Creutzfeldt-Jakob Disease, a rare but fatal degenerative brain disorder, has long intrigued and alarmed the medical community due to its rapid progression and severe impact on neurological functions. This condition, although uncommon, poses critical challenges in diagnosis and management, underscoring the importance of understanding its symptoms and underlying causes. The recognition of what causes Creutzfeldt-Jakob Disease and its potential ramifications not only aids in early detection but also highlights the critical need for advancing treatments to mitigate its devastating effects. With no known cure, the stakes in comprehending and addressing this disease are alarmingly high, making it a focal point of neurodegenerative research.
This article aims to demystify Creutzfeldt-Jakob Disease by detailing its causes, enumerating the symptoms, and discussing the risk factors associated with its development. Subsequent sections will delve into the diagnostic criteria, the current landscape of treatments and management strategies, and the ongoing research efforts dedicated to combating this disease. By providing a comprehensive overview, the guide serves as an invaluable resource for understanding the complex nature of Creutzfeldt-Jakob Disease, facilitating a better grasp of its prognosis, and recognizing the imperative for continued research in finding definitive creutzfeldt-jakob disease treatments.
What is Creutzfeldt-Jakob Disease?
Creutzfeldt-Jakob Disease (CJD) is a rare, fatal degenerative brain disorder, which is part of a family of diseases known as prion diseases or transmissible spongiform encephalopathies. It primarily affects the central nervous system, leading to severe neurological impairment. The disease is characterized by its rapid progression, typically leading to death within a year of onset.
Overview of Prion Diseases
Prion diseases involve the accumulation of an abnormal infectious protein called a prion in the brain. Unlike viruses and bacteria, prions are resistant to the methods typically used to destroy pathogens, such as heat and radiation, and do not respond to antibiotics or antiviral medications. In CJD, these prions cause irreversible damage to nerve cells, leading to the symptoms associated with the disease.
Forms of Creutzfeldt-Jakob Disease
There are several forms of CJD, each with distinct characteristics:
- Sporadic CJD: This is the most common form, accounting for approximately 85% of cases. It occurs spontaneously, without any known cause.
- Hereditary CJD: About 10 to 15% of cases in the United States are familial, resulting from a genetic mutation.
- Acquired CJD: Although very rare, CJD can be acquired through exposure to infected brain or nervous system tissue, typically through medical procedures. This form is known as iatrogenic CJD.
- Variant CJD (vCJD): Linked to the consumption of meat from cattle afflicted with bovine spongiform encephalopathy (BSE), also known as mad cow disease, this type affects younger individuals and has a slightly longer progression.
Symptoms and Progression
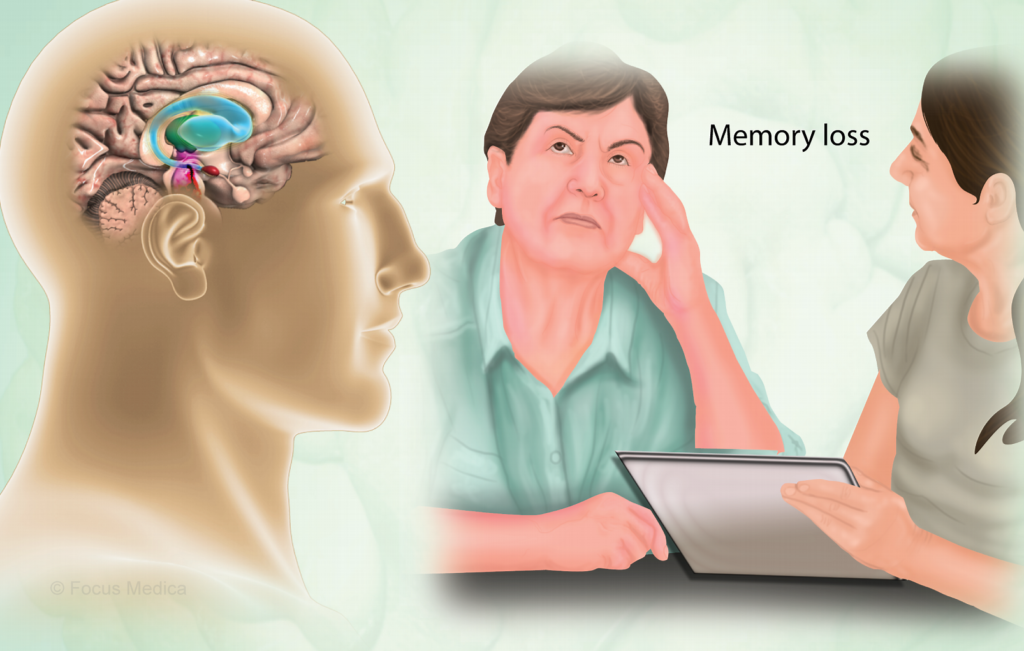
The initial symptoms of Creutzfeldt-Jakob Disease may be mistaken for other forms of dementia such as Alzheimer’s disease, due to similar symptoms like memory loss and impaired thinking. However, CJD progresses much more rapidly. Early symptoms include personality changes, memory loss, and problems with coordination. As the disease advances, patients may experience myoclonus or involuntary muscle jerks, severe mental deterioration, blindness, and eventually the loss of ability to move or speak.
