Calciphylaxis is a rare and severe condition that affects blood vessels in fatty and skin tissues. This painful disorder causes calcium deposits to form in small blood vessels, leading to skin ulcers, infections, and potentially life-threatening complications. Despite its rarity, calciphylaxis has a significant impact on those affected, making early detection and proper management crucial for improving outcomes.
Understanding the early signs, risk factors, and treatment options for calciphylaxis is essential for healthcare providers and patients alike. This article aims to explore the key aspects of calciphylaxis, including its initial symptoms, factors that increase the likelihood of developing the condition, and current approaches to diagnosis and treatment. By shedding light on this complex disorder, we hope to raise awareness and promote better recognition and care for those at risk or already affected by calciphylaxis.
Understanding Calciphylaxis



Definition and Overview
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare and potentially life-threatening condition characterized by the calcification of small blood vessels in the skin and subcutaneous tissue. This calcification leads to the development of painful, ischemic skin lesions that can progress to non-healing ulcers and necrosis. While calciphylaxis most commonly affects individuals with end-stage renal disease, it can also occur in patients with normal kidney function.
Pathophysiology
The exact pathophysiology of calciphylaxis remains unclear, but several factors are thought to contribute to its development. The primary mechanism involves the calcification of the medial layer of small arterioles, leading to vascular occlusion and tissue ischemia. This calcification process is believed to be triggered by an imbalance in calcium and phosphate metabolism, often associated with secondary hyperparathyroidism in patients with chronic kidney disease. Other proposed mechanisms include endothelial dysfunction, inflammation, and a hypercoagulable state.
RELATED: Ocular Migraine Relief: Proven Methods and Treatments
Types of Calciphylaxis
Calciphylaxis can be classified into two main types: uremic and non-uremic. Uremic calciphylaxis, the more common type, occurs in patients with end-stage renal disease and is associated with abnormalities in calcium and phosphate metabolism. Non-uremic calciphylaxis, on the other hand, develops in individuals with normal kidney function and may be associated with underlying conditions such as autoimmune disorders, malignancies, or hyperparathyroidism. Recognizing the different types of calciphylaxis is crucial for determining the appropriate diagnostic approach and treatment strategies.
Early Signs and Symptoms
Skin Changes
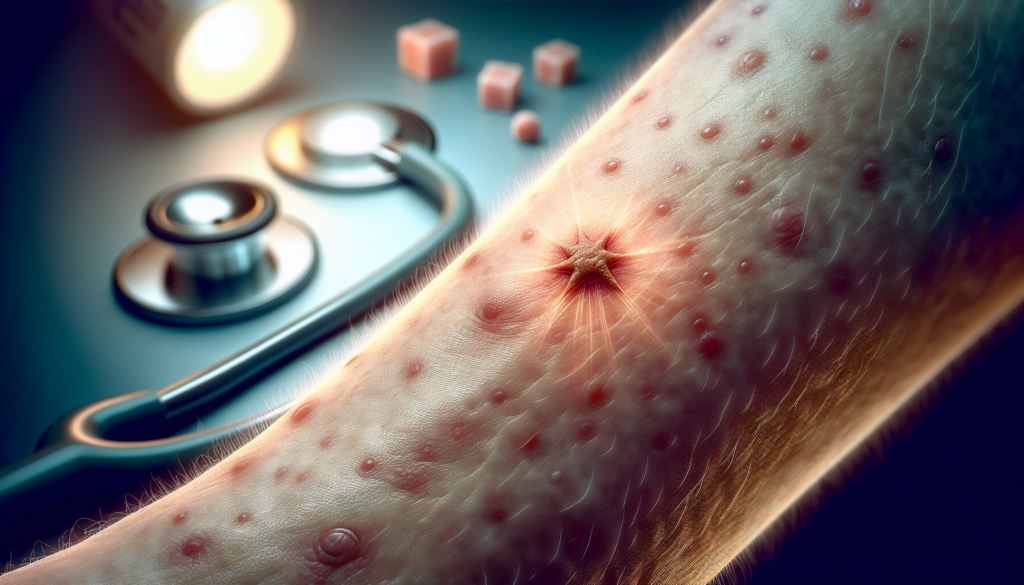
The initial signs of calciphylaxis often involve subtle changes in the skin. Patients may notice localized areas of erythema, purpura, or livedo reticularis, which are characterized by a mottled, netlike pattern on the skin. These skin changes can be easily overlooked or mistaken for other dermatological conditions, leading to a delay in diagnosis. As the disease progresses, the affected areas may develop into painful, indurated plaques or nodules, signaling the onset of more severe skin manifestations.
Pain and Discomfort
One of the hallmark features of calciphylaxis is the presence of severe, intractable pain that often precedes the appearance of visible skin lesions. Patients may experience a burning, stinging, or deep aching sensation in the affected areas, which can be disproportionate to the extent of the skin changes. This pain can be debilitating and significantly impact the patient’s quality of life. The intensity of the pain may serve as an important clue to suspect calciphylaxis, especially in high-risk individuals such as those with end-stage renal disease or on long-term dialysis.
Systemic Symptoms
In addition to the localized skin manifestations, patients with calciphylaxis may experience systemic symptoms that can provide valuable diagnostic clues. These symptoms may include fatigue, weakness, fever, and general malaise. Some patients may also have signs of underlying inflammation, such as elevated levels of C-reactive protein or erythrocyte sedimentation rate. The presence of these systemic symptoms, in combination with the characteristic skin changes and risk factors, should prompt a high index of suspicion for calciphylaxis and trigger further diagnostic evaluation.
