Atherosclerosis, often silently lurking within the arteries, gradually narrows and hardens them, posing a significant risk to cardiovascular health. This stealthy condition, commonly misconceived as an inevitable part of aging, actually results from complex interplays between lifestyle, genetic factors, and internal inflammation. Its significance cannot be overstated, as it underpins many forms of heart disease, the leading cause of death globally. By understanding atherosclerosis, individuals can take proactive steps to mitigate its development and safeguard their health, highlighting the critical need for awareness and education on this matter.
This article delves into the essentials of atherosclerosis, starting with a clear explanation of what the condition entails and moving through its causes, signs, and symptoms that signal its onset. It further explores diagnostic methods and tests employed to detect atherosclerosis, followed by an overview of current treatment protocols designed to manage and possibly reverse the condition. Equally important, the article highlights prevention strategies, offering actionable advice for those looking to reduce their risk. Through these discussions, readers will gain a comprehensive understanding of atherosclerosis, empowering them with the knowledge to take charge of their cardiovascular health.
Understanding Atherosclerosis
Definition and Basics
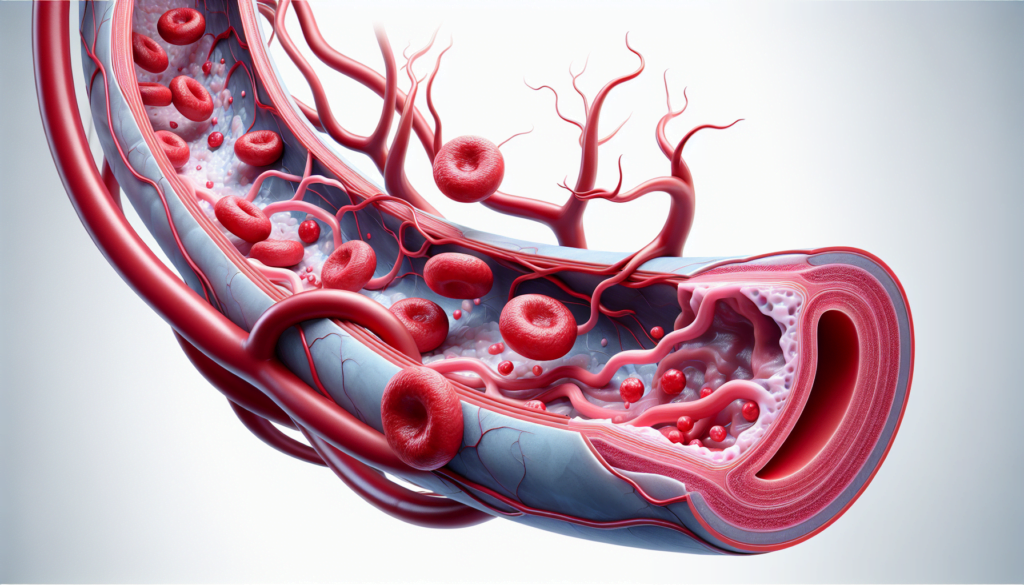
Atherosclerosis is a condition characterized by the buildup of fats, cholesterol, and other substances in and on the artery walls, a process commonly referred to as plaque formation. This plaque buildup can lead to the narrowing of arteries, significantly restricting blood flow and potentially causing blockages. These blockages can result in serious cardiovascular diseases if a plaque bursts, leading to the formation of a blood clot. It is essential to recognize that atherosclerosis can affect arteries not just in the heart but throughout the body, including those in the brain, arms, legs, pelvis, and kidneys.
The development of atherosclerosis is typically slow and can start as early as childhood, worsening with age. Factors contributing to this condition include unhealthy cholesterol levels, poor lifestyle choices, and genetic predisposition. However, it is treatable and preventable through healthy lifestyle habits, emphasizing the importance of early detection and management.
Difference Between Atherosclerosis and Arteriosclerosis
While often used interchangeably, atherosclerosis and arteriosclerosis refer to different conditions. Arteriosclerosis is a broader term that describes the thickening and hardening of the arteries, generally associated with aging. This condition leads to less elastic arterial walls, which can increase blood pressure and reduce the overall flexibility of the vascular system.
On the other hand, atherosclerosis is a specific type of arteriosclerosis that involves the accumulation of plaque inside the arteries. This plaque consists of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, a clotting material in the blood. The risk factors for both conditions overlap somewhat, but the mechanisms and implications of atherosclerosis are more directly linked to cardiovascular health risks such as heart attacks, strokes, and peripheral artery disease.