Incidence and Impact
Globally, CJD is extremely rare, with about 1 to 2 cases diagnosed per million people each year. In the United States, around 350 cases are reported annually. The rapid progression and severity of the disease highlight the importance of understanding its mechanisms and developing effective treatments.
Creutzfeldt-Jakob Disease remains a challenging and devastating condition, with ongoing research focused on uncovering more about its causes and potential treatments.
Causes of Creutzfeldt-Jakob Disease
Creutzfeldt-Jakob Disease (CJD) is primarily caused by the abnormal folding of a protein known as a prion. Prions are infectious agents composed mostly of protein, which can induce abnormal folding of normal cellular prion proteins in the brain, leading to brain damage. This section explores the various ways CJD can manifest, categorized into sporadic, familial, acquired, and variant forms.
Sporadic
The majority of CJD cases are classified as sporadic CJD, which appears without any known cause. This form accounts for about 85% of cases. Research suggests that sporadic CJD may occur when a normal prion protein spontaneously misfolds and turns into a pathological prion. Although the exact trigger is unknown, it is more likely to occur in individuals possessing specific genetic variations in the prion protein gene.
Familial
Familial CJD is a rare inherited form, accounting for 10-15% of cases. It is caused by mutations in the prion protein gene (PRNP). These genetic alterations lead to the production of prions that eventually cause the disease. Familial forms of the disease can also include other prion diseases like Gerstmann-Straussler-Scheinker syndrome and fatal familial insomnia. Each mutation can lead to slightly different clinical manifestations and disease progression.
Acquired
CJD can also be acquired through exposure to brain or nervous system tissue, usually through certain medical procedures. Historically, cases of iatrogenic CJD have been reported following the transplantation of infected human tissue, such as corneas, dura mater grafts, or the administration of contaminated human growth hormone. Modern medical practices have significantly reduced this risk through improved screening and sterilization techniques.
Variant
Variant CJD (vCJD) is linked to the consumption of meat from cattle affected by Bovine Spongiform Encephalopathy (BSE), commonly known as mad cow disease. It primarily affects younger individuals and has a longer duration of illness compared to sporadic CJD. The prions from affected cattle are believed to infect humans, leading to vCJD. This form was first identified in the UK in the late 1990s during an outbreak of BSE.
Understanding these causes and the mechanisms of prion transmission and mutation is crucial for developing effective prevention and treatment strategies for CJD.
Symptoms of Creutzfeldt-Jakob Disease
Early Symptoms
The onset of Creutzfeldt-Jakob Disease (CJD) presents a variety of symptoms that can significantly impact an individual’s daily life. These symptoms are largely neurological and psychological, manifesting differently based on the type of CJD. In sporadic CJD, individuals primarily experience neurological symptoms that rapidly worsen over a few months. These include difficulty walking due to balance and coordination problems, slurred speech, numbness or pins and needles in different parts of the body, dizziness, vision problems such as double vision, and hallucinations.
Conversely, variant CJD starts with psychological symptoms like severe depression, withdrawal from social interactions, anxiety, irritability, and insomnia. Neurological symptoms follow approximately four months later, worsening over time. Familial CJD mirrors the sporadic form but progresses over about two years, while the pattern for iatrogenic CJD varies based on exposure to the infectious prion protein.
