Prostatitis is a common and often misunderstood condition that affects millions of men worldwide. This inflammatory disorder of the prostate gland can cause a range of uncomfortable symptoms, significantly impacting a man’s quality of life. Despite its prevalence, many individuals lack awareness about the different types of prostatitis, their signs, and available treatment options.
This comprehensive overview aims to shed light on prostatitis, its various forms, and the telltale signs that may indicate its presence. Readers will gain insights into the four distinct types of prostatitis, each with its unique characteristics and challenges. The article will also explore the wide array of treatment approaches, from antibiotics and pain management to lifestyle changes and alternative therapies, helping men and their healthcare providers make informed decisions about managing this condition effectively.
What is Prostatitis? An Overview
Prostatitis is an inflammation or infection of the prostate gland that presents as several syndromes with varying clinical features. The term prostatitis is defined as microscopic inflammation of the tissue of the prostate gland and is a diagnosis that spans a broad range of clinical conditions. The National Institutes of Health (NIH) has recognized and defined a classification system for prostatitis in 1999, which includes four syndromes: acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CPPS), and asymptomatic inflammatory prostatitis.
Definition and Prevalence
Prostatitis is a common condition that affects millions of men worldwide. It is estimated that the prevalence of prostatitis amongst men in North America, Europe, and Asia is between 2-10%. In the United States, prostatitis accounts for nearly 2 million outpatient visits per year and is diagnosed in approximately 25% of male patients presenting with genitourinary symptoms. Autopsy studies have revealed a histologic prevalence of prostatitis of 64-86%, and approximately 8.2% of men have prostatitis at some point in their lives.
RELATED: Understanding Norovirus: Key Symptoms and Treatment Options
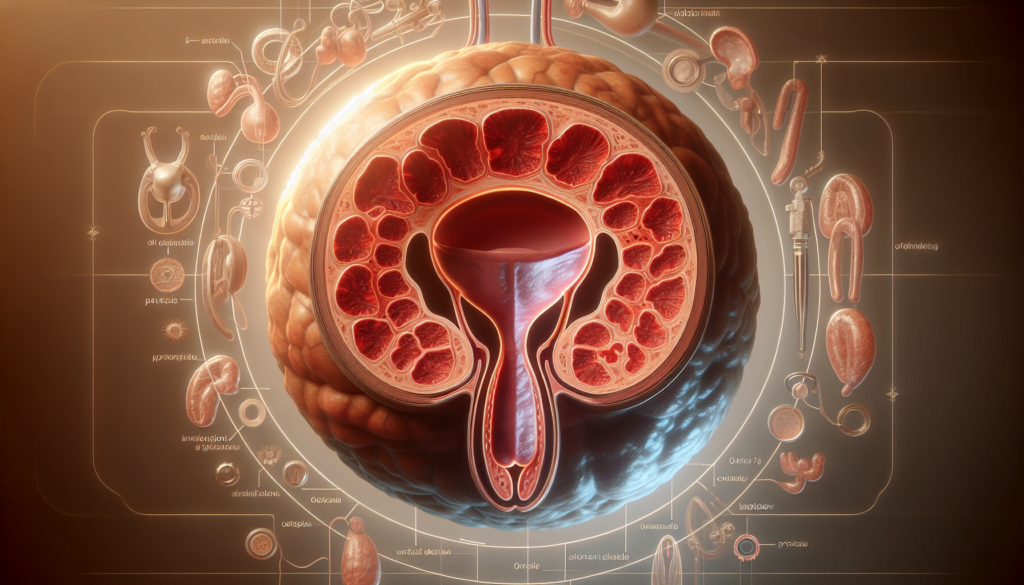
Anatomy of the Prostate
The prostate is a small gland that is part of the male reproductive system. It is located below the bladder and in front of the rectum in men and people assigned male at birth (AMAB). The prostate consists of connective tissues and glandular tissues and adds fluid to semen. Its muscles also help push semen through the urethra during ejaculation.
Risk Factors for Prostatitis
Several factors can increase the risk of developing prostatitis. A history of sexually transmitted diseases is associated with an increased risk for prostatitis symptoms. Other risk factors include:
- Age: In patients younger than 35 years, the most common variant of the syndrome is acute bacterial prostatitis. Among older patients, nonbacterial prostatitis (NIH types II and IV) are the most common.
- Urinary tract abnormalities: Functional or structural bladder pathology, such as primary vesical neck obstruction, pseudodyssynergia, impaired detrusor contractility, or acontractile detrusor muscle, can increase the risk of prostatitis.
- Immune system disorders: HIV-related disease is predominantly seen in younger patients and can lead to prostatitis caused by viral and fungal pathogens.
- Catheterization: Nursing home patients with indwelling urethral catheters may be at increased risk for acute bacterial prostatitis.
Understanding the definition, prevalence, anatomy, and risk factors associated with prostatitis is crucial for the accurate diagnosis and effective management of this condition.
The Four Types of Prostatitis Explained
Prostatitis can be classified into four distinct categories based on the National Institutes of Health (NIH) classification system:
- Acute Bacterial Prostatitis (NIH Category I): This is a Gram-negative infection of the prostate, most commonly caused by E. coli. It is associated with systemic signs of infection such as fever, chills, and malaise, as well as urinary tract symptoms like dysuria and urinary frequency. Men aged 20 to 40 are often affected, although the incidence increases around 60. Risk factors include frequent unprotected sexual intercourse, urinary tract instrumentation, and transrectal prostate biopsies.
