Candida albicans, a common yeast found naturally in the human body, can sometimes cause trouble when it grows out of control. This microscopic organism typically lives harmlessly in our gut, mouth, and skin, but certain conditions can lead to its overgrowth, resulting in various health issues. Understanding Candida albicans and its potential effects on our well-being is crucial for maintaining overall health and seeking appropriate treatment when needed.
This article delves into the world of Candida albicans, exploring its nature, symptoms of overgrowth, and risk factors that can contribute to infections. We’ll also discuss how healthcare professionals diagnose Candida-related problems and the available treatment options. By the end, readers will have a better grasp of this often misunderstood organism and be better equipped to recognize and address potential Candida-related health concerns.
What is Candida Albicans?
Definition and characteristics
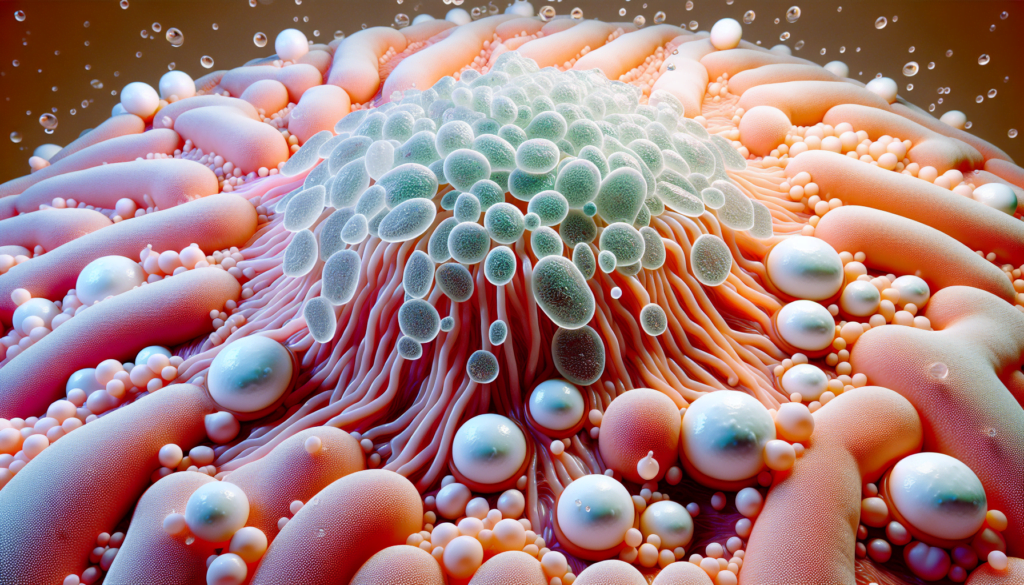
Candida albicans is a species of yeast that belongs to the genus Candida. It is a dimorphic fungus, meaning it can exist in two forms: as oval-shaped yeast cells or as filamentous hyphae. The ability to switch between these two forms is a crucial factor in its pathogenicity. Candida albicans is characterized by its white color when cultured on a plate, which is reflected in its name – “albicans” comes from the Latin word for “white.”
Natural occurrence in the body
Candida albicans is a commensal organism, naturally residing in the gastrointestinal tract, oral cavity, and vagina of healthy individuals. It is part of the normal human microbiota and is present in approximately 40-60% of healthy adults. In a balanced state, Candida albicans coexists harmoniously with other microorganisms without causing any harm to the host.
The gastrointestinal tract serves as the primary reservoir for Candida albicans in the body. The fungus colonizes the mucosal surfaces of the mouth, esophagus, and intestines, where it adheres to epithelial cells. In the vagina, Candida albicans is kept in check by the presence of beneficial lactobacilli bacteria, which maintain an acidic environment that prevents overgrowth.
RELATED: A Complete Overview of Non-Hodgkin Lymphoma: From Causes to Treatments
When Candida becomes problematic
Under certain conditions, the delicate balance between Candida albicans and the host can be disrupted, leading to an overgrowth of the fungus. This overgrowth can result in various clinical manifestations, ranging from superficial mucosal infections to life-threatening systemic diseases.
Several factors can contribute to the transition of Candida albicans from a commensal to a pathogenic organism. These include:
- Immunosuppression: Individuals with weakened immune systems, such as those undergoing chemotherapy, organ transplant recipients, or people with HIV/AIDS, are more susceptible to Candida infections.
- Antibiotic use: Prolonged or broad-spectrum antibiotic therapy can disrupt the normal bacterial flora, allowing Candida albicans to proliferate unchecked.
- Hormonal changes: Pregnancy, oral contraceptives, and hormone replacement therapy can alter the vaginal environment, favoring the growth of Candida.
- Diabetes: Poorly controlled diabetes can lead to increased glucose levels in the body, providing a favorable environment for Candida growth.
- Mucosal damage: Trauma to the mucosal barriers, such as from dental procedures, surgery, or the use of catheters, can facilitate the invasion of Candida into the bloodstream.
