A cystocele, commonly known as a fallen bladder, is a condition that affects many women, particularly as they age. This pelvic floor disorder occurs when the supportive tissue between a woman’s bladder and vaginal wall weakens, allowing the bladder to bulge into the vagina. The impact of this condition on a woman’s quality of life can be significant, causing discomfort and affecting daily activities.
Understanding cystocele is crucial for women’s health. This article delves into the nature of a fallen bladder, its symptoms, and the factors that contribute to its development. It also explores how doctors diagnose this condition and the range of treatment options available, from conservative approaches to surgical interventions. By shedding light on this common yet often overlooked issue, we aim to empower women with the knowledge to seek timely care and improve their overall well-being.
What is a Cystocele?
Definition
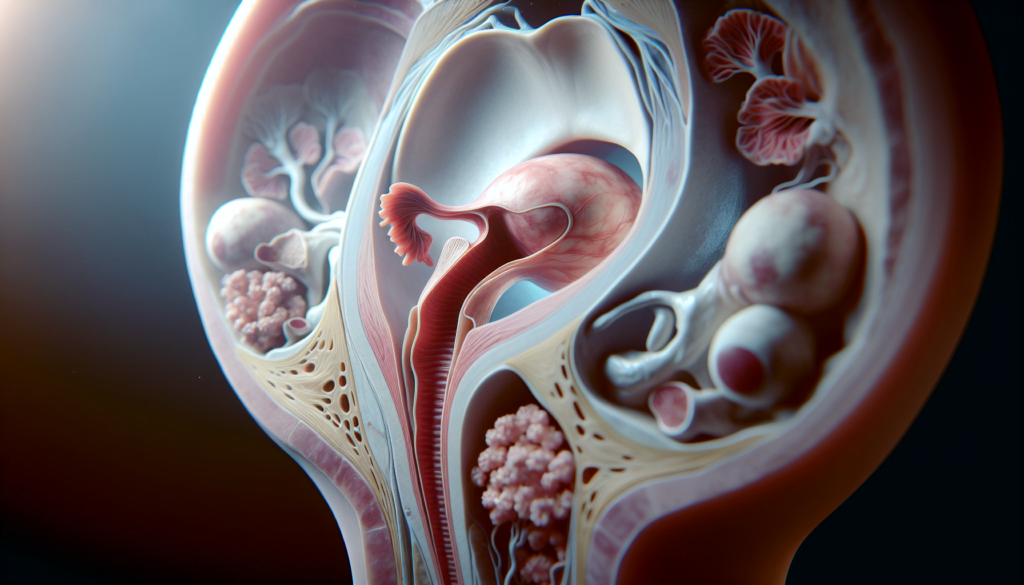
A cystocele, also known as a fallen bladder, is a condition that occurs when the supportive tissues between a woman’s bladder and vaginal wall weaken and stretch, allowing the bladder to bulge or herniate into the vagina. This type of pelvic organ prolapse can cause discomfort and problems with urination.
Types of Cystoceles
Cystoceles are categorized into three grades based on the severity of the prolapse:
- Grade 1 (mild): The bladder sags only slightly into the vagina.
- Grade 2 (moderate): The bladder drops to the opening of the vagina.
- Grade 3 (severe): The bladder bulges through the vaginal opening.
The degree of prolapse determines the severity of symptoms and the impact on a woman’s quality of life.
RELATED: Peripheral Artery Disease: Early Signs and How to Seek Treatment
Prevalence
Cystoceles are a common condition, especially among older women. Studies suggest that about 40% of women will experience some form of pelvic organ prolapse in their lifetime, with the risk increasing with age. According to research, the proportion of women aged 70-79 seeking medical consultation due to symptomatic pelvic organ prolapse is as high as 18.6 per 1,000 women.
Factors such as vaginal childbirth, menopause, obesity, chronic constipation, and a family history of pelvic organ prolapse can increase the likelihood of developing a cystocele. As the population ages, the prevalence of this condition is expected to rise, making it crucial for women to be aware of the signs, symptoms, and available treatment options for a fallen bladder.
Symptoms of Cystocele
Common Signs
The symptoms of a cystocele can vary depending on its severity. In mild cases, a woman may not experience any noticeable signs or symptoms. However, as the condition progresses, she may begin to feel a sense of heaviness or fullness in her pelvis, as if something is falling out of her vagina. Other common symptoms include:
- Difficulty urinating, such as a slow or weak urine stream or the feeling that the bladder has not completely emptied
- Frequent urination or the urge to urinate more often than usual
- Stress incontinence, which is the leakage of urine during physical activity, coughing, sneezing, or laughing
- Pain or discomfort in the pelvis, lower back, or vagina
- A bulge or protrusion in the vagina that may be visible or palpable
- Painful sexual intercourse (dyspareunia)
These symptoms tend to worsen as the day progresses or after standing for long periods. They may also be more noticeable during bowel movements or physical exertion.
RELATED: Periodontal Disease (Gum Disease): Essential Tips for Oral Health Maintenance
When to See a Doctor
It is important for women to seek medical attention if they experience any symptoms of a cystocele, even if they are mild. Early diagnosis and treatment can prevent the condition from progressing and causing more serious complications. Women should consult their healthcare provider if they notice:
- A bulge or protrusion in the vagina
- Persistent discomfort or pain in the pelvis or vagina
- Difficulty urinating or a frequent urge to urinate
- Urinary incontinence or leakage
- Recurrent urinary tract infections
A doctor can perform a pelvic exam to diagnose a cystocele and determine its severity. They may also recommend additional tests, such as urodynamic studies or imaging scans, to assess bladder function and rule out other underlying conditions.