Understanding the nuances between these two conditions is crucial for proper diagnosis and treatment. Atherosclerosis, specifically, requires targeted interventions to manage the buildup of plaque and prevent severe cardiovascular events. By addressing factors such as diet, exercise, and cholesterol management, individuals can significantly reduce their risk of developing severe atherosclerotic complications.
Causes of Atherosclerosis
Atherosclerosis is a complex condition influenced by various genetic, lifestyle, and medical factors. This section explores the primary causes that contribute to the development of atherosclerosis.
Genetic Factors
Research indicates that genetics play a significant role in the susceptibility to atherosclerosis. Specific genes and genetic polymorphisms are linked to variations in lipid metabolism, inflammation, and thrombogenesis, which can predispose individuals to this disease. Notably, familial hypercholesterolemia, a common inherited disorder, markedly increases cholesterol levels, thereby enhancing the risk of developing atherosclerotic plaques. Studies utilizing genetic models and inbred mouse strains have demonstrated that genetic factors can influence the severity and progression of atherosclerosis, independent of external factors.
Lifestyle Choices
Lifestyle choices significantly impact the development of atherosclerosis. Factors such as smoking, physical inactivity, and unhealthy dietary habits contribute to the buildup of plaque in the arteries. Smoking is particularly harmful as it directly damages the arterial walls and reduces the effectiveness of other risk management strategies. Diets high in saturated fats and low in fiber increase cholesterol levels, which accelerates plaque formation. Furthermore, physical inactivity is linked to poor cardiovascular health and increased atherosclerotic risk. Engaging in regular physical activity can mitigate these risks by improving lipid profiles and enhancing overall heart health.
Medical Conditions
Several medical conditions exacerbate the risk of developing atherosclerosis. High blood pressure and diabetes are notable contributors; they damage the inner layers of arterial walls, promoting plaque accumulation. Metabolic syndrome, characterized by a cluster of conditions including high blood pressure, high blood sugar levels, excess body fat around the waist, and abnormal cholesterol levels, further elevates the risk. Chronic inflammation from conditions such as arthritis, lupus, and psoriasis can also lead to vascular damage and atherosclerosis. Additionally, age-related factors increase susceptibility, with risks escalating as individuals age, particularly after the age of 45 in men and 55 in women.
Understanding these causes is crucial for both preventing and managing atherosclerosis, highlighting the importance of genetic screening, lifestyle modifications, and control of associated medical conditions to mitigate the risk of serious cardiovascular events.
Symptoms and Early Signs
Atherosclerosis often progresses silently and may not present symptoms until an artery is significantly narrowed or blocked. Recognizing the symptoms early is crucial for managing and potentially reversing the effects of this disease.
Symptomatology Based on Affected Arteries
The symptoms of atherosclerosis vary depending on which arteries are affected:
- Heart Arteries: If atherosclerosis affects the coronary arteries, individuals may experience chest pain or pressure, known as angina. This symptom occurs because the heart muscle is not receiving enough oxygen-rich blood during periods of physical exertion or stress.
- Brain Arteries: Atherosclerosis in the arteries leading to the brain can manifest as sudden numbness or weakness in the arms or legs, difficulty speaking or slurred speech, temporary loss of vision in one eye, or facial muscle drooping. These symptoms are indicative of a transient ischemic attack (TIA), which, if untreated, could progress to a stroke.
- Peripheral Arteries: When atherosclerosis occurs in the arteries of the arms and legs, it can lead to peripheral artery disease. Symptoms include leg pain when walking (claudication) and decreased blood pressure in the affected limb.
- Renal Arteries: In the arteries leading to the kidneys, atherosclerosis can cause high blood pressure or kidney failure.
Asymptomatic Cases
In its early stages, atherosclerosis usually does not cause any symptoms. Often, symptoms first appear under physical or emotional stress when the body demands more oxygen. In asymptomatic cases, the disease can be identified through various diagnostic methods such as coronary angiography, intravascular ultrasonography, and computed tomography. These methods can detect the disease in subclinical stages, highlighting the importance of regular health screenings.
Mild atherosclerosis typically remains symptom-free. However, as the condition advances, symptoms become more apparent and can significantly impact the quality of life. It is critical to understand that while atherosclerosis can remain hidden for years, its progression can lead to severe cardiovascular events like heart attacks or strokes if not addressed timely. Regular check-ups and monitoring of heart health can aid in early detection and management of the disease.
Diagnosis and Tests
Physical Examination
To diagnose atherosclerosis, healthcare providers begin with a comprehensive physical examination. During this examination, they assess the patient’s medical and family history and conduct a physical evaluation to detect any symptoms indicative of the condition. Regular checks from the age of 20 help identify risk factors for plaque buildup in the arteries. Key aspects of the physical examination may include checking blood pressure, calculating body mass index (BMI), and measuring waist circumference to evaluate whether a patient has an unhealthy weight. Additionally, healthcare providers may listen to the arteries using a stethoscope to detect a whooshing sound known as a bruit, which can indicate turbulent blood flow caused by narrowing arteries.
