Achalasia: A Disorder of the Esophagus is a rare condition that affects the ability of the esophagus to move food into the stomach. This disorder occurs when the lower esophageal sphincter fails to relax properly, leading to difficulties in swallowing and other digestive issues. Understanding achalasia is crucial for both patients and healthcare providers to ensure timely diagnosis and effective management of the condition.
Recent advancements in medical research have shed light on the pathogenesis, clinical presentation, and treatment options for achalasia of the esophagus. This article explores the underlying causes of this disorder, discusses the latest diagnostic tools, and examines personalized treatment approaches. By delving into these aspects, readers will gain valuable insights into managing this challenging digestive condition and improving the quality of life for those affected by it.
Achalasia Pathogenesis
The pathogenesis of achalasia involves a complex interplay of neurological, autoimmune, and genetic factors that lead to the degeneration of inhibitory neurons in the myenteric plexus of the esophagus. This loss of ganglion cells results in an imbalance between excitatory and inhibitory neurotransmission, causing impaired relaxation of the lower esophageal sphincter (LES) and aberrant peristalsis.
Neurological Factors
Achalasia is characterized by a selective loss of inhibitory ganglion cells in the myenteric plexus, which is associated with decreased production of nitric oxide (NO) and vasoactive intestinal peptide (VIP). These neurotransmitters are crucial for LES relaxation and normal esophageal peristalsis. Studies have shown that patients with achalasia have significantly lower levels of neuronal nitric oxide synthase (nNOS), VIP, and interstitial cells of Cajal (ICCs) in the LES compared to healthy controls. Animal models, such as the nNOS knockout mouse, have demonstrated that the absence of NO can lead to an achalasia-like phenotype with hypertensive LES and impaired relaxation.
RELATED: Gonorrhea: Essential Information on Symptoms, Causes, and Treatment
Autoimmune Theories
Inflammation and autoimmunity are thought to play a significant role in the development of achalasia. Histopathological studies have revealed inflammatory infiltrates, predominantly CD3+/CD45RO+ T cells and CD20+ B cells, around myenteric neurons in achalasia patients. The presence of autoantibodies against myenteric plexus neurons in the sera of achalasia patients further supports the autoimmune hypothesis. These autoantibodies have been shown to induce phenotypic and functional changes in myenteric neurons, reproducing the characteristics of the disease. Additionally, achalasia has been associated with other autoimmune disorders, such as Sjögren’s syndrome, type 1 diabetes, and rheumatoid arthritis.
Genetic Considerations
Genetic factors may contribute to the susceptibility of developing achalasia. Familial cases of achalasia and its association with specific genetic syndromes, such as Allgrove syndrome and multiple endocrine neoplasia type 2B, suggest a genetic component to the disease. Polymorphisms in genes related to immune regulation and neurodegeneration, such as HLA class II alleles, PTPN22, IL-23 receptor, and nitric oxide synthase (NOS) isoforms, have been linked to an increased risk of achalasia. However, the exact role of these genetic variations in the pathogenesis of achalasia remains to be elucidated.
In conclusion, the pathogenesis of achalasia involves a complex interaction between neurological, autoimmune, and genetic factors. The selective loss of inhibitory neurons in the myenteric plexus, accompanied by inflammation and autoimmunity, leads to the characteristic features of impaired LES relaxation and esophageal dysmotility. Further research is needed to better understand the underlying mechanisms and develop targeted therapies for this debilitating disorder.
Clinical Presentation
of Achalasia: A Disorder of the Esophagus – Treatment Options
Achalasia commonly presents with progressive dysphagia to solids and liquids, regurgitation of undigested food, chest pain, and weight loss. The mean duration of symptoms before diagnosis is often prolonged, ranging from 4.7 to 24 months.
Early vs. Late Symptoms
In the early stages, patients may experience dysphagia intermittently, particularly with solid foods. As the disease progresses, dysphagia becomes more frequent and occurs with liquids as well. Regurgitation of undigested food, especially during sleep, can lead to aspiration pneumonia. Chest pain, often mistaken for cardiac pain, is reported by 25-64% of patients. Significant weight loss is observed in 35-91% of patients at presentation.
RELATED: Bacterial Vaginosis: Symptoms, Causes, and Treatment Explained
Atypical Manifestations
Atypical symptoms are present in up to 61.7% of patients and can delay the diagnosis by an additional 6 months. These include heartburn (16.3%), vomiting (15.3%), belching (7.7%), and other gastrointestinal symptoms (43%). Misdiagnoses such as GERD (16.7%) and eosinophilic esophagitis (4%) are common. Non-gastrointestinal misdiagnoses involve ENT, psychiatric, neurologic, cardiologic, or thyroid diseases.
Pediatric Achalasia
In children, achalasia often presents atypically with recurrent pneumonia, nocturnal cough, hoarseness, and feeding difficulties. Up to 50% of children are initially misdiagnosed and treated for GERD or asthma, leading to a diagnostic delay of 6-10 years. Failure to thrive and eating disorders are common presentations in this age group.
Pitfalls in diagnosis include misinterpretation of symptoms like heartburn and nausea, tertiary contractions on barium swallow, hiatal hernias, reflux-like changes on endoscopy, and eosinophils in esophageal biopsies. A high index of suspicion and careful interpretation of diagnostic studies are essential to avoid delays in diagnosis and unnecessary interventions.