When Candida albicans overgrows and invades host tissues, it can cause a range of infections collectively known as candidiasis. These infections can affect various body sites, including the oral cavity (thrush), the vagina (vulvovaginal candidiasis), the skin (cutaneous candidiasis), and in severe cases, the bloodstream and internal organs (invasive candidiasis).
The pathogenicity of Candida albicans is attributed to its virulence factors, such as the ability to adhere to host cells, secrete hydrolytic enzymes, and form biofilms. These factors enable the fungus to evade the host’s immune defenses and establish infection.
Common Symptoms of Candida Overgrowth
When candida albicans grows out of control, it can cause various symptoms depending on the location of the infection. Some of the most common signs and symptoms associated with candida overgrowth include:
Oral thrush
Oral thrush is a type of candida infection that affects the mouth and throat. It is characterized by the appearance of white, slightly raised lesions on the tongue, inner cheeks, gums, or back of the throat. These lesions may cause discomfort, pain, or a burning sensation, especially when eating or swallowing. In some cases, the lesions may bleed slightly when scraped. Infants, elderly individuals, and those with weakened immune systems are more susceptible to developing oral thrush.
Genital yeast infections
Candida albicans is a common cause of genital yeast infections, particularly in women. Symptoms of a vaginal yeast infection include intense itching, burning, and irritation in the vaginal area. The vulva may appear red and swollen, and there may be a thick, white, cottage cheese-like discharge. Pain or discomfort during sexual intercourse and urination is also common. Men can develop genital yeast infections as well, although less frequently than women. Symptoms in men may include a red, itchy rash on the penis, along with burning and irritation.
RELATED: What is Neurofibroma? A Complete Guide to Symptoms and Treatment
Digestive issues
An overgrowth of candida albicans in the gut can lead to various digestive symptoms. These may include bloating, gas, abdominal pain, diarrhea, and constipation. Some individuals may also experience nausea, vomiting, and a feeling of fullness or discomfort after eating. Candida overgrowth in the gut can disrupt the balance of beneficial bacteria, leading to digestive disturbances and potentially contributing to the development of leaky gut syndrome.
Skin and nail infections
Candida albicans can cause infections on the skin and nails, particularly in warm, moist areas such as the armpits, groin, and skin folds. Symptoms of a skin infection may include a red, itchy rash with small, raised bumps or blisters. The affected skin may be painful, and there may be a burning sensation. Nail infections caused by candida can result in thickened, discolored, or brittle nails that may separate from the nail bed. These infections are more common in individuals with compromised immune systems or those who frequently have their hands in water.
It is important to note that the symptoms of candida overgrowth can vary from person to person and may resemble those of other conditions. If you suspect that you have a candida infection, it is essential to consult with a healthcare professional for an accurate diagnosis and appropriate treatment. Antifungal medications, along with lifestyle and dietary changes, can help restore the balance of candida in the body and alleviate symptoms.
Risk Factors for Candida Infections
Weakened immune system
A weakened immune system is one of the primary risk factors for developing candida infections. Individuals with compromised immunity, such as those undergoing chemotherapy, organ transplant recipients, or people with HIV/AIDS, are more susceptible to candida albicans overgrowth. The immune system plays a crucial role in keeping candida albicans in check, and when it is not functioning optimally, the fungus can proliferate unchecked, leading to various forms of candidiasis.
In patients with diabetes, the immune response is impaired, making them more prone to candida infections. Poorly controlled diabetes can lead to increased glucose levels in the body, providing a favorable environment for candida growth. Additionally, diabetes can cause microvascular degeneration and impaired candidacidal activity of neutrophils, further compromising the body’s ability to fight off candida albicans.
Antibiotic use
Prolonged or broad-spectrum antibiotic therapy is another significant risk factor for candida infections. Antibiotics disrupt the normal bacterial flora in the body, allowing candida albicans to proliferate unchecked. The delicate balance between beneficial bacteria and candida is essential for maintaining a healthy microbiome. When this balance is disrupted, candida can overgrow and cause infections.
Antibiotics are often prescribed to treat bacterial infections, but they can also eliminate the beneficial bacteria that help keep candida albicans in check. This is particularly true for broad-spectrum antibiotics, which target a wide range of bacteria. As a result, individuals who have recently taken antibiotics or are on long-term antibiotic therapy are at a higher risk of developing candida infections.
Diabetes
Diabetes is a significant risk factor for candida infections, particularly in individuals with poorly controlled blood sugar levels. High glucose levels in the body provide an ideal environment for candida albicans to thrive. In addition, diabetes can lead to impaired immune function, making it harder for the body to fight off candida infections.
Individuals with diabetes are more likely to develop oral thrush, genital yeast infections, and skin and nail infections caused by candida albicans. Poorly controlled diabetes can also lead to increased glycogen levels, a polysaccharide that the body uses to store glucose. Extra glycogen in the vaginal area can contribute to yeast growth and increase the risk of vaginal candidiasis.