Advanced Symptoms
As CJD advances, symptoms become more severe and debilitating. All forms of CJD lead to a loss of physical coordination, affecting functions such as walking, speaking, and maintaining balance (ataxia). Individuals may experience muscle twitches and spasms, loss of bladder and bowel control, blindness, swallowing difficulties (dysphagia), loss of speech, and the inability to perform voluntary movements. Psychological symptoms also intensify, including severe memory loss, concentration problems, confusion, agitation, aggressive behavior, loss of appetite leading to weight loss, paranoia, and unusual emotional responses.
Final Stages
In the final stages of CJD, individuals become totally bedridden and lose awareness of their surroundings, requiring constant care. The ability to speak and communicate is lost, and death usually follows as a result of complications such as infections (e.g., pneumonia) or respiratory failure. The progression from early symptoms to death varies, with an average duration of four to six months for most patients. Ninety percent of individuals with CJD die within a year of symptom onset, although some cases may last longer, especially in younger patients or those with variant CJD, which can last 12 to 14 months. Variably protease-sensitive prionopathy (VPSPr), another rare prion disease, mimics other forms of dementia and has a longer course, lasting about 24 months.
Understanding the symptoms of Creutzfeldt-Jakob Disease across its stages is crucial for early detection and care planning, despite the current lack of a cure.
Risk Factors for Creutzfeldt-Jakob Disease
Identifying risk factors for Creutzfeldt-Jakob Disease (CJD) is challenging, as most cases occur without a known reason. However, certain factors have been associated with different forms of CJD, providing some insight into potential risks.
Age
The likelihood of developing sporadic CJD increases later in life, typically around age 60. Familial CJD tends to occur slightly earlier than sporadic cases. In contrast, variant Creutzfeldt-Jakob Disease (vCJD) predominantly affects younger individuals, usually in their late 20s. This variation in age of onset across the different forms of CJD underscores the role that age plays as a risk factor.
Genetics
Genetic factors play a crucial role, especially in familial CJD. This form of the disease results from genetic changes that cause CJD, with a child needing only one copy of the gene from either parent to be at risk. The chance of passing this gene to offspring stands at 50%. The most common mutation identified is the E200K mutation in the prion protein gene (PRNP), with variations in genetic susceptibility affecting the disease’s appearance and symptoms. Additionally, the M129V polymorphism in the PRNP gene has been identified as a nonspecific genetic risk factor, influencing susceptibility to all forms of CJD and other neurodegenerative diseases. Methionine homozygosity (Met/Met) at codon 129 significantly increases the risk for all forms of CJD, particularly the variant form.
Exposure to Contaminated Tissue
Exposure to contaminated tissue presents a risk for iatrogenic CJD. This can occur through medical procedures involving the transfer of infected human tissue, such as corneal transplants, dura mater grafts, or the use of contaminated surgical instruments. Historically, cases of iatrogenic CJD have resulted from the transplantation of infected tissue or the administration of contaminated human growth hormone. Although the risk has been significantly reduced through improved screening and sterilization techniques, it remains a concern. Variant CJD, linked to consuming meat from cattle with Bovine Spongiform Encephalopathy (BSE or “mad cow disease”), represents another form of CJD acquired through exposure to contaminated tissue.
Identifying and understanding these risk factors are crucial steps toward developing effective prevention strategies and enhancing our overall comprehension of Creutzfeldt-Jakob Disease.
Diagnosis of Creutzfeldt-Jakob Disease
Diagnosing Creutzfeldt-Jakob Disease (CJD) involves a comprehensive evaluation by a neurologist to distinguish it from other conditions with similar neurological symptoms, such as Alzheimer’s disease, Parkinson’s disease, or brain tumors. The definitive diagnosis of CJD can only be confirmed through the examination of brain tissue, typically obtained post-mortem. However, several diagnostic tools and tests are used to assess the likelihood of CJD during a patient’s life.
Neurological Exams
Neurological examinations are critical in the initial assessment of suspected CJD cases. These exams focus on identifying characteristic signs of the disease, including:
- Muscle twitching and spasms
- Changes in reflexes
- Problems with coordination
- Vision impairments, potentially leading to blindness
These clinical evaluations help to pinpoint symptoms that are unusual for other neurodegenerative diseases, which is crucial for an accurate preliminary diagnosis.
Diagnostic Tests
A series of specialized tests are employed to support the diagnosis of CJD:
- Magnetic Resonance Imaging (MRI): This imaging technique uses magnetic fields and radio waves to create detailed images of the brain. It is particularly useful for identifying the specific brain abnormalities associated with CJD.