Advanced Diagnostic Tools
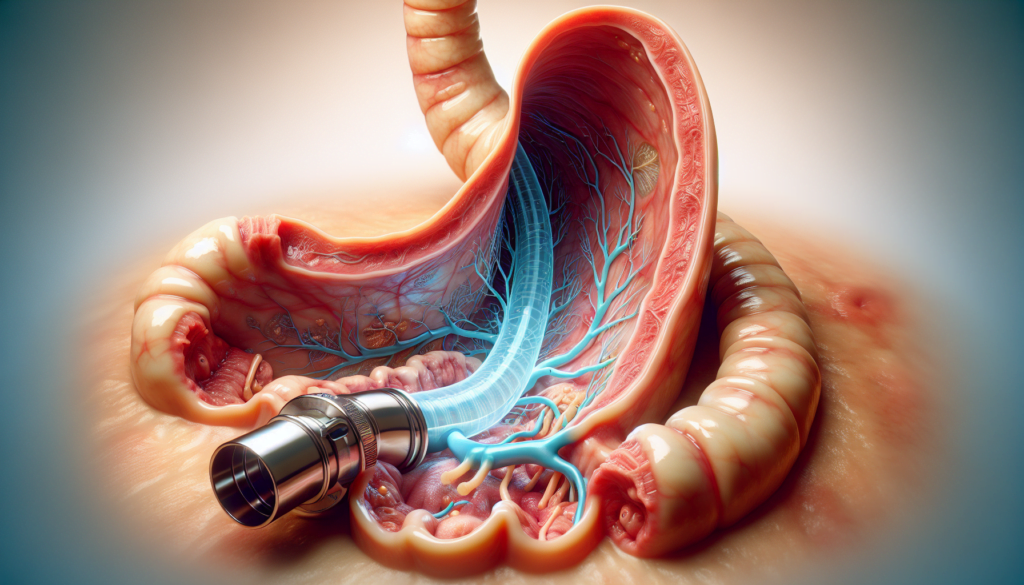
In recent years, advanced diagnostic tools have revolutionized the evaluation and management of achalasia. High-resolution manometry (HRM) and impedance planimetry have emerged as powerful techniques that provide detailed insights into esophageal motility and function.
HRM utilizes multiple closely spaced pressure sensors to generate a detailed pressure topography of the esophagus. This technology has improved the sensitivity and specificity of achalasia diagnosis by allowing for a more precise assessment of lower esophageal sphincter (LES) relaxation and esophageal body peristalsis. HRM has also led to the development of the Chicago Classification system, which categorizes achalasia into three subtypes based on the patterns of esophageal pressurization and contractility.
Impedance planimetry, also known as the functional lumen imaging probe (FLIP), measures the cross-sectional area and distensibility of the esophagus and LES. This technique provides valuable information about the mechanical properties of the esophagus and can help guide treatment decisions. Studies have shown that FLIP measurements correlate with treatment outcomes and can predict the response to endoscopic or surgical interventions.
Emerging technologies, such as 3D-HRM and high-frequency ultrasound, are also being explored for their potential applications in achalasia diagnosis. 3D-HRM combines HRM with impedance planimetry to generate a three-dimensional map of esophageal pressure and geometry. High-frequency ultrasound allows for a detailed visualization of the esophageal wall layers and can detect early changes in esophageal morphology.
The integration of these advanced diagnostic tools has significantly improved the understanding of achalasia pathophysiology and has facilitated personalized treatment approaches. By providing objective and quantitative data, these techniques enable clinicians to make informed decisions and optimize patient outcomes.
Personalized Treatment Approaches
Recent advances have enabled personalized treatment approaches for achalasia based on patient characteristics and disease subtypes. Careful patient selection is crucial for optimal outcomes. Factors such as age, comorbidities, achalasia subtype, and prior treatments influence the choice of therapy.
For patients with type I or II achalasia, POEM or pneumatic dilation may provide comparable symptomatic relief. However, for those with type III achalasia, a tailored POEM or laparoscopic Heller myotomy (LHM) is more effective than pneumatic dilation due to the ability to perform an extended myotomy.
Combination therapies are emerging as promising strategies to enhance treatment efficacy. For instance, combining POEM with an anti-reflux procedure like fundoplication can reduce the risk of post-procedure gastroesophageal reflux disease (GERD). Similarly, the sequential use of pneumatic dilation followed by POEM or LHM may improve outcomes in patients with persistent symptoms after initial therapy.
RELATED: How to Identify and Remove Tonsil Stones: A Complete Guide
Novel experimental treatments are under investigation to expand the therapeutic arsenal for achalasia. Techniques such as endoscopic stenting, neural cell transplantation, and electrical stimulation of the lower esophageal sphincter show potential but require further research before clinical implementation.
Personalized treatment approaches, considering patient factors and disease characteristics, are essential for optimizing outcomes in achalasia management. Combination therapies and novel experimental treatments may offer additional options for refractory cases or those seeking enhanced efficacy. As research advances, the future holds promise for increasingly tailored and effective achalasia therapies.
Conclusion
The management of achalasia has seen significant progress, with advanced diagnostic tools and personalized treatment approaches leading the way. High-resolution manometry and impedance planimetry have revolutionized the diagnosis and classification of this disorder, enabling healthcare providers to tailor treatments to individual patients. These advancements have a profound impact on patient outcomes, offering hope for improved quality of life for those grappling with this challenging condition.
Looking ahead, the future of achalasia treatment seems promising. Ongoing research into combination therapies and experimental treatments may open up new avenues to address refractory cases. As our understanding of the disorder deepens, we can expect more targeted and effective interventions to emerge. The key to success lies in continued collaboration between researchers, clinicians, and patients to further refine diagnostic techniques and treatment strategies, ultimately enhancing the care provided to those affected by achalasia.