Blood Tests
Blood tests are a critical component in diagnosing atherosclerosis. These tests check levels of cholesterol, triglycerides, blood sugar, and lipoproteins. They also measure proteins that are signs of inflammation, such as C-reactive protein (CRP), which is linked to arterial inflammation. High levels of blood sugar and cholesterol are known risk factors for atherosclerosis, making these tests essential for assessing an individual’s risk and the presence of the condition.
Imaging and Specialized Tests
Imaging and specialized tests provide detailed insights into the heart’s structure and function, helping to confirm the diagnosis of atherosclerosis. These tests include:
- Electrocardiogram (ECG or EKG): This simple, painless test records the heart’s electrical activity, showing the heart’s rhythm and the timing of electrical impulses. It can detect heart conditions, including effects from past heart attacks.
- Echocardiogram: This ultrasound test creates images of the heart, showing how well the heart and its valves are functioning and identifying areas of poor blood flow.
- Stress Tests: These tests measure heart function under physical stress, typically using a treadmill or stationary bike. They can reveal heart problems that aren’t apparent when the heart is at rest. For those unable to exercise, medication may be used to mimic the effects of exercise on the heart.
- Ankle-Brachial Index (ABI): This test compares blood pressures in the ankle and arm to diagnose peripheral artery disease, often associated with atherosclerosis.
- Imaging Tests:
- Angiography: Uses a special dye and X-rays to view blood flow in the arteries and identify blockages.
- Computed Tomography (CT) Angiography and Coronary Calcium Scan: These tests provide detailed images of the heart and arteries, showing calcium deposits and plaque buildup.
- Magnetic Resonance Imaging (MRI) and Cardiac MRI: These tests offer detailed images of the heart and blood vessels, assessing blood flow and tissue damage.
- Positron Emission Tomography (PET): This nuclear scan evaluates blood flow at the microvascular level and can detect inflammation.
- Intravascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT): These advanced imaging techniques provide detailed information about the composition and structure of arterial plaques, crucial for assessing the severity of atherosclerosis.
These diagnostic tools are integral to detecting atherosclerosis at various stages, from initial functional abnormalities to advanced plaque formation, allowing for timely and targeted interventions.
Treatment Approaches
Lifestyle Changes
The foundation of managing and preventing atherosclerosis involves substantial lifestyle changes. These changes not only help in slowing the progression of the disease but can also enhance overall cardiovascular health. Key lifestyle modifications include:
- Smoking Cessation: Stopping smoking is crucial as tobacco smoke is a significant risk factor for atherosclerosis. Healthcare professionals can support smoking cessation through behavioral interventions combined with pharmacological treatments.
- Dietary Adjustments: Adopting a heart-healthy diet is essential. This includes increasing the intake of fruits, vegetables, and whole grains while reducing the consumption of saturated fats and cholesterol. Such dietary practices help in managing blood cholesterol levels and reducing atherosclerosis risk.
- Regular Physical Activity: Engaging in regular exercise, such as 30 to 45 minutes of moderate activity most days of the week, helps improve heart health and control weight. Exercise can also aid in reducing blood pressure and enhancing lipid profiles.
- Weight Management: Maintaining a healthy weight is crucial as obesity is a risk factor for atherosclerosis. Even a modest weight loss can significantly impact cardiovascular health and reduce the risks associated with atherosclerosis.
- Stress Management: Managing stress effectively through techniques like yoga, meditation, or regular social activities can reduce the physiological impacts of stress on the cardiovascular system.
- Regular Health Screenings: Regular check-ups and screenings are vital, especially for individuals over 65 or those with pre-existing health conditions, to monitor cardiovascular health and manage risk factors effectively.
Medication
Medications play a pivotal role in the treatment of atherosclerosis, especially when lifestyle changes alone are insufficient. Medications used include:
- Statins and Other Cholesterol-lowering Drugs: These medications reduce levels of “bad” cholesterol and are central in the management of atherosclerosis.
- Blood Pressure Medications: While these do not reverse atherosclerosis, they are crucial in managing blood pressure and reducing the risk of cardiovascular complications.
- Anti-platelet Drugs: Medications like aspirin may be prescribed to prevent blood clots, reducing the risk of heart attack or stroke.
- Diabetes Medications: Controlling blood sugar is vital for patients with diabetes to prevent the progression of atherosclerosis.
