Leukoplakia is a condition that affects the mouth, causing white or gray patches to form on the tongue, gums, or inside of the cheeks. These patches can’t be rubbed off and may indicate an increased risk of oral cancer. While leukoplakia itself isn’t dangerous, it’s crucial to have any unusual changes in the mouth checked out by a healthcare professional.
This article delves into the various types of leukoplakia, helping readers to identify its symptoms and understand the diagnostic techniques used by doctors. It also explores the management strategies available to treat this condition, including lifestyle changes and medical interventions. By the end, readers will have a comprehensive understanding of leukoplakia and the steps to take if they suspect they might have it.
Types of Leukoplakia
There are several types of leukoplakia, each with distinct characteristics and potential for malignant transformation. The most common types include:
Homogeneous Leukoplakia
Homogeneous leukoplakia presents as uniformly white plaques that are usually asymptomatic. The patches may have a smooth, wrinkled, or ridged surface. This type of leukoplakia is typically benign and has a lower likelihood of transforming into malignancy compared to non-homogeneous leukoplakia.
Non-Homogeneous Leukoplakia
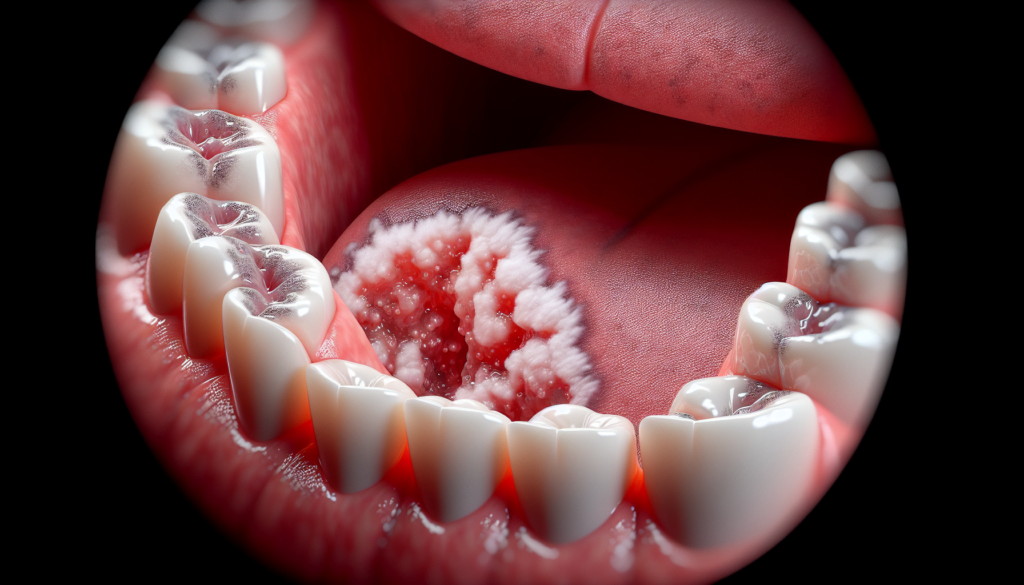
Non-homogeneous leukoplakia is characterized by irregular, flat, nodular, or exophytic white or red patches in the mouth. These lesions have a higher probability of malignant transformation, with studies suggesting that non-homogeneous leukoplakia is seven times more likely to become cancerous than the homogenous type.
RELATED: Thoracic Outlet Syndrome: Comprehensive Guide to Symptoms and Management
Proliferative Verrucous Leukoplakia (PVL)
PVL is a rare and aggressive subtype of leukoplakia that has the highest risk of malignant transformation. Some studies suggest that more than 60% of people with PVL develop oral cancer. PVL typically presents as small white patches that can grow rapidly and develop tiny lumps or bumps. The most commonly affected sites are the gingiva, buccal mucosa, and lateral border of the tongue.
Oral Hairy Leukoplakia
Oral hairy leukoplakia is a distinct type of leukoplakia that is strongly associated with Epstein-Barr virus (EBV) infection and immunosuppression, particularly in individuals with HIV/AIDS. It presents as white, hairy patches, often with folds resembling hair growing out of them. These lesions mostly occur on the tongue but can also appear in other parts of the mouth. Unlike other types of leukoplakia, oral hairy leukoplakia does not have the potential to become cancerous.
It is crucial for dental professionals to accurately diagnose and differentiate between these types of leukoplakia to provide appropriate management and monitoring for patients, as each type carries a different risk of malignant transformation.
Identifying Symptoms





Leukoplakia manifests as white or gray patches that develop on the tongue, gums, or the inside of the cheeks. These patches are usually slightly raised above the surrounding mucosa and cannot be rubbed off. Individuals with leukoplakia typically do not experience any symptoms, making it crucial for dental professionals to accurately identify and diagnose the condition during routine check-ups.
Visual Characteristics
Leukoplakia patches are characterized by their bright white appearance and sharply defined borders. The lesions may be uniformly white (homogeneous leukoplakia) or exhibit irregular, flat, nodular, or exophytic white or red patches (non-homogeneous leukoplakia). Proliferative verrucous leukoplakia (PVL), a rare and aggressive subtype, presents as small white patches that can grow rapidly and develop tiny lumps or bumps.
Texture and Sensation
The surface of leukoplakia patches can vary in texture, appearing smooth, wrinkled, or ridged. In most cases, these lesions are asymptomatic, meaning that patients do not experience any pain or discomfort. However, individuals with an underlying condition, such as cancer, may experience some pain associated with the patches.
