Myelofibrosis is a rare but serious bone marrow disorder that affects thousands of people worldwide. This condition disrupts the normal production of blood cells, leading to a range of health issues. Understanding myelofibrosis symptoms and available treatments is crucial for patients and their loved ones to manage this challenging disease effectively.
This article aims to shed light on the key aspects of myelofibrosis. It will explain what myelofibrosis is, describe its common symptoms, and explore the diagnostic process. Additionally, it will delve into current treatment strategies, providing readers with a comprehensive overview of this complex condition. By the end, readers will have a better grasp of myelofibrosis and the options available to address its impact on health and quality of life.
Myelofibrosis: An Overview
Definition and Classification
Myelofibrosis is a rare bone marrow disorder characterized by the abnormal proliferation of blood cells and the formation of fibrous tissue in the bone marrow. It belongs to a group of diseases known as myeloproliferative neoplasms (MPNs), which are blood cancers that involve the overproduction of one or more types of blood cells. Myelofibrosis can be classified as primary myelofibrosis (PMF) when it arises on its own, or as secondary myelofibrosis when it develops as a progression of other MPNs such as polycythemia vera (post-PV-MF) or essential thrombocythemia (post-ET-MF).
Epidemiology
The worldwide annual incidence of myelofibrosis is estimated to be around 0.47 cases per 100,000 people, with variations depending on geographic location. In the United States, the incidence rate of primary myelofibrosis is approximately 0.44 per 100,000 person-years. Myelofibrosis typically affects individuals over 50 years of age, with a median age at diagnosis of around 65 years. When it occurs in children, it usually manifests before the age of 3, with girls being affected twice as often as boys.
RELATED: Hepatitis A: Everything You Need to Know About HAV
Pathophysiology
The exact cause of myelofibrosis remains unknown, but several genetic mutations have been identified in patients with this condition. Approximately 50-60% of individuals with myelofibrosis have a mutation in the JAK2 gene, which plays a role in the regulation of blood cell production. Other mutations, such as those in the CALR and MPL genes, have also been associated with myelofibrosis. These genetic alterations lead to the abnormal proliferation of blood cells and the release of cytokines that stimulate the formation of fibrous tissue in the bone marrow, disrupting normal blood cell production.
Clinical Presentation of Myelofibrosis
Hematological Manifestations
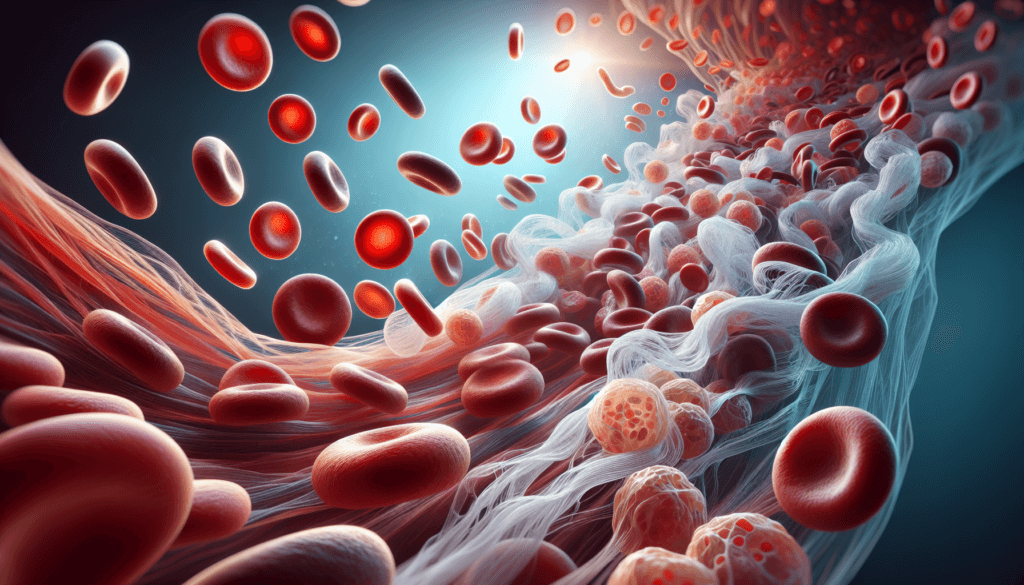
Myelofibrosis often leads to a range of hematological abnormalities. Anemia is a common finding, resulting from the disruption of normal red blood cell production in the fibrotic bone marrow. The red blood cells that are produced may be misshapen or immature, a condition known as poikilocytosis. In addition to anemia, patients with myelofibrosis may exhibit variable numbers of white blood cells and platelets. As the disease progresses, the platelet count typically decreases, leading to thrombocytopenia. The presence of immature white blood cells and platelets in the peripheral blood, known as leukoerythroblastosis, is another characteristic hematological feature of myelofibrosis.
Systemic Symptoms
The clinical presentation of myelofibrosis extends beyond the hematological manifestations. Patients often experience a constellation of systemic symptoms that can significantly impact their quality of life. Fatigue and weakness are prevalent complaints, primarily due to the underlying anemia. Night sweats, fever, and weight loss, collectively referred to as constitutional symptoms, are also frequently reported. These symptoms are thought to be mediated by the release of inflammatory cytokines from the abnormal clonal cells. Bone pain, particularly in the extremities, is another common symptom that may be attributed to the expansion of hematopoietic tissue within the bone marrow cavity.