- Chronic Bacterial Prostatitis (NIH Category II): This condition involves chronic urogenital pain with evidence of an ongoing urinary tract infection. Symptoms persist for at least 3 months and patients often have a history of recurrent UTIs caused by the same microorganisms. Among all men with chronic prostatitis symptoms, only about 5% to 10% have chronic bacterial prostatitis.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (NIH Category III): Formerly called prostatodynia, this is defined as recurrent or chronic genitourinary, prostatic, or pelvic pain without evidence of a urinary tract infection. It is the most common form of chronic prostatitis, accounting for about 90% of all cases. CP/CPPS is further subdivided into inflammatory (NIH Category IIIa) and non-inflammatory (NIH Category IIIb) based on the presence or absence of significant leukocytes in prostatic fluid.
- Asymptomatic Inflammatory Prostatitis (NIH Category IV): This condition is characterized by histological evidence of inflammation in a biopsy sample or positive findings of excessive WBCs in prostatic fluid in patients without any symptoms. It is primarily an incidental histological diagnosis and generally needs no treatment. About 70% of men have asymptomatic inflammatory prostatitis on prostate histological examinations at autopsy.
Identifying Prostatitis: Signs and Symptoms
Prostatitis can manifest through a range of symptoms, which may vary depending on the type and underlying cause. It is crucial to recognize these signs and seek medical attention for an accurate diagnosis and appropriate treatment. The primary symptoms of prostatitis can be categorized into urinary symptoms, pain and discomfort, sexual dysfunction, and systemic symptoms.
Urinary Symptoms
One of the most common indicators of prostatitis is a change in urinary habits. Patients may experience frequent urges to urinate, especially at night (nocturia). They may also have difficulty starting or maintaining a steady stream of urine, often accompanied by a burning sensation or pain during urination (dysuria). In some cases, there may be blood in the urine (hematuria) or a feeling of incomplete bladder emptying.
RELATED: All About Meningitis: Symptoms, Causes, and Effective Treatments
Pain and Discomfort
Prostatitis can cause significant discomfort in the pelvic region. Patients may experience pain in the lower abdomen, groin, or perineum (the area between the scrotum and anus). This pain can range from mild to severe and may radiate to the lower back or rectum. Sitting for extended periods may exacerbate the discomfort, while some men find relief by sitting on a donut-shaped cushion.
Sexual Dysfunction
Prostatitis can have a significant impact on sexual function. Men with prostatitis may experience painful ejaculation, decreased libido, and erectile dysfunction. These symptoms can lead to emotional distress and relationship strain, making it essential to address them with a healthcare provider.
Systemic Symptoms
In cases of acute bacterial prostatitis, patients may experience flu-like symptoms, such as fever, chills, body aches, and fatigue. These systemic symptoms indicate a more severe infection that requires prompt medical attention and treatment with antibiotics.
Recognizing the signs and symptoms of prostatitis is the first step in seeking appropriate medical care. By understanding the various manifestations of this condition, men can take proactive measures to manage their health and improve their quality of life.
Comprehensive Treatment Approaches for Prostatitis
Prostatitis treatment has an impact on several aspects, including medication, physical therapy, lifestyle changes, and psychological support. A multifaceted approach is often necessary to effectively manage the symptoms and improve quality of life.
Antibiotics are the primary treatment for acute and chronic bacterial prostatitis. The duration of antibiotic therapy ranges from 4 to 6 weeks or longer in some cases. For chronic nonbacterial prostatitis/chronic pelvic pain syndrome (CNP/CPPS), antibiotics may be tried initially to rule out occult infection.
Pain management is crucial in prostatitis treatment. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help alleviate pain and inflammation. Alpha-blockers may be prescribed to relax the muscles around the prostate and improve urinary symptoms. Anticholinergic agents like oxybutynin can be beneficial for men with irritative voiding symptoms.
Physical therapy techniques, including myofascial release, pelvic floor muscle exercises, and relaxation training, can be effective in managing prostatitis symptoms. These techniques help reduce muscle tension, improve blood flow, and promote healing. Regular exercise, such as walking or gentle stretching, can also aid in alleviating symptoms and improving overall well-being.
RELATED: Melanoma: Early Detection and Treatment Options Explained
Dietary modifications may play a role in managing prostatitis. Patients are often advised to avoid irritants like spicy foods, caffeine, and alcohol. Increasing fluid intake and consuming a diet rich in fruits, vegetables, and whole grains may help reduce inflammation and promote prostate health. Some men may benefit from supplements like quercetin, bee pollen, or saw palmetto, although more research is needed to confirm their efficacy.
Psychological support is an essential component of prostatitis treatment, as the condition can have a significant impact on mental health and quality of life. Stress management techniques, such as deep breathing exercises and meditation, can help patients cope with the emotional aspects of prostatitis. Counseling or support groups may also be beneficial for men struggling with the psychological impact of the condition.
A comprehensive, individualized treatment plan that addresses the specific needs and symptoms of each patient is crucial for effectively managing prostatitis. Close collaboration between healthcare providers, including urologists, primary care physicians, physical therapists, and mental health professionals, can ensure the best possible outcomes for men with this challenging condition.
Conclusion
Prostatitis is a complex condition that has a significant impact on men’s health and quality of life. This overview has shed light on the various types of prostatitis, their symptoms, and the wide range of treatment options available. Understanding the different forms of this disorder and recognizing its signs are crucial steps to seek timely medical attention and receive appropriate care.
Managing prostatitis often requires a multi-faceted approach, combining medical treatments with lifestyle changes and psychological support. By working closely with healthcare providers and exploring various treatment options, men with prostatitis can find relief from their symptoms and improve their overall well-being. Remember, each case is unique, and finding the right combination of treatments may take time and patience.