- Other Specialized Medications: These may include drugs to reduce inflammation or specific symptoms associated with atherosclerosis.
Surgical Interventions
In cases where atherosclerosis is advanced and poses high risks, surgical interventions may be necessary. These procedures are aimed at restoring normal blood flow and preventing serious cardiovascular events:
- Angioplasty and Stent Placement: This procedure involves using a balloon to open up clogged arteries and placing a stent to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): This surgery uses vessels from other parts of the body to bypass blocked coronary arteries.
- Carotid Endarterectomy: This involves the removal of plaque from the carotid arteries to prevent strokes.
- Peripheral Artery Bypass Surgery: Similar to CABG, this surgery uses grafts to bypass blocked arteries in the legs or arms.
These treatments are selected based on the severity and location of artery blockage, and they aim to significantly reduce the symptoms and risks associated with atherosclerosis.
Prevention Strategies
Diet and Nutrition
A critical component of preventing atherosclerosis involves adhering to a heart-healthy diet. The American Heart Association recommends incorporating a variety of nutritious foods to support cardiovascular health. Key dietary practices include:
- Increasing Intake of Fruits and Vegetables: Consuming a diverse range of fruits and vegetables helps reduce the risk of cardiovascular disease by supplying essential vitamins, minerals, and fiber.
- Choosing Whole Grains: Whole grains are preferred over refined grains because they provide more nutrients and fiber, which can help manage cholesterol levels.
- Including Healthy Fats: Sources of monounsaturated and polyunsaturated fats, such as nuts, seeds, avocados, and olive oil, should be included in the diet to improve heart health.
- Limiting Saturated and Trans Fats: Reducing intake of saturated fats and avoiding trans fats help lower cholesterol levels and reduce the risk of coronary heart disease.
- Moderating Sodium and Sugar Intake: Keeping sodium and added sugars below recommended levels helps prevent hypertension and atherosclerosis.
- Opting for Plant-based Diets: Diets like the Mediterranean, DASH, and vegetarian diets not only support weight management but also improve lipid profiles and reduce overall cardiovascular risk.
Exercise and Physical Activity
Regular physical activity is paramount in preventing atherosclerosis and managing overall cardiovascular health. The American College of Sports Medicine and the Centers for Disease Control and Prevention recommend:
- Moderate-Intensity Physical Activity: At least 30 minutes of moderate-intensity exercise, such as brisk walking, cycling, or swimming, should be performed on most days of the week.
- Strength Training: Incorporating muscle-strengthening activities at least two days per week enhances overall physical health and cardiovascular fitness.
- Flexibility and Balance Exercises: Activities like yoga and stretching improve flexibility and balance, which are crucial for overall well-being, especially in older adults.
Engaging in physical activity not only reduces the risk of cardiovascular disease but also improves mood, enhances weight management, and boosts energy levels.
Smoking Cessation and Managing Chronic Conditions
Smoking cessation is one of the most effective ways to reduce the risk of atherosclerosis and its complications. Healthcare providers play a critical role in supporting individuals in their journey to quit smoking by offering various interventions, including:
- Behavioral Therapy: Counseling and support groups can help individuals understand the triggers of smoking and develop strategies to quit.
- Pharmacotherapy: Medications such as nicotine replacement therapy can alleviate withdrawal symptoms and reduce the urge to smoke.
Additionally, managing chronic conditions such as hypertension, diabetes, and high cholesterol is vital in preventing atherosclerosis. Regular monitoring and appropriate medical treatment of these conditions can significantly reduce the risk of developing severe cardiovascular diseases.
By implementing these strategies, individuals can significantly enhance their cardiovascular health and reduce the risk of atherosclerosis.
Conclusion
This comprehensive exploration of atherosclerosis underscores the critical facets of identifying, managing, and preventing a condition that stands as a leading threat to cardiovascular health worldwide. From the foundational understanding of the disease, its causes, and symptoms, to the detailed discussions on diagnostic tests, treatment approaches, and prevention strategies, the article has equipped readers with essential knowledge. Emphasizing the interplay between lifestyle choices and genetic predispositions in influencing atherosclerosis progression, the content underscores the empowerment that comes from informed health decisions.
Taking proactive steps towards lifestyle modifications, including dietary adjustments, regular physical activity, and smoking cessation, coupled with managing chronic conditions, emerges as a pivotal strategy in combating atherosclerosis. As individuals embrace these practices and healthcare providers offer tailored support and treatment, the potential to significantly mitigate the disease’s progression and impact on life expectancy becomes evident. This article serves as a valuable resource, encouraging ongoing education and action in the pursuit of optimal cardiovascular health and the prevention of atherosclerosis.