Risk Factors and Causes
Kidney Disease-Related Factors
Calciphylaxis is most commonly associated with end-stage renal disease and dialysis treatment. Abnormalities in mineral metabolism, such as hyperphosphatemia, hypercalcemia, and secondary hyperparathyroidism, are prevalent in patients with chronic kidney disease and are thought to contribute to the development of calciphylaxis. The use of calcium-based phosphate binders and vitamin D analogs in the management of these abnormalities may further increase the risk. Additionally, longer dialysis vintage, typically over 6-7 years, has been identified as a potential risk factor for calciphylaxis in patients with kidney disease.
Non-Renal Risk Factors
Although calciphylaxis predominantly affects individuals with advanced kidney disease, it can also occur in patients with normal renal function or earlier stages of chronic kidney disease. In these cases, other underlying conditions may play a role in the pathogenesis of calciphylaxis. Obesity, particularly in the setting of rapid weight loss, has been associated with the development of calciphylaxis, possibly due to increased stress on dermal arterioles in expanded subcutaneous adipose tissue. Autoimmune disorders, such as systemic lupus erythematosus and rheumatoid arthritis, as well as hypercoagulable states, including protein C and S deficiencies and antiphospholipid antibody syndrome, have also been implicated in the development of calciphylaxis. Certain medications, particularly warfarin, corticosteroids, and iron compounds, have been identified as potential triggers for calciphylaxis in both uremic and non-uremic patients.
RELATED: Top Treatments for Occipital Neuralgia: A Complete Guide
Genetic Predisposition
While the exact role of genetic factors in calciphylaxis remains unclear, some evidence suggests that genetic predisposition may contribute to an individual’s risk of developing this condition. Polymorphisms in genes involved in the regulation of extraskeletal calcification, such as matrix Gla protein and fetuin-A, have been proposed as potential genetic risk factors for calciphylaxis. However, further research is needed to elucidate the specific genetic mechanisms underlying the development of calciphylaxis and to identify individuals who may be at increased risk based on their genetic profile. As our understanding of the genetic basis of calciphylaxis evolves, it may become possible to develop targeted preventive strategies for high-risk individuals.
Diagnosis and Treatment Options
Diagnostic Methods
Accurately diagnosing calciphylaxis requires a comprehensive evaluation. A thorough physical examination to identify skin lesions and assess pain levels is essential. Laboratory tests, including renal function tests, mineral bone parameters, liver function tests, and inflammatory markers, can provide valuable diagnostic clues. Radiological imaging, such as plain X-rays and nuclear bone scans, may demonstrate calcium deposits in blood vessels but are not routinely recommended for diagnosis. The gold standard for confirming calciphylaxis is a skin biopsy, which typically reveals calcification, microthrombosis, and fibrointimal hyperplasia of small dermal and subcutaneous arteries and arterioles. Special stains like von Kossa or Alizarin red can enhance the detection of calcium deposits. However, skin biopsies carry risks of ulceration, infection, and lesion propagation, so careful consideration of the risk-benefit ratio is necessary.
Medical Interventions
Treatment of calciphylaxis involves a multifaceted approach. Normalizing serum calcium and phosphorous levels, maintaining parathyroid hormone levels between 150-300 ng/mL, and avoiding calcium supplements, vitamin D analogues, and calcium-based phosphate binders are crucial. Cinacalcet is preferred over surgical parathyroidectomy for managing secondary hyperparathyroidism. Sodium thiosulfate, administered intravenously, is frequently used off-label for its potential to chelate calcium and restore endothelial function. Antibiotic therapy is indicated for infected lesions, while aggressive pain management often requires potent analgesics like fentanyl patches or narcotic medications. Nutrition consultation to address protein-energy malnutrition and optimization of dialysis prescription are also important supportive measures.
RELATED: Neurofibromatosis: A Detailed Look at Symptoms and Treatments
Surgical Approaches
Surgical debridement of necrotic ulcers is often necessary to preserve surrounding tissue and prevent sepsis. Deep ulcer shaving combined with split-thickness skin grafting has shown promise in promoting wound healing and reducing pain. However, the decision to perform surgical debridement should be made on a case-by-case basis, considering factors such as wound infection, tissue involvement, and patient comorbidities. Hyperbaric oxygen therapy may be considered as a second-line treatment for recalcitrant wounds, although its efficacy remains controversial.
Emerging Therapies
Several novel therapies are being explored for calciphylaxis treatment. Intravenous bisphosphonates, low-dose tissue plasminogen activator infusions, LDL-apheresis, and vitamin K supplementation have shown potential benefits in case reports and small case series. SNF472, an intravenous formulation that inhibits hydroxyapatite crystal formation, has demonstrated improved wound healing, pain control, and quality of life in a recent open-label trial. However, larger prospective studies are needed to validate the efficacy and safety of these emerging therapies before they can be widely recommended for clinical use.
Conclusion
Calciphylaxis remains a challenging condition with severe consequences for those affected. This article has shed light on its early signs, risk factors, and current treatment approaches. Understanding these aspects is crucial to improve early detection and management. The complex interplay of factors contributing to calciphylaxis underscores the need for a multidisciplinary approach to care, involving nephrologists, dermatologists, and wound care specialists.
Looking ahead, ongoing research into new therapies offers hope for better outcomes. While current treatments can help manage symptoms, more effective interventions are needed to address the underlying causes of calciphylaxis. Continued efforts to raise awareness among healthcare providers and at-risk patients are essential to enhance early diagnosis and improve the quality of life for those living with this rare but serious condition.