Meralgia paresthetica is a condition that causes numbness, tingling, and burning pain in the outer thigh. This uncomfortable sensation has an impact on daily activities and quality of life for many individuals. Understanding meralgia paresthetica treatment options is crucial for those seeking relief from its symptoms and to regain normal function.
This article explores expert tips and advice to manage meralgia paresthetica effectively. It delves into the causes and symptoms of the condition, discusses diagnostic methods, and outlines various conservative treatment approaches. Additionally, it examines when surgery might be necessary and provides insights to help individuals make informed decisions about their care. By the end, readers will have a comprehensive understanding of how to address this challenging condition.
Understanding Meralgia Paresthetica
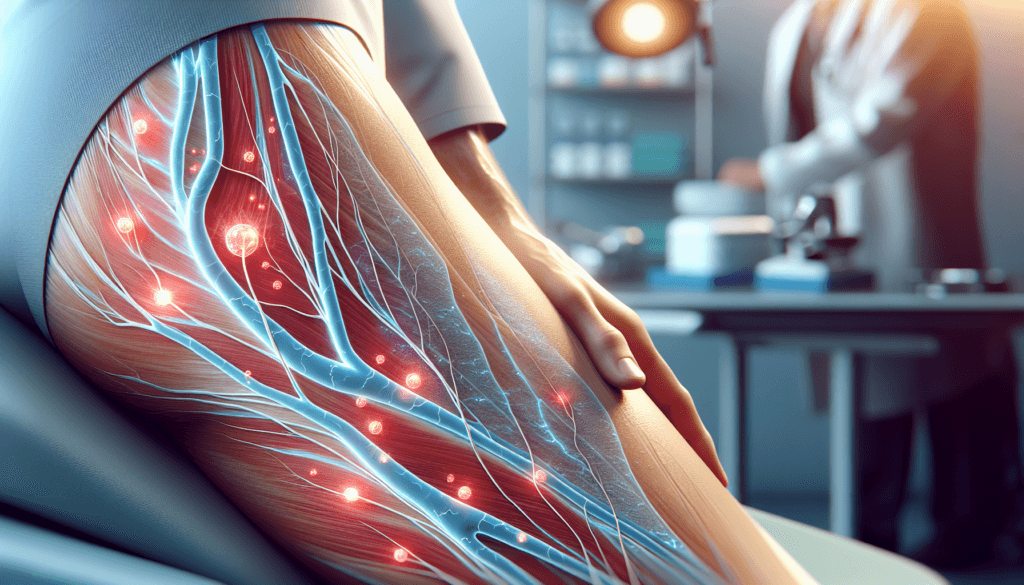
Meralgia paresthetica is a condition that causes numbness, pain, or a burning sensation in the outer thigh due to compression of the lateral femoral cutaneous nerve (LFCN). This nerve provides sensation to the front and side of the thigh. Understanding the symptoms, causes, and risk factors of meralgia paresthetica is essential for effective treatment and management.
Symptoms
The primary symptoms of meralgia paresthetica include pain, tingling, numbness, or burning in the outside of the thigh. These sensations are usually present on only one side of the body. Individuals may experience increased sensitivity to light touch rather than firm pressure and heightened sensitivity to heat. Symptoms may worsen after walking or standing for extended periods. As the condition progresses, the pain may become sharper and more intense, with intermittent periods of relief.
RELATED: Epstein-Barr Virus: How It Affects Your Health and Treatment Options
Causes
Meralgia paresthetica occurs when the LFCN becomes compressed or damaged due to insufficient space to pass through the hip bone or joints. This compression can result from various factors, including swelling, trauma, or increased pressure in the area. Common causes include weight gain, obesity, tight clothing, pregnancy, injury, wearing heavy items around the waist, diseases that damage nerves like diabetes, repetitive motions that irritate the nerve, and prolonged standing or walking.
Risk Factors
Several factors increase the risk of developing meralgia paresthetica. These include being overweight, pregnant, or having certain medical conditions such as diabetes, hypothyroidism, and alcoholism. Individuals between the ages of 30 and 60 are more susceptible to the condition. Exposure to lead-based paint, having legs of different lengths, and engaging in activities that put pressure on the LFCN also elevate the risk of meralgia paresthetica.
By recognizing the symptoms, causes, and risk factors associated with meralgia paresthetica, individuals can seek appropriate treatment options and make necessary lifestyle modifications to alleviate their discomfort. Consulting with a healthcare professional is crucial for an accurate diagnosis and the development of a personalized treatment plan to address this challenging condition effectively.
Diagnosing Meralgia Paresthetica
Meralgia paresthetica is primarily diagnosed based on a patient’s history and physical examination findings. The key is to identify the characteristic symptoms of pain, numbness, tingling or burning sensations in the outer thigh region, without any associated motor deficits or abnormal reflexes.
Physical Examination
During the physical exam, the healthcare provider will assess the area of altered sensation, typically over the anterolateral thigh. Palpation near the anterior superior iliac spine may elicit a positive Tinel’s sign, indicating irritation of the lateral femoral cutaneous nerve. The pelvic compression test, where pressure is applied to the patient’s pelvis for about 45 seconds, can help confirm the diagnosis if symptoms improve during the maneuver. A thorough neurological examination is essential to rule out other conditions that may mimic meralgia paresthetica, such as lumbar radiculopathy or plexopathy.
