Periodontitis is a severe gum disease that affects millions of people worldwide. This condition goes beyond simple gum inflammation, causing damage to the soft tissue and bone that support the teeth. Left untreated, periodontitis can lead to tooth loss and has been linked to various systemic health issues, making it a significant concern for overall well-being.
Understanding the early signs, causes, and treatment options for periodontitis is crucial for maintaining oral health. This article delves into the progression of the disease, explores its underlying causes, and highlights the importance of recognizing early warning signs. Additionally, it examines comprehensive treatment approaches available to manage and prevent this serious dental condition.
The Progression of Periodontitis



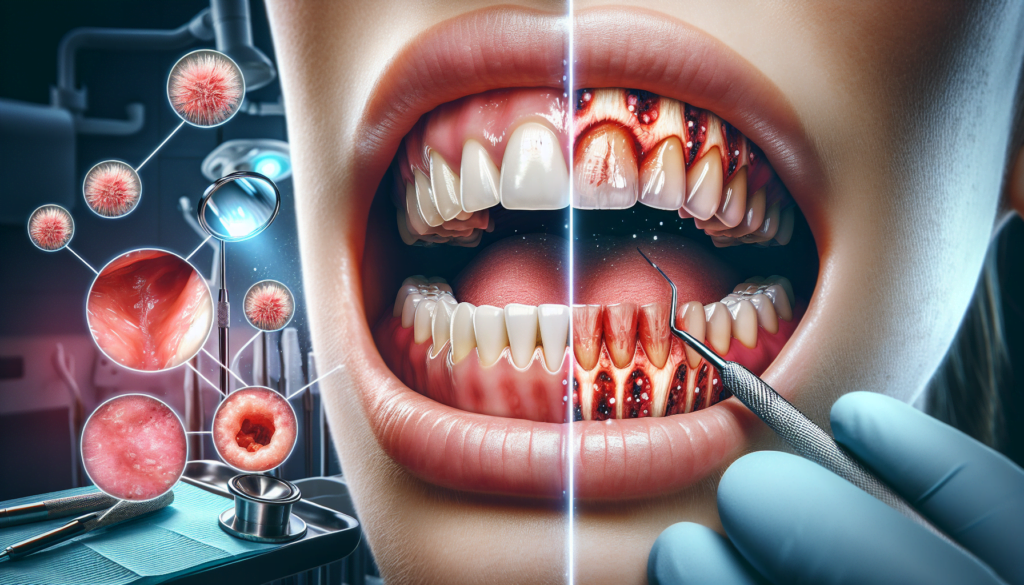
Periodontitis is a progressive disease that develops in stages, each characterized by specific symptoms and levels of severity. Understanding these stages is crucial for early detection and effective treatment.
Gingivitis Stage
Gingivitis, the mildest form of periodontal disease, is caused by the accumulation of dental plaque around the gum line. At this stage, the gums become inflamed, appearing red and swollen, and may bleed easily during brushing or flossing. Gingivitis is reversible with proper oral hygiene practices and professional dental cleanings.
Early Periodontitis
If gingivitis is left untreated, it can progress to early periodontitis. At this stage, the infection begins to affect the bone supporting the teeth, leading to the formation of periodontal pockets. These pockets allow bacteria to penetrate deeper into the tissues, triggering an immune response that can cause further damage to the periodontium. Treatment at this stage typically involves scaling and root planing to remove plaque and tartar buildup beneath the gum line.
RELATED: Dupuytren Contracture: Causes, Symptoms, and Modern Treatments
Moderate Periodontitis
Moderate periodontitis is characterized by significant bone loss and gum recession. Symptoms may include deep periodontal pockets, tooth mobility, and changes in bite alignment. Treatment at this stage may require a combination of scaling and root planing, antibiotic therapy, and surgical interventions to regenerate lost bone and gum tissue.
Advanced Periodontitis
Advanced periodontitis, the most severe stage of gum disease, is marked by extensive bone loss and tooth mobility. At this point, teeth may need to be extracted, and patients may require extensive reconstructive procedures to restore their oral health. Symptoms include severe pain, tooth loss, gum inflammation, and pus discharge.
Periodontitis progresses at different rates depending on various factors, such as oral hygiene habits, genetic predisposition, and systemic health conditions. Regular dental check-ups and early intervention are essential for preventing the progression of gum disease and maintaining optimal oral health.
Identifying Early Warning Signs
Detecting periodontitis in its early stages is crucial for effective treatment and preventing further damage to the gums and supporting structures. Several warning signs can indicate the onset of periodontal disease, allowing individuals to seek timely intervention from dental professionals.
Changes in Gum Appearance
One of the most noticeable early signs of periodontitis is a change in the appearance of the gums. Healthy gums should be firm, pale pink, and fit snugly around the teeth. However, in the early stages of periodontal disease, the gums may become swollen, red, and tender to the touch. They may also bleed easily during brushing or flossing, which is not normal for healthy gums.
