Actinic keratosis is a common skin condition that affects millions of people worldwide. It occurs when the skin has been damaged by years of sun exposure, leading to the development of rough, scaly patches. These patches, often found on areas frequently exposed to the sun like the face, ears, and hands, can be a precursor to skin cancer if left untreated.
This guide aims to provide a comprehensive overview of actinic keratosis. It will cover the essential aspects of understanding the condition, including its causes and risk factors. The article will also explore the diagnosis process, available treatment options, and effective prevention strategies. By the end, readers will have a clear understanding of how to manage and prevent this potentially serious skin condition.
Understanding Actinic Keratosis



Actinic keratosis (AK) is a common skin condition that affects millions of people worldwide. It occurs when the skin has been damaged by years of sun exposure, leading to the development of rough, scaly patches. These patches, often found on areas frequently exposed to the sun like the face, ears, and hands, can be a precursor to skin cancer if left untreated.
What is Actinic Keratosis?
Actinic keratoses are premalignant cutaneous lesions that may progress to squamous cell carcinoma. They commonly appear on sun-exposed areas of the skin in individuals with a history of cumulative sun exposure. AKs are caused by ultraviolet (UV) damage to the skin, which can disrupt regulatory pathways involved in cell growth and differentiation, leading to the intraepidermal proliferation of dysplastic keratinocytes.
RELATED: Lichen Sclerosus: A Detailed Guide to Understanding and Treating
Causes and Risk Factors
Chronic unprotected exposure to UV radiation is the leading cause of actinic keratosis. The UV rays emitted by indoor tanning beds are especially dangerous in raising the risk of developing AKs. Other risk factors include:
- History of unprotected sun exposure or sunburns
- Living in a geographic location closer to the equator
- Having a weakened immune system due to medical conditions or medications
- Having light skin, blonde or red hair, and blue, green, or gray eyes
- Being over the age of 40
Signs and Symptoms
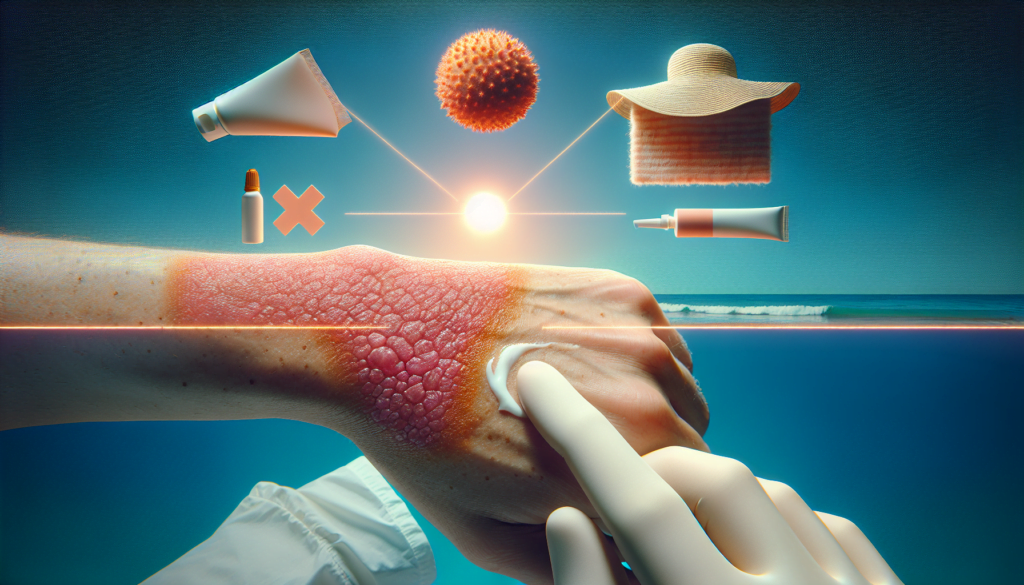
Actinic keratoses can present in various forms, such as scaly, erythematous macules, papules, plaques, or cutaneous horns. They may appear as rough, dry, or scaly patches of skin, usually less than 1 inch in diameter. AKs can be flat to slightly raised, with color variations including pink, red, or brown. Some AKs may itch, burn, bleed, or crust over. It is essential to have any new or changing skin lesions evaluated by a healthcare provider, as it can be difficult to distinguish between noncancerous and cancerous growths.
Diagnosis of Actinic Keratosis
Actinic keratosis (AK) is often diagnosed based on its clinical features. A primary care provider or dermatologist can establish the diagnosis through a comprehensive review of the patient’s medical history and a thorough physical examination. The doctor will assess risk factors such as prolonged outdoor work or sports without adequate sun protection.
