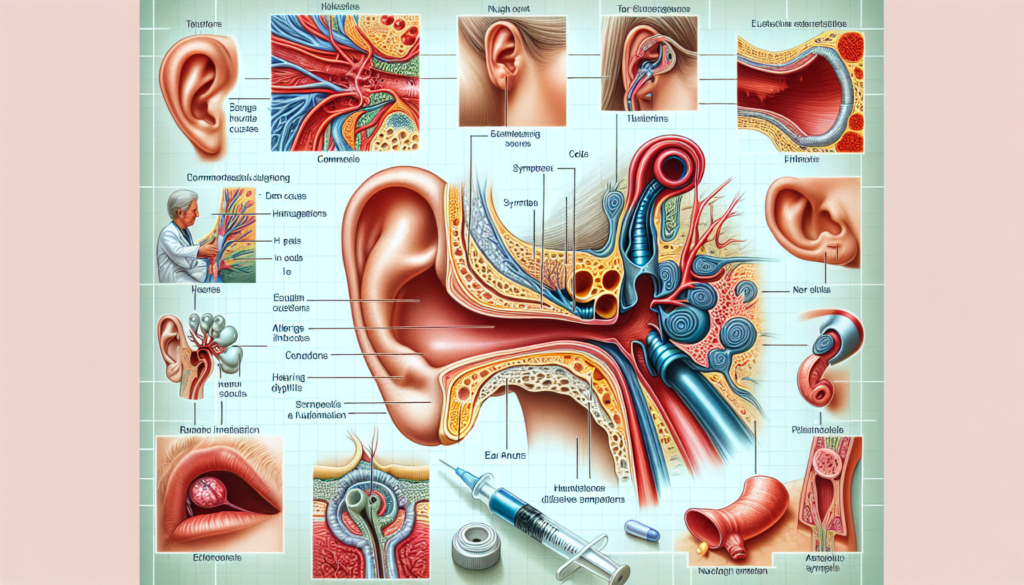
The eustachian tube is a small passageway that connects the middle ear to the back of the throat. When this tube becomes blocked or does not open properly, it can lead to a condition known as eustachian tube dysfunction. Eustachian tube dysfunction affects millions of people worldwide and can cause a range of uncomfortable symptoms that impact daily life.
This article will provide a comprehensive overview of eustachian tube dysfunction, including its causes, symptoms, and available treatment options. It will compare the different types of eustachian tube dysfunction, explore home remedies versus medications, and discuss surgical interventions. The article will also address short-term versus long-term management strategies and consider costs and insurance coverage for treatment. By the end, readers will have a clearer understanding of eustachian tube dysfunction and be equipped with information to make informed decisions about their care.
Overview of Eustachian Tube Dysfunction
The eustachian tube is a small passageway that connects the middle ear to the back of the throat. It serves several important functions, including:
- Balancing pressure in the middle ear
- Draining fluid from the middle ear
- Protecting the ear from sounds caused by the body and nasal drainage
The eustachian tube contains a valve that opens and closes. If this valve does not open adequately, it can lead to a buildup of fluid in the ears, causing pain and pressure. On the other hand, if the tube remains open for too long, it can result in a persistent feeling of pressure and the ability to hear unusual sounds like breathing or one’s own voice too loudly. Eustachian tube disorders are common and a leading cause of ear infections (otitis media).
The most common types of eustachian tube disorders include:
- Patulous eustachian tube dysfunction
- Obstructive eustachian tube dysfunction
- Baro-challenge-induced eustachian tube dysfunction (obstructive dysfunction that occurs during airplane flights or scuba diving)
Patulous Eustachian Tube Dysfunction
Patulous eustachian tube dysfunction occurs when the valve of the eustachian tube remains open. This allows sound to travel from the nasal-sinus cavity to the ears, causing the person to hear their own voice, breathing, or even blood pumping too loudly. Symptoms include a sense of fullness in the ears and the ability to hear bodily functions very clearly.
Causes of patulous eustachian tube dysfunction may include weight loss, chronic neuromuscular or immunological diseases, chronic nasal allergies, acid reflux disease, and stress or anxiety. Diagnosis involves the doctor observing the eardrum’s response to deep breathing and swallowing, as well as measuring ear pressure.
