Hiatal hernia is a common digestive condition that affects millions of people worldwide. This occurs when part of the stomach pushes through the diaphragm, the muscle that separates the chest from the abdomen. While some individuals with hiatal hernias may not experience any symptoms, others can face discomfort and complications that impact their daily lives.
Understanding the symptoms, diagnosis, and treatment options for hiatal hernias is crucial for those affected by this condition. This article aims to shed light on the key aspects of hiatal hernias, including common signs to watch out for, how doctors diagnose the problem, and the various approaches to manage and treat it. By exploring these topics, readers will gain valuable insights to help them navigate this health issue more effectively.
Understanding Hiatal Hernia
A hiatal hernia is a protrusion of the abdominal contents into the thorax through an enlarged esophageal hiatus caused by a weakness or opening in the diaphragm. The upper part of the stomach usually protrudes upwards, but it can also be the small intestine, transverse colon, or omentum.
Definition and Types
Hiatal hernias are classified into four different types:
- Type I (sliding type) – The most common type, accounting for more than 95% of hiatal hernias. The gastro-oesophageal junction slides up into the thorax, and the acute angle between the esophagus and stomach disappears.
- Type II (pure para-oesophageal junction hernia or rolling hernia) – The gastro-oesophageal junction stays in its normal anatomical position, but the fundus of the stomach protrudes up through the diaphragm next to the oesophagus.
- Type III (mixed type) – A combination of Type I and II, where both the gastro-oesophageal junction and fundus protrude through the hiatus.
- Type IV (giant hiatal hernia) – More than one-third or one-half of the stomach or any other abdominal organ or structure herniates through the diaphragm.
RELATED: Cystic Fibrosis: Detailed Insights into Symptoms and Treatments
Causes and Risk Factors
Hiatal hernias may be congenital or acquired, with an increased prevalence in older people. Muscle weakness with loss of flexibility and elasticity with age predisposes to the development of a hiatal hernia. Other predisposing factors include:
- Elevated intraabdominal pressure due to obesity, pregnancy, chronic constipation, and chronic obstructive pulmonary disease (COPD)
- Trauma
- Previous surgeries
- Genetics
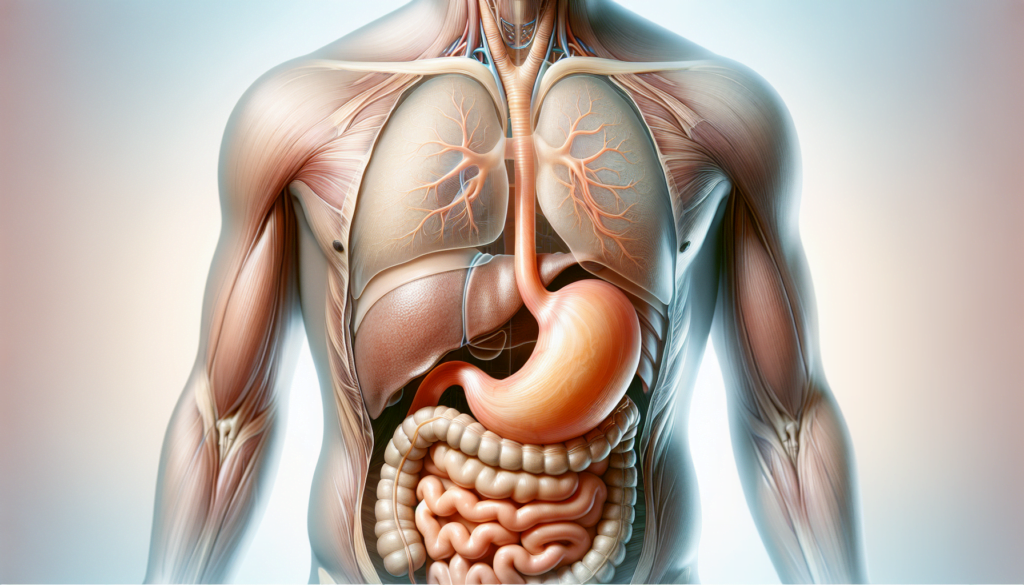
Anatomy of a Hiatal Hernia
The diaphragm is a muscular structure that assists in respiration and has a small opening, a hiatus, through which the esophagus passes prior to connecting to the stomach at the gastroesophageal junction (GEJ). In a hiatal hernia, the stomach pushes through that opening and into the chest, compromising the lower esophageal sphincter (LES). This laxity of the LES can allow gastric content and acid to back up into the esophagus, leading to gastroesophageal reflux disease (GERD).