RELATED: Hyponatremia: Low Sodium Levels and Their Impact on Health
Organ Involvement
As myelofibrosis progresses, the involvement of extramedullary organs becomes increasingly evident. Splenomegaly, or enlargement of the spleen, is a hallmark feature of the disease. The spleen takes over the role of hematopoiesis as the bone marrow becomes increasingly fibrotic, leading to its progressive enlargement. Hepatomegaly, or enlargement of the liver, may also occur due to extramedullary hematopoiesis. In advanced stages, patients may develop portal hypertension, a complication resulting from the increased blood flow through the spleen and liver. This can manifest as abdominal pain, ascites, and esophageal varices. The infiltration of other organs, such as the lungs, by extramedullary hematopoietic tissue can lead to respiratory symptoms and pulmonary hypertension in some cases.
Diagnostic Approach to Myelofibrosis
Clinical Evaluation
The diagnosis of myelofibrosis begins with a thorough clinical evaluation. A detailed medical history should be obtained, focusing on cardiovascular risk factors, past illnesses and injuries, current and past medications, history of thrombosis or hemorrhagic events, family medical history, and current symptoms. The physical examination includes assessment of vital signs, lymph nodes, spleen, and abdomen. Splenomegaly is a hallmark feature of myelofibrosis and is often palpable on examination.
Laboratory Investigations
A complete blood count with differential is essential in the diagnostic workup of myelofibrosis. Patients often present with anemia, leukocytosis or leukopenia, and abnormal platelet counts. A peripheral blood smear may reveal abnormal teardrop-shaped red blood cells and immature blasts. Blood chemistry profile can show elevated serum levels of uric acid, lactate dehydrogenase, alkaline phosphatase, and bilirubin. Molecular testing for JAK2, CALR, and MPL mutations is crucial for diagnosis and treatment planning. These mutations are present in approximately 90% of patients with myelofibrosis. In the absence of these mutations, the presence of other clonal markers or the absence of reactive myelofibrosis supports the diagnosis.
Histopathological Assessment
Bone marrow examination, including aspiration and biopsy, is essential for confirming the diagnosis of myelofibrosis. The bone marrow typically shows increased numbers of megakaryocytes with unusual size and shape, and there is often significant scarring (fibrosis) of the bone marrow. The degree of fibrosis is graded using reticulin and collagen staining. In early stages of myelofibrosis, the bone marrow may show only mild reticulin fibrosis, while advanced stages demonstrate dense collagen fibrosis and osteosclerosis. The World Health Organization provides specific diagnostic criteria for myelofibrosis, which include a combination of major and minor criteria based on bone marrow morphology, molecular genetics, and clinical features.
Comprehensive Treatment Strategies
Myelofibrosis treatment has seen significant advancements in recent years, with a focus on risk-adapted therapy tailored to each patient’s specific needs. The Dynamic International Prognostic Scoring System (DIPSS-Plus) is used to stratify patients into low, intermediate-1, intermediate-2, and high-risk categories, guiding treatment decisions. For low-risk patients, a watch-and-wait approach may be appropriate, while intermediate and high-risk patients often require more aggressive interventions.
Symptom management is a crucial aspect of myelofibrosis care, as the disease can cause debilitating symptoms such as fatigue, night sweats, and bone pain. JAK inhibitors, particularly ruxolitinib, have revolutionized symptom control by targeting the overactive JAK-STAT pathway. These medications can significantly reduce spleen size and improve quality of life. Other supportive measures include blood transfusions for anemia, radiation therapy for localized bone pain, and medications for itching and other constitutional symptoms.
RELATED: Hyperpigmentation: Common Causes and How to Treat It
While most myelofibrosis treatments are palliative, allogeneic stem cell transplantation remains the only potentially curative option. However, this procedure carries significant risks and is typically reserved for younger, fit patients with high-risk disease. Reduced-intensity conditioning regimens have expanded the eligibility criteria for transplantation, but careful patient selection is essential to balance the potential benefits and risks.
Follow-up care is vital for monitoring treatment response, managing side effects, and detecting disease progression. Regular check-ups should include physical exams, blood counts, and assessment of symptom burden using tools like the Myeloproliferative Neoplasm Symptom Assessment Form (MPN-SAF). Bone marrow biopsies may be performed periodically to evaluate fibrosis and blast percentage. Patients should also be educated about the signs and symptoms of disease progression and encouraged to report any new or worsening symptoms promptly.
As researchers continue to unravel the complex pathogenesis of myelofibrosis, novel targeted therapies are emerging that hold promise for improved outcomes. These include telomerase inhibitors, epigenetic modifiers, and combination approaches that aim to disrupt multiple pathways involved in disease progression. Ongoing clinical trials are evaluating the safety and efficacy of these innovative strategies, offering hope for patients with this challenging condition.
Conclusion
Myelofibrosis presents a complex challenge for patients and healthcare providers alike. The condition has a significant impact on blood cell production and overall health, leading to a range of symptoms that can greatly affect quality of life. Understanding the signs, diagnostic process, and available treatments is crucial to manage this rare but serious bone marrow disorder effectively. As research continues, new therapies and approaches are emerging, offering hope to improve outcomes and ease the burden of myelofibrosis.
For those dealing with myelofibrosis, a team approach involving hematologists, oncologists, and supportive care specialists is key to provide comprehensive care. Regular check-ups, symptom management, and staying informed about new developments in treatment options are essential steps to take. While myelofibrosis remains a challenging condition, ongoing advancements in medical science are paving the way for better management strategies and potentially more effective treatments in the future.