Acute myeloid leukemia (AML) is a devastating blood cancer that affects thousands of lives each year. This aggressive form of leukemia develops rapidly in the bone marrow, disrupting the production of normal blood cells and causing a host of severe health issues. As medical research advances, understanding AML has become crucial for improving diagnosis, treatment, and patient outcomes.
This article delves into the complex world of acute myeloid leukemia, exploring its symptoms, causes, and current treatment approaches. Readers will gain insights into the risk factors associated with AML, learn to recognize early warning signs, and understand the diagnostic process. Additionally, the piece covers various treatment options available to patients and discusses strategies to manage side effects, providing a comprehensive overview of this challenging disease.
Understanding Acute Myeloid Leukemia
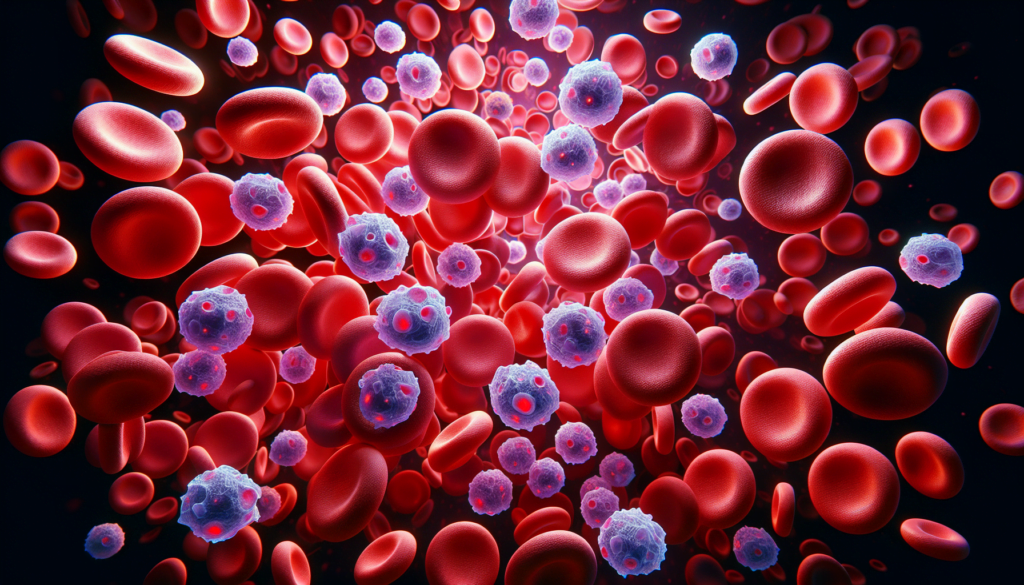
Acute myeloid leukemia (AML) is a devastating blood cancer that affects thousands of lives each year. This aggressive form of leukemia develops rapidly in the bone marrow, disrupting the production of normal blood cells and causing a host of severe health issues.
AML results when the DNA of a developing stem cell in the bone marrow becomes damaged, leading to an acquired mutation. This damaged cell becomes a leukemic cell and multiplies into billions of cells called leukemic blasts. These blasts do not function normally, blocking the production of healthy blood cells and growing and surviving better than normal cells.
As a result, the number of healthy blood cells is usually lower than normal, which can lead to various conditions such as anemia (low red blood cell count), neutropenia (low neutrophil count), thrombocytopenia (low platelet count), and pancytopenia (low counts of all three blood cell types).
RELATED: Bacterial Vaginosis: Symptoms, Causes, and Treatment Explained
The World Health Organization (WHO) classifies AML into several subtypes based on the genetic abnormalities in the leukemia cells and the percentage of myeloblasts present in the bone marrow and blood. These subtypes include:
- AML with certain genetic abnormalities (gene or chromosome changes)
- AML with myelodysplasia-related changes
- AML related to previous chemotherapy or radiation
- AML not otherwise specified (similar to the French-American-British classification)
Determining the subtype of AML is crucial as it plays a significant role in determining the type of treatment a patient will receive.
In addition to the subtype, several prognostic factors help doctors determine a person’s risk of the leukemia coming back after treatment and, therefore, if they should receive more or less intensive treatment. These factors include:
- Chromosome (cytogenetic) abnormalities
- Gene mutations
- Markers on the leukemia cells
- Age
- White blood cell count
- Prior blood disorders leading to AML
- Treatment-related AML
- Infection
- Leukemia cells in the central nervous system
- Status of AML after treatment
Understanding the complexities of AML, its subtypes, and prognostic factors is essential for improving diagnosis, treatment, and patient outcomes. As medical research advances, healthcare professionals and patients alike can work together to combat this challenging disease and provide hope for those affected by it.