Common Symptoms of Hiatal Hernia
Many people with hiatal hernias don’t experience any symptoms. However, when symptoms do occur, they are often related to acid reflux (gastroesophageal reflux disease, or GERD). The most common symptoms include:
Heartburn and Acid Reflux
Heartburn, a burning sensation in the chest, is a frequent symptom of hiatal hernias. This occurs when stomach acid flows back into the esophagus, causing irritation and discomfort. Heartburn may worsen after eating, especially when lying down or bending over. Other related symptoms include:
- Regurgitation of food or liquids into the mouth
- Backflow of stomach acid into the esophagus
- A foul, acidic taste in the mouth
- Difficulty swallowing or a lump-like sensation in the throat
- Chronic sore throat and hoarseness due to acid irritation
Chest Pain and Discomfort
Hiatal hernias can cause chest pain that may mimic the pain associated with a heart attack. This noncardiac chest pain is often recurring and can be accompanied by a feeling of pressure or fullness in the chest. The pain may also radiate to the upper abdomen or lower chest.
Other Associated Symptoms
In addition to heartburn and chest pain, hiatal hernias may cause other symptoms, such as:
- Nausea and vomiting, due to stomach compression or acid overflow
- Shortness of breath, if the hernia compresses the lungs
- Bloating and burping
- Indigestion, characterized by a feeling of fullness soon after eating and a burning abdominal pain
It’s important to note that the severity and frequency of symptoms can vary from person to person. Some individuals may experience mild, occasional discomfort, while others may have more severe and persistent symptoms that significantly impact their daily lives. If you experience any of these symptoms, especially if they are severe or persistent, it’s essential to consult with a healthcare provider for proper diagnosis and treatment.
Diagnosis Methods for Hiatal Hernia
Diagnosing a hiatal hernia often involves a combination of physical examination, imaging tests, and endoscopic procedures. While a physical exam alone is usually not sufficient to confirm the presence of a hiatal hernia, it can provide important clues and help rule out other conditions. Healthcare providers rely on various diagnostic tools to accurately identify and assess the severity of a hiatal hernia.
Physical examination of patients with a hiatal hernia is usually normal and unhelpful in the diagnosis. In some cases, a hiatal hernia may develop into gastroesophageal reflux disease (GERD), and patients with GERD usually appear ill due to the pain. Common physical examination findings in GERD include hoarseness of voice, laryngitis, otitis media, and lung wheezes.
Imaging tests play a crucial role in diagnosing hiatal hernias. Plain chest radiographs may demonstrate a retrocardiac gas-filled structure, indicating the presence of a hernia. However, an upper GI barium series is the preferred examination for investigating suspected hiatal hernias and their sequelae. This test involves drinking a chalky liquid containing barium sulfate, which coats the esophagus and stomach, making them visible on X-rays. CT scans are useful when more precise cross-sectional anatomic localization is desired, particularly in cases of totally intrathoracic stomach or when staging is needed for patients with carcinoma complicating a hiatal hernia.
Endoscopy is another key diagnostic modality in assessing patients with hiatal hernias. An upper GI endoscopy involves inserting a flexible tube with a light and camera (endoscope) down the throat to visualize the esophagus and stomach. This procedure can help establish the diagnosis of esophagitis and hiatal hernia while excluding other esophageal pathologies such as ulceration, stricture, Barrett’s esophagus, or malignancy. Endoscopy is particularly helpful in evaluating patients who develop symptoms after antireflux surgery, as it allows the physician to define the normal appearances for various antireflux surgeries and recognize postoperative problems.