Treatment options for patulous eustachian tube dysfunction include limiting decongestants and caffeine, drinking more water, using medicated nasal drops, and in some cases, surgery such as implants, fillers, grafts, or fat transfers to help the eustachian tube close properly.
Obstructive Eustachian Tube Dysfunction
Obstructive eustachian tube dysfunction occurs when the valve does not open properly, preventing pressure from balancing and fluids from draining out of the ear. Symptoms include pressure, pain, fullness in the ears, and muffled hearing.
Causes of obstructive eustachian tube dysfunction include environmental allergies, sinusitis, acid reflux, abnormal tissue growth (neoplasms), and impaired muscle coordination or deficiency, such as in patients with cleft palate.
Diagnosis involves the doctor observing changes in the eardrum’s shape due to negative pressure buildup. Treatment may include medication or surgery, such as tympanostomy tubes (ear tubes), balloon dilation of the eustachian tube, adenoidectomy, or laser treatment to reduce inflamed tissue.
Baro-challenge-induced eustachian tube dysfunction is a type of obstructive dysfunction that occurs only during airplane flights or scuba diving due to changes in altitude and pressure.
It’s important to note that while decongestants and antihistamines are commonly used to treat eustachian tube dysfunction, in some cases, they may worsen the condition. If symptoms persist, it’s best to consult an ear, nose, and throat specialist for proper evaluation and treatment.
Comparison of ETD Type
There are three main types of eustachian tube dysfunction (ETD): patulous ETD, obstructive ETD, and baro-challenge-induced ETD. While they all involve dysfunction of the eustachian tube, each type has distinct characteristics, causes, and symptoms.
Patulous ETD vs. Obstructive ETD
Patulous ETD occurs when the eustachian tube remains open, allowing sound to travel from the nasal cavity to the ears. This can cause distortion of one’s own voice and breathing sounds. Symptoms of patulous ETD include a sense of fullness in the ears and the ability to hear bodily functions very loudly.
In contrast, obstructive ETD happens when the eustachian tube fails to open properly, preventing pressure equalization and fluid drainage from the middle ear. This leads to symptoms such as pressure, pain, fullness in the ears, and muffled hearing.
The causes of these two types of ETD also differ. Patulous ETD may be caused by weight loss, chronic diseases, nasal allergies, acid reflux, and stress. Obstructive ETD, on the other hand, can result from allergies, sinusitis, acid reflux, abnormal tissue growth, and impaired muscle function.
Obstructive ETD vs. Baro-challenge-induced ETD
Baro-challenge-induced ETD is a subtype of obstructive ETD that occurs specifically during changes in atmospheric pressure, such as when flying or scuba diving. The rapid pressure changes can cause the eustachian tube to become blocked, leading to symptoms similar to those of obstructive ETD.
The main difference between obstructive ETD and baro-challenge-induced ETD is the triggering factor. While obstructive ETD can occur due to various causes, baro-challenge-induced ETD is specifically triggered by pressure changes. Additionally, symptoms of baro-challenge-induced ETD may only be present during or after exposure to these pressure changes, while obstructive ETD symptoms can persist.
Diagnosis and treatment options may vary depending on the type of ETD. Patulous ETD is often diagnosed through observation of the eardrum’s response to breathing and swallowing, while obstructive ETD may be identified by the presence of negative pressure in the middle ear. Treatment for patulous ETD may include medications, surgery, or insertion of ear tubes, while obstructive ETD treatment options include medications, surgery, and pressure equalization techniques.
Home Remedies versus Medications
When dealing with eustachian tube dysfunction (ETD), individuals often face the choice between trying home remedies or using over-the-counter (OTC) medications to alleviate their symptoms. Both approaches have their advantages and disadvantages, which should be carefully considered before deciding on a course of treatment.
Pros and Cons of Home Remedies
Home remedies for ETD can be an attractive option for many people, as they are generally safe, easily accessible, and cost-effective. Some common home remedies include:
- Chewing gum or yawning to help open the eustachian tubes
- Using a saline nasal spray to clear nasal passages
- Performing the Valsalva maneuver (gently blowing out while pinching the nostrils closed)
The main advantage of home remedies is that they are non-invasive and carry minimal risk of side effects. They can be particularly useful for managing mild symptoms or preventing ETD in certain situations, such as during air travel.