Prompt medical care is essential for women with severe cystoceles that cause significant pain, discomfort, or urinary problems. Left untreated, a severe cystocele can lead to chronic bladder infections, kidney damage, and a decreased quality of life. In such cases, surgery may be necessary to repair the weakened vaginal wall and restore normal bladder function.
Causes and Risk Factors
Weakening of Pelvic Floor Muscles
The pelvic floor muscles and connective tissues form a complex that supports the pelvic organs, including the bladder. Over time, these muscles and tissues can weaken or stretch, leading to a cystocele or fallen bladder. Factors such as pregnancy, childbirth, menopause, and aging contribute to the weakening of the pelvic floor muscles. As estrogen levels decrease during menopause, the muscles around the vagina lose strength, increasing the risk of developing a cystocele.
Pregnancy and Childbirth
Pregnancy and vaginal delivery are significant risk factors for developing a cystocele. The stress and strain on the pelvic floor muscles during pregnancy and the delivery process can cause damage to the supportive tissues. Multiple vaginal deliveries further increase the likelihood of experiencing a fallen bladder. Women who have given birth vaginally are at a higher risk compared to those who have had cesarean deliveries or have never been pregnant.
Other Contributing Factors
Several other factors can contribute to the development of a cystocele. These include:
- Chronic constipation or straining during bowel movements
- Repeated heavy lifting
- Obesity or being overweight
- Family history of pelvic organ prolapse
- Previous pelvic surgeries, such as a hysterectomy
- Connective tissue disorders, like Marfan syndrome or Ehlers-Danlos syndrome
Women with a combination of these risk factors are more likely to experience a fallen bladder. Maintaining a healthy weight, preventing constipation, and avoiding heavy lifting can help reduce the risk of developing a cystocele.
Diagnosis and Treatment Options
Physical Examination
Diagnosing a cystocele typically begins with a thorough pelvic examination. During this exam, the healthcare provider assesses the severity of the bladder prolapse by observing the degree of descent of the anterior vaginal wall while the patient is asked to strain or bear down. The provider may also check for any associated urinary incontinence or retention.
Imaging Tests
In some cases, imaging tests may be necessary to further evaluate the extent of the cystocele and its impact on bladder function. These tests may include:
- Pelvic ultrasound: This non-invasive test uses sound waves to create images of the pelvic organs, allowing the provider to visualize the position of the bladder and assess any abnormalities.
- Voiding cystourethrogram: This test involves taking X-ray images of the bladder and urethra during urination, which can help identify any obstruction or abnormal bladder emptying caused by the fallen bladder.
- Dynamic MRI: Magnetic resonance imaging (MRI) can provide detailed images of the pelvic floor muscles and organs, helping to evaluate the severity of the cystocele and its relationship to other pelvic structures.
Conservative Treatments
For mild to moderate cases of cystocele, conservative treatment options may be recommended before considering surgery. These may include:
- Pelvic floor exercises (Kegels): Regularly performing these exercises can help strengthen the muscles that support the bladder and other pelvic organs, potentially reducing the severity of the fallen bladder.
- Pessary: A pessary is a removable device inserted into the vagina to provide support for the prolapsed bladder. This can help alleviate symptoms and may be a good option for women who wish to avoid or delay surgery.
- Lifestyle modifications: Losing weight, avoiding heavy lifting, and treating chronic constipation can help reduce the pressure on the pelvic floor and may improve cystocele symptoms.
RELATED: How to Manage Panic Attacks & Panic Disorder Effectively
Surgical Interventions
In cases where conservative treatments are ineffective or the cystocele is severe, surgical intervention may be necessary. The goal of surgery is to repair the weakened vaginal wall and restore the bladder to its normal position. Common surgical procedures for cystocele include:
- Anterior colporrhaphy: This procedure involves making an incision in the vaginal wall and using stitches to reinforce the weakened tissue and support the bladder.
- Paravaginal repair: This surgery focuses on reattaching the lateral vaginal supports to the pelvic sidewall, helping to lift and support the bladder.
- Mesh implantation: In some cases, a surgical mesh may be used to provide additional support for the bladder. However, the use of mesh carries risks, such as erosion and infection, and should be carefully considered on a case-by-case basis.
The choice of surgical technique depends on factors such as the severity of the cystocele, the patient’s age, and any coexisting pelvic floor disorders. Discussing the potential benefits and risks of each option with a qualified healthcare provider is essential for making an informed decision about the best treatment approach for a fallen bladder.
Conclusion
A fallen bladder, or cystocele, has a significant impact on many women’s lives, particularly as they age. Understanding its symptoms, causes, and treatment options is crucial to improve quality of life and seek timely medical care. This condition, which results from weakened pelvic floor muscles, can cause discomfort and urinary problems, but various approaches exist to manage it effectively.
From conservative methods like pelvic floor exercises and pessaries to surgical interventions in severe cases, there are many ways to address a cystocele. By staying informed about risk factors and preventive measures, women can take steps to maintain their pelvic health. Remember, early detection and proper care are key to managing this common yet often overlooked condition, helping women to lead comfortable and active lives.