Risk Factors and Causes
Acute myeloid leukemia (AML) is a complex disease that arises from a combination of genetic and environmental factors. While the exact causes of AML remain unknown, researchers have identified several risk factors that may increase an individual’s likelihood of developing this aggressive form of blood cancer.
Age and gender
AML can occur at any age, but it is more common in older adults. The median age at diagnosis is around 70 years old, with incidence rates increasing significantly after the age of 60. Additionally, AML exhibits a slight male predominance, with men being more likely to develop the disease than women.
Genetic predisposition
Inherited genetic conditions and familial predisposition play a role in AML development. Individuals with a twin, sibling, or parent diagnosed with AML have an increased risk of developing the condition themselves. Several genetic syndromes, such as Down syndrome, Fanconi anemia, Bloom syndrome, ataxia-telangiectasia, and Li-Fraumeni syndrome, are associated with a higher incidence of AML.
Environmental exposures
Exposure to certain environmental factors can significantly increase the risk of developing AML. These include:
- Smoking: Cigarette smoking is a well-established risk factor for various cancers, including AML. The cancer-causing substances in cigarette smoke can spread through the bloodstream and affect blood cell production. Current smokers have a 40% higher risk of developing AML compared to non-smokers.
- Chemical exposure: Long-term exposure to chemicals like benzene, which is present in cigarette smoke, rubbers, dyes, and pesticides, can alter cell function and induce blood cancers. Benzene exposure carries a 7-fold risk for developing leukemia, while benzene poisoning has a staggering 71-fold risk of causing AML.
- Prior cancer treatment: Individuals who have received chemotherapy or radiation therapy for other cancers are at an increased risk of developing AML. Certain chemotherapeutic agents, such as alkylating agents and topoisomerase II inhibitors, can cause genetic damage and lead to therapy-related AML. High doses of radiation exposure can also cause gene abnormalities, most commonly in chromosomes 5 and 7.
- Other blood disorders: Pre-existing blood disorders, such as myelodysplastic syndromes (MDS), myeloproliferative neoplasms (MPN), and aplastic anemia, can progress to AML over time. These conditions are characterized by abnormal blood cell production and function, which may eventually transform into leukemic cells.
- Obesity: Being overweight or obese creates a cellular environment that promotes inflammation and oxidative stress, which may contribute to the development of various cancers, including AML.
While these risk factors increase the likelihood of developing AML, it is essential to note that many individuals with one or more of these risk factors never develop the disease. Conversely, some people with no apparent risk factors may still be diagnosed with AML. As researchers continue to investigate the complex interplay between genetic and environmental factors, a clearer understanding of AML’s causes and risk factors will emerge, potentially leading to improved prevention and treatment strategies.
Recognizing AML Symptoms
The signs and symptoms of acute myeloid leukemia (AML) can be non-specific and resemble those of other common illnesses. However, it is essential to be aware of the potential indicators of this aggressive blood cancer.
Common symptoms
Many of the symptoms experienced by individuals with AML result from a shortage of healthy blood cells due to the overcrowding of leukemic cells in the bone marrow. These symptoms may include:
- Fatigue and weakness
- Shortness of breath during normal physical activities
- Lightheadedness, dizziness, or fainting
- Pale complexion
- Frequent infections and fever
- Easy bruising and prolonged bleeding from minor cuts
- Frequent or severe nosebleeds
- Bleeding gums
Other general symptoms of AML may include:
- Loss of appetite and unexplained weight loss
- Discomfort in bones or joints
- Fullness or swelling in the abdomen due to an enlarged spleen or liver
RELATED: How to Identify and Remove Tonsil Stones: A Complete Guide
Rare symptoms
In some cases, AML can cause more unusual symptoms, such as:
- Leukostasis: When white blood cell counts become extremely high, leukemic cells can clog blood vessels, leading to headaches, confusion, seizures, visual disturbances, difficulty breathing, respiratory failure, or coma. This is a medical emergency that requires immediate treatment.
- Myeloid sarcoma: Rarely, a mass of leukemic cells may form outside the bone marrow (extramedullary disease), most commonly in the skin, soft tissues, lymph nodes, or the dense layer of tissue covering the bone (periosteum).
- Leukemia cutis: In fewer than 10% of AML cases, cancer cells may migrate to the skin, causing various skin problems, including spots, bumps, or rashes.
- Central nervous system involvement: Although uncommon, leukemic cells can spread to the brain and spinal cord, potentially causing symptoms such as headaches, weakness, seizures, vomiting, trouble with balance, facial numbness, or blurred vision.