- Electroencephalogram (EEG): An EEG measures the electrical activity of the brain. The test can detect characteristic patterns that suggest CJD, particularly in sporadic cases.
- Lumbar Puncture (Spinal Tap): This procedure involves the extraction of cerebrospinal fluid to test for markers indicative of CJD, such as the 14-3-3 protein.
- Real-Time Quaking-Induced Conversion (RT-QuIC): A relatively new diagnostic test that can detect the abnormal prion proteins responsible for CJD in cerebrospinal fluid.
Genetic Testing
For cases suspected to be familial CJD, genetic testing plays a pivotal role. A simple blood test can identify mutations in the prion protein gene (PRNP), which are indicative of hereditary prion diseases. Identifying these genetic mutations can confirm the diagnosis and help in understanding the disease’s progression and potential impact on family members.
These diagnostic approaches are complemented by the insights and guidance from specialist services such as the National CJD Research and Surveillance Unit in Edinburgh and the National Prion Clinic in London. These institutions provide crucial support in diagnosing complex cases and in the research towards better understanding and managing CJD.
Treatment and Management of Creutzfeldt-Jakob Disease
Symptom Management
Given the absence of a cure for Creutzfeldt-Jakob Disease (CJD), the focus of treatment is primarily on symptom management. The rapid progression of the disease often limits the effectiveness of treatments, but certain interventions can provide relief for some symptoms. For instance, psychological symptoms such as anxiety and depression may be addressed with sedatives and antidepressants. Furthermore, pain, a symptom experienced by some individuals with CJD, can be managed using opiate-based painkillers. These measures aim to improve the quality of life for individuals with CJD by reducing the severity of their symptoms.
Palliative Care
Palliative care represents a critical component of managing Creutzfeldt-Jakob Disease, focusing on reducing suffering and improving the quality of life for both patients and their caregivers. This care approach includes comprehensive symptom management, emotional and spiritual support, and guidance regarding treatment decisions. Palliative care is especially vital given the rapid decline in function seen in CJD, which can lead to symptoms comparable to the advanced stages of other neurodegenerative diseases within a few months. The involvement of palliative care from the point of diagnosis can facilitate advance care planning and provide anticipatory guidance, helping patients and their families navigate the challenges of the disease.
Supportive Care
Supportive care for individuals with CJD encompasses a broad range of services aimed at addressing the complex needs arising as the disease progresses. This includes significant nursing care and practical support, particularly as individuals lose the ability to perform daily activities independently. Assistance may be required for feeding, washing, and mobility. In some cases, a catheter may be necessary for bladder management, and many patients will experience difficulties swallowing, necessitating nutrition and fluids through a feeding tube. Depending on the severity and progression of the condition, it may be possible to provide care at home, although many caregivers opt for the specialist services offered by hospitals or hospices. Supportive care also involves nonpharmacologic management strategies, such as involving an interdisciplinary team to support caregivers and patients through social, psychological, and spiritual challenges.
The management of CJD is challenging due to its rapid progression and the absence of disease-altering treatments. However, through symptom management, palliative care, and supportive care, it is possible to make the patient as comfortable as possible and provide meaningful support to their families and caregivers during this difficult time.
Conclusion
Through this comprehensive guide, we have journeyed into the intricacies of Creutzfeldt-Jakob Disease, delving into its symptoms, causes, diagnostic challenges, and the existing paradigm of management and care for those affected. The amalgamation of scientific insights and diagnostic criteria underscores the critical nature of early detection and supportive care, in light of the absence of a cure. The exploration into the familial, sporadic, and variant forms of the disease not only reinforces the complexity of CJD but also the indispensable need for personalized care and ongoing research to navigate its devastating impact.
Reflecting upon the broader implications, it becomes evident that Creutzfeldt-Jakob Disease, while rare, poses significant challenges to the medical community and society at large. The urgency for continued research in finding definitive treatments and enhancing diagnostic techniques cannot be overstated. As the quest for understanding and combating this formidable disease progresses, the collective efforts of researchers, clinicians, and families affected by CJD remain crucial. It is through these concerted efforts that hope for advancements in treatment and ultimately, a cure, continues to burn brightly, offering a glimmer of hope amidst the uncertainty that characterizes Creutzfeldt-Jakob Disease.