RELATED: Epididymitis: Detailed Insights on Causes, Symptoms, and Treatments
Diagnostic Tests
While the diagnosis of meralgia paresthetica is mainly clinical, certain diagnostic tests may be considered in some cases. Nerve conduction studies can assess the function of the lateral femoral cutaneous nerve but are often challenging to perform, especially in overweight individuals. Imaging studies like pelvic radiographs, ultrasound, or MRI may be indicated if a pelvic tumor or other underlying pathology is suspected. Injecting a local anesthetic near the lateral femoral cutaneous nerve can temporarily relieve symptoms and support the diagnosis of meralgia paresthetica. Blood tests may be ordered if a metabolic cause, such as diabetes or hypothyroidism, is being considered.
Conservative Treatment Options
Conservative treatment options for meralgia paresthetica focus on reducing pressure on the lateral femoral cutaneous nerve to alleviate symptoms. These approaches include lifestyle changes, physical therapy, and medications. By implementing these strategies, individuals can effectively manage their condition and improve their quality of life without resorting to invasive procedures.
Lifestyle Changes
Making simple lifestyle modifications can have a significant impact on relieving the symptoms of meralgia paresthetica. Losing excess weight, if applicable, can reduce pressure on the affected nerve. Wearing loose-fitting clothing and avoiding tight belts or garments that compress the waist and hip area can also provide relief. Additionally, maintaining good posture and avoiding prolonged periods of standing or sitting can help minimize pressure on the nerve.
Physical Therapy
Physical therapy plays a crucial role in treating meralgia paresthetica. Stretching and strengthening exercises targeting the muscles in the pelvis and thighs can help release the compressed nerve and alleviate symptoms. A physical therapist can develop a personalized exercise program that includes stretches for the hip flexors, quadriceps, and hamstrings, as well as core strengthening exercises. Techniques such as manual therapy, ultrasound, and electrical stimulation may also be used to reduce pain and inflammation.
Medications
In some cases, medications may be necessary to manage the pain and discomfort associated with meralgia paresthetica. Over-the-counter pain relievers like acetaminophen or ibuprofen can help alleviate mild to moderate pain. For more severe cases, prescription medications such as gabapentin, pregabalin, or tricyclic antidepressants may be recommended to reduce neuropathic pain. Topical creams or patches containing lidocaine or capsaicin can also provide localized pain relief. In certain situations, corticosteroid injections near the affected nerve may be considered to reduce inflammation and provide temporary symptom relief.
By implementing a combination of lifestyle changes, physical therapy, and appropriate medications, individuals with meralgia paresthetica can effectively manage their symptoms and improve their overall functioning. It is essential to work closely with a healthcare professional to develop a personalized treatment plan that addresses the specific needs and severity of each individual’s condition. With proper conservative management, most people with meralgia paresthetica can find relief from their symptoms and regain their quality of life.
When to Consider Surgery
In cases where conservative treatment measures fail to provide adequate relief from the symptoms of meralgia paresthetica, surgical intervention may be necessary. The decision to proceed with surgery depends on the severity and duration of the symptoms, as well as their impact on the individual’s quality of life. If pain, numbness, and tingling sensations persist despite lifestyle modifications, physical therapy, and medications, surgery becomes a viable option to consider.
Surgical Procedures
The primary goal of surgical treatment for meralgia paresthetica is to decompress or release the lateral femoral cutaneous nerve from any structures that may be compressing it. The most common surgical procedures include neurolysis, which involves freeing the nerve from surrounding tissues, and nerve transection, which involves cutting the nerve to prevent the transmission of pain signals. In some cases, the nerve may be transposed or moved to a different location to reduce the risk of future compression. The choice of surgical procedure depends on the extent of nerve damage and the surgeon’s preference.
RELATED: Eosinophilic Esophagitis: From Symptoms to Treatment Plans
Recovery and Prognosis
Following surgery for meralgia paresthetica, patients can expect a recovery period of several weeks. During this time, activity restrictions may be necessary to allow proper healing of the surgical site. Pain and numbness in the affected area may persist for some time after surgery, but these symptoms typically improve gradually as the nerve recovers. Physical therapy may be recommended to help with desensitization and to regain strength and mobility in the affected leg. The prognosis for individuals who undergo surgery for meralgia paresthetica is generally favorable, with a high success rate in relieving symptoms and improving quality of life. However, as with any surgical procedure, there are potential risks and complications to consider, such as infection, bleeding, and nerve damage.
Conclusion
Treating meralgia paresthetica effectively requires a thorough understanding of its causes, symptoms, and available treatment options. From lifestyle changes and physical therapy to medications and, in severe cases, surgical interventions, there are various approaches to manage this condition. The key is to work closely with healthcare professionals to develop a tailored treatment plan that addresses individual needs and severity of symptoms.
By taking proactive steps to alleviate pressure on the affected nerve and seeking appropriate medical care, most people with meralgia paresthetica can find relief and improve their quality of life. Remember, early diagnosis and treatment are crucial to prevent long-term nerve damage and to ensure the best possible outcomes. Whether through conservative methods or more advanced interventions, there are solutions available to help individuals regain comfort and functionality in their daily lives.