When to see a doctor
While the signs and symptoms of AML can be attributed to other, less serious illnesses, it is crucial to consult a doctor if you experience any of the following:
- Persistent fatigue or weakness
- Recurrent infections or fever
- Unusual bleeding or bruising
- Unexplained weight loss
- Discomfort in bones or joints
- Fullness or swelling in the abdomen
Seeking prompt medical attention can facilitate early diagnosis and treatment, which is essential for improving outcomes in individuals with acute myeloid leukemia.
AML Diagnostic Process
Diagnosing acute myeloid leukemia (AML) involves a series of tests to determine the presence, subtype, and severity of the disease. An accurate diagnosis is crucial for estimating disease progression and selecting the most appropriate treatment approach.
The diagnostic process begins with a thorough medical history and physical examination, focusing on symptoms, risk factors, and any signs of infection, bleeding, or bruising. If AML is suspected, the doctor will order blood tests to evaluate blood cell counts and identify any abnormalities.
Initial tests
- Complete blood count (CBC) with differential: This test measures the number of red blood cells, white blood cells, and platelets in the blood. In AML, there is often a high number of white blood cells, mostly leukemic blasts, and a low number of red blood cells and platelets.
- Peripheral blood smear: A sample of blood is examined under a microscope to assess the appearance and maturity of blood cells. The presence of myeloblasts in the blood is a strong indicator of AML.
- Bone marrow aspiration and biopsy: These procedures involve removing samples of liquid bone marrow and a small piece of bone for examination. The samples are obtained from the hip bone under local anesthesia. The presence of 20% or more myeloblasts in the bone marrow confirms an AML diagnosis.
Confirmatory tests
- Cytochemistry: Cells are exposed to chemical stains that react with specific types of leukemia cells, causing color changes visible under a microscope. This helps distinguish AML cells from other types of leukemia.
- Flow cytometry and immunohistochemistry: These tests use antibodies to identify specific proteins (antigens) on the surface of leukemia cells, aiding in the classification of AML subtypes based on cell maturity and lineage.
- Lumbar puncture (spinal tap): In cases where AML has potentially spread to the central nervous system, a sample of cerebrospinal fluid may be collected for testing.
Cytogenetic and molecular testing
Cytogenetic and molecular tests analyze chromosomes and genes within the leukemia cells to identify specific abnormalities that can help determine prognosis and guide treatment decisions.
- Cytogenetics (karyotyping): This test examines the chromosomes under a microscope to detect any abnormalities, such as translocations, inversions, deletions, or additions.
- Fluorescence in situ hybridization (FISH): FISH uses fluorescent dyes to detect specific chromosome changes that may be too small to be seen with standard cytogenetic testing.
- Polymerase chain reaction (PCR): This highly sensitive test can detect gene and chromosome changes too small to be seen under a microscope, making it useful for identifying minimal residual disease after treatment.
- Other molecular and genetic tests: Additional tests may be performed to identify specific gene mutations, such as FLT3, IDH1, and IDH2, which can influence treatment options and prognosis.
Imaging tests, such as X-rays, CT scans, PET/CT scans, MRI, and ultrasound, are not typically used to diagnose AML but may be employed to assess the extent of the disease or to identify infections or other complications.
The results of these diagnostic tests help hematologist-oncologists determine the specific subtype of AML, assess the disease’s severity, and develop a personalized treatment plan for each patient.
Treatment Approaches for AML
The treatment of acute myeloid leukemia (AML) typically involves a multi-phase approach, which includes induction therapy, consolidation therapy, and maintenance therapy. The goal of treatment is to eliminate leukemia cells, restore normal blood cell production, and prevent relapse.
Induction Therapy
Induction therapy is the first phase of AML treatment, aiming to achieve complete remission by rapidly reducing the number of leukemia cells in the blood and bone marrow. The most common induction regimen for AML includes the chemotherapy drugs (ara-C) and an anthracycline drug, often referred to as the “7+3” protocol.
In some cases, targeted therapy drugs may be added to the induction regimen to improve remission rates:
- For patients with FLT3 gene mutations, midostaurin (Rydapt) or quizartinib (Vanflyta) may be given along with chemotherapy.
- For patients with CD33 protein on their leukemia cells, (Mylotarg) may be added to chemotherapy.
Patients typically require hospitalization during induction therapy due to the intensive nature of the treatment and the potential for severe side effects. Blood transfusions, antibiotics, and growth factors may be necessary to manage complications.