Sensitivity and Pain
As periodontitis progresses, individuals may experience increased sensitivity and pain in their teeth and gums. This can be particularly noticeable when consuming hot or cold foods and beverages. The sensitivity is often due to the recession of the gums, which exposes the roots of the teeth. Additionally, the inflammation and infection associated with periodontitis can cause a dull, persistent ache in the gums.
RELATED: Cervical Cancer: Early Signs, Causes, and Treatment Options
Altered Bite and Tooth Alignment
Periodontitis can lead to changes in the way teeth fit together when biting down. As the disease advances, the supporting structures of the teeth become weakened, allowing the teeth to shift or become loose. This can result in a change in the bite, where teeth no longer make proper contact with each other. Individuals may also notice the formation of gaps or spaces between their teeth that were not previously present.
Persistent Bad Taste or Breath
Another warning sign of periodontitis is a persistent bad taste in the mouth or chronic bad breath (halitosis). The bacterial infection associated with periodontal disease produces toxins and byproducts that can cause an unpleasant taste and odor. Even with regular brushing and the use of mouthwash, the bad taste and breath may linger, indicating an underlying problem that requires professional attention.
Recognizing these early warning signs and promptly seeking dental care can significantly improve the chances of successful treatment and the preservation of oral health. Regular dental check-ups and maintaining good oral hygiene practices, such as brushing twice daily and flossing, can help detect periodontitis in its early stages and prevent its progression.
Underlying Causes of Periodontitis
The primary cause of periodontitis is bacterial infection. Specific bacteria, such as Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia, are strongly associated with the disease. These bacteria form a complex biofilm that adheres to tooth surfaces and invades the gingival tissue, leading to inflammation and destruction of the periodontium.
The host immune response plays a crucial role in the progression of periodontitis. In susceptible individuals, the immune system may overreact to the bacterial challenge, resulting in excessive inflammation and tissue damage. This dysregulated immune response involves the production of pro-inflammatory cytokines, such as interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and matrix metalloproteinases (MMPs), which contribute to the breakdown of connective tissue and alveolar bone.
Lifestyle factors significantly influence the development and severity of periodontitis. Smoking is a major risk factor, as it impairs the immune response and alters the composition of the oral microbiota. Poor oral hygiene, stress, and an unhealthy diet high in sugar and refined carbohydrates can also exacerbate the disease by promoting bacterial growth and reducing the body’s ability to fight infection.
Systemic diseases, such as diabetes and cardiovascular disease, have been linked to an increased risk of periodontitis. Diabetes, in particular, can impair the immune response and delay wound healing, making individuals more susceptible to periodontal infection. Conversely, the chronic inflammation associated with periodontitis may also contribute to the development and progression of systemic diseases.
In summary, the underlying causes of periodontitis involve a complex interplay between bacterial infection, the host immune response, lifestyle factors, and systemic health. Understanding these factors is crucial for the prevention, diagnosis, and effective management of this chronic inflammatory disease.
Comprehensive Treatment Approaches
Comprehensive treatment approaches for periodontitis involve a combination of non-surgical treatments, surgical interventions, regenerative procedures, and home care and lifestyle changes. The primary goal of these treatments is to halt the progression of the disease and restore periodontal health.
Non-surgical treatments, such as scaling and root planing, are often the first line of defense against periodontitis. These procedures involve the removal of plaque, calculus, and bacterial toxins from the tooth surfaces and beneath the gum line. Antimicrobial agents, such as chlorhexidine, may also be applied to the affected areas to reduce bacterial growth and promote healing.
In more advanced cases of periodontitis, surgical interventions may be necessary. Pocket reduction surgery involves folding back the gum tissue to remove bacteria and smooth the irregular surfaces of the damaged bone. This procedure helps to reduce the depth of periodontal pockets, making it easier to clean the teeth and prevent further damage.
RELATED: Clinical Depression: What You Need to Know About Major Depressive Disorder
Regenerative procedures, such as bone grafting and guided tissue regeneration, aim to regenerate lost bone and connective tissue. These procedures involve the use of bone grafts, membranes, and tissue-stimulating proteins to encourage the regrowth of lost periodontal structures.
Home care and lifestyle changes play a crucial role in the management of periodontitis. Good oral hygiene practices, such as brushing twice daily, flossing, and using an antimicrobial mouthwash, can help control plaque buildup and prevent further damage. Quitting smoking, maintaining a balanced diet, and managing stress are also important lifestyle factors that can impact periodontal health.
Conclusion
Periodontitis is a serious gum disease that has a significant impact on oral and overall health. Understanding its progression, early warning signs, underlying causes, and treatment options is key to maintaining healthy teeth and gums. By recognizing the symptoms early and seeking prompt dental care, individuals can prevent the disease from advancing to more severe stages that may lead to tooth loss and other complications.
Effective management of periodontitis involves a multi-faceted approach. This includes professional dental treatments, good oral hygiene practices, and lifestyle changes to reduce risk factors. Regular dental check-ups, combined with diligent home care, play a crucial role in preventing and managing this condition. By taking proactive steps to protect oral health, individuals can significantly lower their risk of developing periodontitis and enjoy better overall well-being.