RELATED: Thalassemias: Essential Information on Diagnosis and Treatment
Progression Over Time
Leukoplakia patches may change slowly over weeks to months. Dental professionals should closely monitor the progression of these lesions during regular check-ups. Any changes in the appearance of the patches, such as an increase in size or the development of red or dark regions, should be promptly evaluated, as they may indicate a higher risk of malignant transformation.
By understanding the visual characteristics, texture, and progression of leukoplakia lesions, dental professionals can more effectively identify and diagnose this potentially malignant disorder, enabling timely intervention and management to reduce the risk of oral cancer development.
Diagnostic Techniques
The gold standard for diagnosing leukoplakia is a biopsy from the lesion site, but this procedure requires a qualified healthcare provider and is considered invasive, painful, expensive, and time-consuming. For small lesions, an excisional biopsy is indicated, while for large lesions, an incisional biopsy, including the adjacent healthy tissue, is removed for histopathological examination.
Clinical Evaluation
During the clinical evaluation, a healthcare provider will examine the mouth and any unusual white patches. They will try to identify the cause of the symptoms. For example, if the patient uses dentures, the provider may check to ensure the dentures are not rubbing against the gums or the inside of the cheeks.
Imaging Studies
Other conventional clinical diagnostic tools for the timely detection of leukoplakia include toluidine blue dye, oral brush biopsy kits, salivary diagnostics, and optical imaging systems. In recent years, several new easy-to-use light sources and chairside diagnostic instruments have been advertised to dentists.
Histopathological Examination
The main histopathological changes seen in leukoplakia are:
- Keratinization of the epithelium (hyper ortho-keratinization or hyper para-keratinization)
- Increased thickness of the epithelium
- Acanthosis
- Thinning of the basement membrane
- Inflammatory component in the connective tissue
- Changes in the cellular layer, including:
- Increased nuclear-cytoplasmic ratio
- Hyperchromatic nuclei
- Nuclear hyperplasia
- Abnormal mitotic figures
- Increased mitosis
- Pleomorphic nuclei
- Basilar hyperplasia
- Drop-shaped rete pegs
- Loss of polarity
All suspected leukoplakia lesions should be biopsied, irrespective of the presence or absence of symptoms, clinical subtype (homogeneous or non-homogeneous), size, and oral subsite. In extensive leukoplakias, taking multiple biopsies (“mapping”) may be considered. Referral to a specialist for the biopsy procedure is advised, as most dentists are not trained to perform incisional or excisional biopsies.
Management Strategies
The management of leukoplakia involves a combination of non-invasive treatments, surgical approaches, and follow-up care. The choice of treatment depends on factors such as the size, location, and severity of the lesion, as well as the presence of dysplasia or malignancy.
Non-invasive treatments for leukoplakia include:
- Cessation of risk factors: Patients should be advised to quit smoking, reduce alcohol consumption, and avoid other known risk factors to prevent the progression or recurrence of leukoplakia.
- Nutritional supplements: Vitamin A, beta-carotene, lycopene, and other antioxidants may help in the resolution of leukoplakia lesions. However, their effectiveness is not well-established, and they should be used with caution due to potential side effects.
- Topical treatments: The application of topical agents such as bleomycin, vitamin A derivatives (retinoids), and photodynamic therapy (PDT) has shown some success in treating leukoplakia. These treatments aim to promote cell differentiation and reduce the risk of malignant transformation.
RELATED: Teratoma: Key Facts on Symptoms, Causes, and Treatment Options
Surgical approaches are considered when non-invasive treatments fail or when there is a high suspicion of malignancy. The main surgical options include:
- Conventional surgery: Complete excision of the lesion with adequate margins is the most common surgical approach. This method allows for histopathological examination of the entire lesion.
- Laser surgery: The use of CO2, Nd:YAG, or Er:YAG lasers can be an effective alternative to conventional surgery. Laser surgery offers advantages such as minimal bleeding, reduced postoperative pain, and faster healing.
- Cryosurgery: This technique involves the application of extreme cold to destroy abnormal tissue. It is less commonly used for leukoplakia due to the risk of scarring and difficulty in controlling the depth of tissue destruction.
Follow-up care is crucial for patients with leukoplakia, regardless of the treatment modality. Regular monitoring is necessary to detect any recurrence or malignant transformation. Patients should be advised to:
- Maintain good oral hygiene
- Attend regular dental check-ups
- Self-examine their oral cavity for any changes or new lesions
- Report any persistent or new symptoms to their healthcare provider promptly
In conclusion, the management of leukoplakia requires a multidisciplinary approach involving dental professionals, oral and maxillofacial surgeons, and pathologists. The goal of treatment is to prevent malignant transformation and maintain the patient’s quality of life.
Conclusion
Leukoplakia is a complex oral condition that requires careful attention and management. Understanding its various types, symptoms, and diagnostic techniques is crucial to address this potentially serious issue effectively. The comprehensive approach to diagnosing and treating leukoplakia, from clinical evaluations to advanced imaging studies, highlights the importance of early detection and intervention to prevent malignant transformation.
To wrap up, the management of leukoplakia involves a mix of non-invasive treatments and surgical approaches, tailored to each patient’s specific case. Regular follow-ups and lifestyle changes play a key role in preventing recurrence and maintaining oral health. By staying informed about leukoplakia and working closely with healthcare providers, individuals can take proactive steps to protect their oral health and overall well-being.