During the physical exam, the doctor will carefully evaluate the skin condition and any presenting lesions. A dermatoscope, an optical instrument similar to a magnifying glass with light, may be used to examine the lesions in more detail. This technique, known as dermoscopy, allows the doctor to observe the lesions below the skin’s surface and obtain a magnified image.
Visual Examination
In many cases, actinic keratosis can be diagnosed through a visual examination by a trained healthcare professional. The lesions typically appear as rough, scaly patches on sun-exposed areas of the skin, such as the face, ears, and hands. They may be flat or slightly raised and can vary in color from pink to red or brown.
Dermoscopy
Dermoscopy is a non-invasive diagnostic technique that involves the use of a dermatoscope to examine skin lesions more closely. This tool allows the doctor to visualize structures beneath the skin’s surface that are not visible to the naked eye. Dermoscopy can help differentiate actinic keratosis from other skin conditions and aid in determining whether a biopsy is necessary.
RELATED: Laryngitis Treatment: Medical and Home Remedies
Skin Biopsy
In some cases, a skin biopsy may be performed to confirm the diagnosis of actinic keratosis, especially when the lesion has an atypical appearance or if there is suspicion of skin cancer. During a biopsy, a small sample of the affected skin is removed and sent to a laboratory for microscopic examination by a pathologist.
It is crucial to differentiate between actinic keratosis and invasive squamous cell carcinoma (SCC). Although the risk of an AK lesion progressing to SCC is low, early diagnosis and treatment are essential to prevent the development of this potentially invasive skin cancer. Certain factors, such as inflammation, ulceration, rapid growth, or a lack of response to treatment, may raise suspicion of SCC. In these cases, a biopsy is typically recommended.
Individuals with a history of actinic keratosis or those at higher risk for skin cancer should undergo regular skin examinations by a dermatologist. Early detection and prompt treatment of AK lesions can significantly reduce the risk of progression to squamous cell carcinoma.
Treatment Options
There are several treatment options available for actinic keratosis, including topical medications, cryotherapy, photodynamic therapy, and surgical procedures. The choice of treatment depends on factors such as the number, size, and location of the lesions, as well as the patient’s age, health status, and preferences.
Cryotherapy
Cryotherapy involves freezing the actinic keratosis with liquid nitrogen. The procedure is quick and effective, but may cause temporary pain, redness, and blistering. It is best suited for treating a small number of isolated lesions.
RELATED: All About Kidney Infection (Pyelonephritis): Your Questions Answered
Photodynamic Therapy
Photodynamic therapy (PDT) involves applying a light-sensitizing agent to the skin and then exposing it to a specific wavelength of light. The light activates the agent, causing it to destroy the abnormal cells. PDT can treat multiple actinic keratoses in a single session and may provide cosmetic benefits.
Surgical Procedures
Surgical procedures, such as curettage (scraping) and electrodesiccation (burning), may be used to remove individual actinic keratoses. These methods are effective but can cause scarring and are not practical for treating multiple lesions.
In some cases, a combination of treatments may be recommended to achieve the best results. It is important to discuss the benefits and risks of each treatment option with a healthcare provider to determine the most appropriate approach for managing actinic keratosis.
Prevention and Long-term Management
The best approach to prevent actinic keratosis is to minimize exposure to ultraviolet (UV) radiation. This can be achieved through various sun protection strategies:
- Use broad-spectrum sunscreen with an SPF of 30 or higher daily, even on cloudy days. Apply it 15 minutes before sun exposure and reapply every 2 hours or more frequently if sweating or swimming.
- Avoid peak sun hours between 12 and 4 pm when UV rays are strongest.
- Wear protective clothing such as thick, dark-colored garments, wide-brimmed hats, and UV-protective clothing.
- Avoid tanning salons and tanning booths, as they emit harmful UV radiation.
Regular Skin Checks
Regularly examining your skin allows you to notice any changes or the appearance of new actinic keratosis lesions. If you detect any suspicious changes, such as a new lesion or changes in size or shape of an existing one, consult your dermatologist promptly for evaluation.
Lifestyle Modifications
Adopting healthy lifestyle habits can further reduce the risk of developing actinic keratosis:
- Limit sun exposure during peak hours
- Seek shade whenever possible
- Incorporate vitamin B3 (niacinamide) into your diet, as it may help reduce the number of actinic keratoses
Conclusion
Actinic keratosis has a significant impact on skin health and can potentially lead to more serious conditions if left untreated. This guide has shed light on the causes, diagnosis, and treatment options available to manage this common skin condition. By understanding the risk factors and recognizing the signs, individuals can take proactive steps to protect their skin and seek timely medical attention.
To wrap up, prevention remains the key to maintaining healthy skin and reducing the risk of actinic keratosis. Regular skin checks, consistent use of sun protection, and lifestyle adjustments are crucial to minimize UV exposure. With proper care and awareness, individuals can effectively manage actinic keratosis and promote long-term skin health.