However, home remedies may not be effective for everyone, especially those with more severe or persistent symptoms. Additionally, some remedies, such as the Valsalva maneuver, can potentially cause further complications if performed incorrectly or too forcefully.
Pros and Cons of OTC Medications
OTC medications, such as pain relievers, decongestants, and antihistamines, can provide more targeted relief for ETD symptoms. Acetaminophen and ibuprofen can help manage pain and inflammation, while decongestants like pseudoephedrine can reduce swelling in the nasal passages and eustachian tubes.
The primary benefit of OTC medications is their ability to offer faster and more effective symptom relief compared to home remedies. They can be particularly useful for individuals with moderate to severe ETD or those who need quick relief to carry out daily activities.
However, OTC medications also come with potential drawbacks. Some medications may cause side effects, such as drowsiness, dry mouth, or increased blood pressure. Overuse of decongestants can lead to rebound congestion, worsening symptoms in the long run. It is crucial to follow the recommended dosage and consult with a healthcare professional if symptoms persist or worsen.
Ultimately, the choice between home remedies and OTC medications for ETD depends on the severity of symptoms, individual preferences, and any underlying health conditions. In some cases, a combination of both approaches may be most effective. If symptoms do not improve with home remedies or OTC treatments, it is essential to seek medical advice for further evaluation and potential prescription treatments.
Surgical Interventions Comparison
When conservative treatments fail to alleviate the symptoms of eustachian tube dysfunction (ETD), surgical interventions may be considered. The primary goal of surgical treatment is to bypass the eustachian tube and re-establish ventilation of the middle ear. This can restore hearing, relieve pressure sensations, and reduce the tendency for middle ear infections.
Myringotomy vs. Pressure Equalization Tubes
Myringotomy involves making a tiny incision in the eardrum and suctioning out any fluid within the middle ear. In adults, the incision often stays open long enough to allow the swelling in the eustachian tube lining to resolve. However, after the eardrum heals (usually within 1 to 3 days), the middle ear fluid may re-accumulate if the eustachian tube lining has not recovered.
Pressure equalization tubes, also known as tympanostomy tubes or grommets, are tiny hollow tubes made of plastic or metal that are inserted into the eardrum after making an incision and suctioning out any middle ear fluid. These tubes usually provide middle ear ventilation for 6 to 12 months. Often, the eustachian tube will have recovered by this time and the tubes need not be replaced. However, longer-lasting tubes are available for more chronic problems.
The major disadvantage of pressure equalization tubes is that water must be kept out of the ear, requiring the use of earplugs or a cotton ball smothered in petroleum jelly while bathing. Swimming usually requires custom earplugs fit individually to the patient’s ear. Water that gets into the ear canal can carry bacteria through the tube into the middle ear space and cause an ear infection, noted as a purulent drainage (white, green, or yellow pus) from the ear. This type of ear infection can be easily treated with antibiotic eardrops.
Another risk of either myringotomy or pressure equalization tubes is that the incision may not heal, which may eventually require surgery (tympanoplasty) to patch the hole.
Eustachian Tuboplasty Techniques
Eustachian tuboplasty refers to surgical procedures that aim to directly improve the function of the eustachian tube itself. Several techniques have been developed:
- Laser Eustachian Tuboplasty: This procedure uses a carbon dioxide or 980-nm diode laser to vaporize the mucosa and cartilage from the posterior luminal wall of the eustachian tube nasopharyngeal opening, with the goal of dilating the tube.
- Microdebrider Eustachian Tuboplasty: A microdebrider is used to remove hypertrophic mucosa and cartilage at the nasopharyngeal opening of the eustachian tube.
- Balloon Dilation Eustachian Tuboplasty (BDET): This minimally invasive procedure involves inserting a balloon catheter into the eustachian tube and inflating it with sterile water at a desired pressure for a predetermined time. The aim is to dilate the cartilaginous part of the eustachian tube without causing structural damage. BDET can be performed transnasally under endoscopic guidance or via a transtympanic route.
Eustachian tuboplasty techniques are emerging as promising alternatives to traditional tympanostomy tube placement for managing chronic ETD. However, more research is needed to establish their long-term efficacy and safety compared to established surgical treatments. The choice of surgical intervention depends on individual patient factors and the severity of ETD.