Maintenance Therapy
Maintenance therapy, also called post-consolidation therapy, is given over a longer period to keep the leukemia from returning. Not all patients with AML require maintenance therapy, but it may be an option for those at higher risk of relapse or those unable to complete intensive initial treatment.
Options for maintenance therapy include:
- Oral chemotherapy drug (Onureg)
- Continuation of targeted therapy drugs (without chemotherapy) for patients who received them during initial treatment
Treatment for older, frail patients or those who opt for less intensive therapy may not be divided into distinct phases. Instead, they may receive low-intensity chemotherapy, targeted drugs, or supportive care to manage symptoms and maintain quality of life.
The treatment approach for AML is highly individualized and depends on various patient- and disease-related factors. Close collaboration between the patient and the healthcare team is essential to determine the most appropriate treatment plan while considering the potential benefits and risks.
Managing AML Side Effects
Treatment for acute myeloid leukemia can cause a range of side effects that impact patients’ quality of life. Managing these side effects is an essential part of supportive care for AML patients.
Treatment-related side effects
Common side effects of AML treatment include:
- Myelosuppression: Chemotherapy drugs can suppress the bone marrow, leading to low blood cell counts. This can cause anemia (low red blood cells), neutropenia (low white blood cells), and thrombocytopenia (low platelets).
- Infection: Neutropenia increases the risk of infections, which can be serious and life-threatening. Patients may receive antibiotics, antivirals, or antifungals to prevent or treat infections.
- Bleeding: Thrombocytopenia can cause abnormal bleeding. Patients with low platelet counts may require transfusions to prevent or control bleeding.
- Fatigue: Anemia and the overall impact of treatment can cause significant fatigue. Rest, nutrition, and managing other symptoms can help alleviate fatigue.
- Nausea and vomiting: Chemotherapy drugs can cause nausea and vomiting. Anti-nausea medications and dietary changes can help manage these symptoms.
- Mouth sores: Some chemotherapy drugs can cause painful mouth sores or mucositis. Good oral hygiene and pain management can help alleviate discomfort.
- Hair loss: Many chemotherapy drugs cause temporary hair loss. Patients may choose to wear wigs, hats, or scarves during treatment.
RELATED: Scabies: Comprehensive Guide to Symptoms and Treatments
Supportive care
Supportive care is essential for managing side effects and maintaining quality of life during AML treatment. Key aspects of supportive care include:
- Transfusions: Red blood cell and platelet transfusions can help manage anemia and thrombocytopenia.
- Infection prevention and treatment: Patients may receive prophylactic antibiotics, antivirals, or antifungals to prevent infections. Prompt treatment of infections is crucial.
- Nutrition support: Maintaining adequate nutrition is important for overall health and recovery. Some patients may require supplemental nutrition or feeding tubes.
- Pain management: Pain can be caused by the disease itself or by treatment side effects. Appropriate pain management is essential for maintaining quality of life.
- Emotional support: AML diagnosis and treatment can be emotionally challenging. Counseling, support groups, and other resources can help patients cope with the emotional impact of the disease.
Quality of life considerations
AML and its treatment can have a significant impact on patients’ quality of life. Important considerations include:
- Fatigue and activity levels: Fatigue is a common side effect that can limit patients’ ability to participate in daily activities. Balancing rest and activity is important for maintaining quality of life.
- Emotional well-being: AML can cause significant emotional distress, including anxiety and depression. Addressing emotional well-being through counseling, medication, or other support services is crucial.
- Social support: Support from family, friends, and healthcare providers is essential for coping with the challenges of AML treatment.
- Long-term effects: Some side effects of AML treatment, such as cognitive changes or neuropathy, may persist after treatment ends. Ongoing monitoring and management of these effects is important for long-term quality of life.
Managing side effects and providing comprehensive supportive care is crucial for helping AML patients maintain the best possible quality of life during and after treatment. A multidisciplinary team approach, including oncologists, nurses, social workers, and other healthcare professionals, can help address the complex needs of AML patients and their families.
Conclusion
Acute myeloid leukemia poses significant challenges to patients and healthcare providers alike. The complex nature of this disease, from its varied risk factors to its diverse symptoms and treatment approaches, underscores the need for ongoing research and personalized care strategies. Advances in diagnostic techniques and targeted therapies have opened up new avenues to combat AML, offering hope for improved outcomes and quality of life for those affected.
Managing AML is a team effort, involving not just medical interventions but also comprehensive supportive care. The journey through diagnosis, treatment, and recovery can be grueling, but with the right support and resources, patients can navigate these challenges more effectively. As our understanding of AML continues to grow, so does our ability to develop more effective treatments and provide better care for those living with this challenging disease.