretions can demonstrate ≥ 2 WBC per oil immersion field, indicating urethritis. The sensitivity of urethral Gram stain depends on the collection method and the provider’s experience. Endourethral cultures, obtained by gently inserting a malleable cotton-tipped swab 1-2 cm into the urethra, are necessary to test for Chlamydia trachomatis infection. Cultures for Neisseria gonorrhoeae should be obtained in cases of sexual assault, developing antimicrobial resistance, or suspected gonorrhea treatment failures.
Blood Tests
Blood tests can be useful in diagnosing urethritis and associated conditions. Patients with urethritis should be offered syphilis serology, such as the Venereal Disease Research Laboratory (VDRL) test or Rapid Plasma Reagin (RPR) test, and HIV serology. Men diagnosed with nongonococcal urethritis should be tested for HIV and syphilis. In cases of reactive arthritis, elevated erythrocyte sedimentation rate (ESR) in the absence of rheumatoid factor may be helpful in diagnosis.
Treatment Approaches and Complications
Antibiotic Therapy
The primary treatment for urethritis caused by bacterial infections is antibiotic therapy. The choice of antibiotics depends on the specific pathogen identified through testing. For gonococcal urethritis, the CDC recommends a single dose of ceftriaxone 500 mg intramuscularly or cefixime 800 mg orally. If chlamydial infection has not been excluded, doxycycline 100 mg orally twice a day for 7 days should also be administered. For non-gonococcal urethritis, doxycycline 100 mg orally twice a day for 7 days is the recommended treatment. Azithromycin, given as a single 1 g dose orally or 500 mg orally followed by 250 mg orally daily for 4 days, is an alternative regimen.
Antiviral Medications
In cases where urethritis is caused by viral infections such as herpes simplex virus, antiviral medications are used for treatment. Acyclovir, famciclovir, and valacyclovir are commonly prescribed antiviral drugs that can help alleviate symptoms and reduce the duration of the infection. These medications work by inhibiting viral replication, allowing the body’s immune system to fight off the infection more effectively.
RELATED: Muscle Spasms: Common Triggers and How to Avoid Them
Potential Complications if Left Untreated
Untreated urethritis can lead to serious complications, particularly in cases of sexually transmitted infections. In men, untreated gonococcal or chlamydial infections can cause epididymitis, an inflammation of the epididymis, which may result in pain, swelling, and fertility issues. Prostatitis, an inflammation of the prostate gland, is another potential complication that can cause pain, urinary symptoms, and sexual dysfunction. In rare cases, untreated urethritis can lead to the development of reactive arthritis, a condition characterized by joint pain and inflammation. Additionally, untreated STIs can increase the risk of HIV transmission. Prompt diagnosis and appropriate treatment of urethritis are crucial in preventing these complications and reducing the spread of infections to sexual partners.
Conclusion
Urethritis is a condition that has a significant impact on the urinary and reproductive health of many individuals. This guide has shed light on the causes, diagnosis, and treatment of urethritis, highlighting the importance of early detection and proper management. By understanding the risk factors and common symptoms, individuals can take proactive steps to protect their health and seek medical attention when needed.
Moving forward, it’s crucial to raise awareness about urethritis and its potential complications. Healthcare providers play a key role in accurate diagnosis and effective treatment, while patients must be proactive in their sexual health. By promoting safe sexual practices and regular check-ups, we can work towards reducing the incidence of urethritis and its associated health risks. Remember, timely intervention and proper care are essential to maintain urinary health and overall well-being.