Hormonal changes
Hormonal changes, particularly those associated with pregnancy, oral contraceptives, and hormone replacement therapy, can increase the risk of candida infections, especially vaginal candidiasis. Estrogen promotes glycogen production at the vaginal mucosa, providing a nutrient-rich environment for candida albicans to grow.
During pregnancy, elevated estrogen levels can lead to an increased risk of vaginal yeast infections. Similarly, women taking high-estrogen-containing oral contraceptives or undergoing hormone replacement therapy are more susceptible to candida overgrowth. These hormonal changes can alter the vaginal environment, favoring the growth of candida albicans and increasing the likelihood of infection.
In conclusion, several risk factors contribute to the development of candida infections, with a weakened immune system, antibiotic use, diabetes, and hormonal changes being among the most significant. Understanding these risk factors is crucial for preventing and managing candida infections, particularly in vulnerable populations. By addressing underlying health conditions, minimizing antibiotic use when possible, and maintaining good hygiene practices, individuals can reduce their risk of developing candida infections caused by candida albicans overgrowth.
Diagnosis and Treatment Options
Diagnostic methods
Diagnosing candida albicans infections involves various methods depending on the location and severity of the infection. For oral thrush, healthcare providers can usually diagnose the condition by examining the mouth and throat. In some cases, they may take a small sample from the affected area for testing. Vaginal yeast infections are diagnosed based on a lab culture of a vaginal discharge sample. Candidiasis of the esophagus requires an endoscopy, a procedure that uses a tube with a light and camera to examine the digestive tract. For invasive candidiasis, blood tests are the primary diagnostic tool. Healthcare providers rely on the patient’s medical history, symptoms, physical examinations, and laboratory tests to diagnose this severe form of candida albicans infection. The most common way to test for invasive candidiasis is by taking a blood sample or a sample from the infected body site and sending it to a laboratory for a fungal culture.
Antifungal medications
Antifungal medications are the standard treatment for candida albicans infections. These medications come in various forms, including creams, oral gels, pills, and intravenous (IV) solutions. The type of antifungal, dose, and length of treatment depend on the type and severity of the infection, as well as the patient’s overall health. For vaginal yeast infections, treatment usually involves an antifungal cream applied inside the vagina or a single dose of fluconazole taken orally. In more severe cases, additional doses of fluconazole or other medications may be prescribed. Oral thrush is typically treated with an antifungal oral gel applied inside the mouth for 7-14 days. Severe cases may require antifungal medication in pill form or through an IV. Candidiasis of the esophagus is almost always treated with fluconazole, either in pill form or through an IV. Invasive candidiasis requires intensive treatment with IV antifungal medications, such as echinocandins or amphotericin B. The length of treatment for invasive candidiasis depends on the location and severity of the infection, ranging from several weeks to several months.
RELATED: Nasal Polyps Explained: Symptoms, Causes, and Treatment Options
Natural remedies
While there is limited scientific evidence supporting the use of natural remedies for candida albicans infections, some individuals may find relief from certain dietary and lifestyle changes. These changes include restricting foods high in sugar and yeast, managing stress, and taking probiotics to support a healthy balance of gut bacteria. However, it is essential to note that natural remedies should not replace medical treatment for candida albicans infections, particularly in severe cases. Consulting with a healthcare provider is crucial to ensure proper diagnosis and treatment.
Lifestyle changes
In addition to medical treatment, making certain lifestyle changes can help prevent and manage candida albicans infections. Maintaining good hygiene, particularly in the genital area, is essential. This includes wearing breathable, cotton underwear, changing out of wet swimsuits or sweaty clothing promptly, and wiping from front to back after using the bathroom. Avoiding douches, perfumed sprays, and scented tampons can also help maintain a healthy balance of bacteria in the vaginal area. For individuals with diabetes, keeping blood sugar levels under control is crucial, as high blood sugar can contribute to the growth of candida albicans. Quitting smoking and reducing alcohol consumption may also help prevent candida albicans infections, as these habits can weaken the immune system and disrupt the balance of bacteria in the body.
Conclusion
Understanding Candida albicans and its potential effects has a significant impact on maintaining overall health. This common yeast, normally harmless, can cause trouble when it grows out of control, leading to various infections. Recognizing the symptoms, risk factors, and available treatments empowers individuals to address potential Candida-related health concerns effectively. By staying informed, people can work with healthcare providers to manage or prevent Candida overgrowth.
To wrap up, Candida albicans is a complex organism that plays a role in our body’s delicate balance. While it can cause problems, there are ways to manage and treat Candida-related issues. By making smart lifestyle choices, seeking timely medical attention, and following prescribed treatments, individuals can keep Candida in check and maintain their well-being. This knowledge serves as a valuable tool to make informed decisions about one’s health.