RELATED: Diabetes Overview: Key Symptoms, Causes, and Treatments
Other diagnostic procedures that may be used in conjunction with endoscopy include pH monitoring to check for stomach acid in the esophagus, esophageal manometry to measure the functionality of the esophagus, and a barium swallow test (also known as an esophagogram or upper GI series) to visualize the esophagus and stomach using fluoroscopic X-rays.
In summary, diagnosing a hiatal hernia requires a multi-faceted approach that combines physical examination, imaging studies, and endoscopic procedures. By utilizing these diagnostic methods, healthcare providers can accurately identify the presence and severity of a hiatal hernia, allowing for the development of an appropriate treatment plan tailored to the individual patient’s needs.
Treatment Options for Hiatal Hernia
The treatment for hiatal hernia depends on the severity of symptoms and the size of the hernia. While some people may not require any treatment, others may need a combination of lifestyle changes, medications, and in some cases, surgical interventions to manage their symptoms effectively.
Lifestyle Changes
Making certain lifestyle modifications can help alleviate the symptoms associated with hiatal hernia. These changes include:
- Eating smaller, more frequent meals throughout the day instead of three large meals
- Avoiding lying down or going to bed immediately after eating
- Elevating the head of the bed by 6-8 inches to prevent acid reflux while sleeping
- Maintaining a healthy weight through a balanced diet and regular exercise
- Avoiding trigger foods such as spicy or fatty foods, citrus fruits, tomatoes, chocolate, and caffeine
- Quitting smoking and limiting alcohol consumption
Incorporating these lifestyle changes into daily routines can significantly reduce the frequency and severity of hiatal hernia symptoms.
Medications
For individuals experiencing mild to moderate symptoms, medications may be prescribed to manage acid reflux and heartburn. Some common medications include:
- Antacids: These over-the-counter medications neutralize stomach acid, providing quick relief from heartburn and indigestion.
- H2 receptor blockers: These drugs, such as famotidine and cimetidine, reduce the production of stomach acid, offering longer-lasting relief compared to antacids.
- Proton pump inhibitors (PPIs): PPIs, including omeprazole and lansoprazole, are stronger acid-suppressing medications that can effectively treat chronic acid reflux and allow the esophagus to heal.
It is essential to consult with a healthcare provider before starting any medication to ensure proper dosage and to avoid potential side effects or interactions with other medications.
RELATED: Dyslexia Explained: A Comprehensive Guide for Parents and Teachers
Surgical Interventions
In cases where lifestyle changes and medications do not provide adequate relief, or when the hiatal hernia is large and causing severe symptoms, surgical intervention may be necessary. The most common surgical procedures for hiatal hernia include:
- Nissen fundoplication: This procedure involves wrapping the upper part of the stomach around the lower esophagus to strengthen the sphincter and prevent acid reflux. It is typically performed laparoscopically, resulting in smaller incisions and faster recovery times.
- Laparoscopic hiatal hernia repair: During this minimally invasive procedure, the surgeon repositions the herniated portion of the stomach back into the abdomen and tightens the diaphragmatic opening to prevent future herniation.
The choice of surgical procedure depends on the individual’s specific condition and the surgeon’s expertise. Recovery time varies, but most people can return to normal activities within a few weeks following surgery.
In conclusion, the treatment for hiatal hernia aims to manage symptoms and improve quality of life. By implementing lifestyle changes, using medications when necessary, and considering surgical options in severe cases, individuals with hiatal hernia can effectively control their symptoms and prevent complications.
Conclusion
Hiatal hernias have a significant impact on many individuals’ lives, causing discomfort and potential complications. Understanding the symptoms, diagnosis methods, and treatment options is crucial to manage this condition effectively. From lifestyle changes and medications to surgical interventions, there are various approaches to address hiatal hernias and improve quality of life. The choice of treatment depends on the severity of symptoms and the size of the hernia.
To wrap up, this article has provided a comprehensive overview of hiatal hernias, covering their types, causes, symptoms, diagnosis, and treatment options. By exploring these aspects, readers can gain valuable insights to help them navigate this health issue more effectively. Whether dealing with mild symptoms or considering surgical options, being well-informed about hiatal hernias is key to making informed decisions about one’s health and well-being.