Short-Term versus Long-Term Management
The management of eustachian tube dysfunction (ETD) can be divided into short-term and long-term strategies. Short-term management focuses on providing immediate relief from symptoms, while long-term management aims to address the underlying causes and prevent recurrence.
Immediate Relief Options
When experiencing acute symptoms of ETD, such as ear pain, fullness, or muffled hearing, several techniques can provide temporary relief:
- Swallowing, yawning, or chewing gum: These actions help open the eustachian tubes and equalize pressure in the middle ear.
- Valsalva maneuver: Gently blowing out while pinching the nostrils closed can help open the eustachian tubes.
- Nasal decongestants: Over-the-counter decongestant sprays or oral medications can reduce inflammation and swelling in the nasal passages and eustachian tubes, providing short-term relief. However, prolonged use of decongestants should be avoided.
- Pain relievers: Acetaminophen or ibuprofen can help alleviate pain and discomfort associated with ETD.
Preventive Strategies
To manage ETD in the long term, it is essential to identify and address the underlying causes. Some preventive strategies include:
- Treating allergies: If allergies are contributing to ETD, managing them through medications, immunotherapy, or environmental modifications can help reduce inflammation and prevent recurrence.
- Managing acid reflux: Chronic acid reflux can cause inflammation in the throat and eustachian tubes. Treating reflux with lifestyle changes, medications, or surgery may be necessary to prevent ETD.
- Quitting smoking: Smoking can irritate the nasal passages and eustachian tubes, leading to inflammation and dysfunction. Quitting smoking can help improve ETD symptoms and prevent future episodes.
- Maintaining a healthy lifestyle: Engaging in regular exercise, maintaining a healthy weight, and staying hydrated can help promote overall health and reduce the risk of developing conditions that contribute to ETD.
In cases where conservative measures fail to provide relief or if ETD becomes chronic, surgical interventions such as myringotomy, pressure equalization tubes, or eustachian tube balloon dilation may be considered. These procedures aim to improve ventilation and drainage of the middle ear, reducing the likelihood of recurrent infections and hearing problems.
By combining short-term relief techniques with long-term preventive strategies and addressing any underlying conditions, individuals with ETD can effectively manage their symptoms and improve their quality of life.
Costs and Insurance Considerations
The cost of eustachian tube balloon dilation (ETBD) can vary depending on several factors, including the healthcare provider, location, and insurance coverage. According to MDsave, a healthcare marketplace that allows patients to compare prices and purchase procedures upfront, the national average cost for ETBD ranges from $5,863 to $13,079. For in-office ETBD procedures, the cost ranges from $3,501 to $4,485, with a national average of $4,157.
Patients with high deductible health plans or those without insurance can potentially save money by purchasing their procedure through platforms like MDsave. It is important for patients to discuss the costs associated with ETBD with their healthcare provider and insurance company to understand their coverage and out-of-pocket expenses.
Insurance coverage for ETBD may vary depending on the individual’s plan and the medical necessity of the procedure. Some insurance companies may consider ETBD to be investigational or not medically necessary, resulting in limited or no coverage. Patients should consult with their insurance provider to determine their specific coverage for ETBD and any associated costs, such as copayments, deductibles, and coinsurance.
In cases where insurance coverage is limited or unavailable, patients may need to explore alternative payment options, such as financing plans, medical credit cards, or payment assistance programs offered by healthcare providers or charitable organizations.
It is crucial for patients to carefully consider the costs and potential benefits of ETBD when making decisions about their treatment options for eustachian tube dysfunction. Discussing the financial aspects of the procedure with healthcare providers and insurance representatives can help patients make informed decisions and plan accordingly for the associated expenses.
Conclusion and Recommendations
Eustachian tube dysfunction is a common condition that can significantly impact an individual’s quality of life. By understanding the different types of ETD, their causes, and the various treatment options available, patients can make informed decisions about their care. While home remedies and over-the-counter medications may provide relief for mild cases, more severe or chronic ETD may require surgical interventions, such as pressure equalization tubes or eustachian tuboplasty.
Effective management of ETD involves a combination of short-term symptom relief and long-term preventive strategies. Patients should work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs and concerns, including the costs and insurance considerations associated with various treatment options. By taking a proactive approach to managing ETD, individuals can minimize its impact on their daily lives and maintain optimal ear health.