Addison’s disease is a rare endocrine disorder that affects the adrenal glands, causing them to produce insufficient amounts of vital hormones. This condition can have a significant impact on a person’s overall health and quality of life. Despite its rarity, understanding Addison’s disease is crucial for early detection and proper management of the condition.
This article aims to provide a comprehensive look at Addison’s disease, covering its symptoms, diagnosis, and treatment methods. It will explore the various signs that may indicate the presence of this disorder, discuss the diagnostic procedures used to confirm it, and examine the different treatment options available to those affected. By shedding light on this often-overlooked condition, we hope to increase awareness and improve outcomes for individuals living with Addison’s disease.
Understanding Addison’s Disease




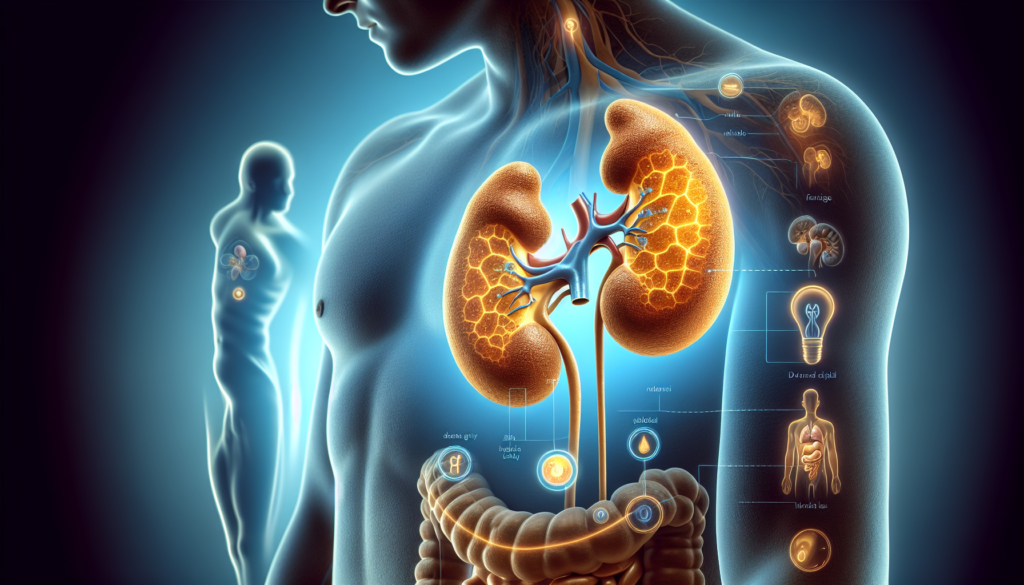
Addison’s disease, also known as primary adrenal insufficiency or hypoadrenalism, is a rare disorder of the adrenal glands. The adrenal glands, located on top of the kidneys, produce two essential hormones: cortisol and aldosterone. In Addison’s disease, the adrenal glands are damaged and do not produce enough of these hormones, leading to a range of symptoms and potential complications.
What is Addison’s Disease?
Addison’s disease affects approximately 9,000 people in the UK, with over 300 new cases diagnosed each year. It can impact individuals of any age, although it is most common between the ages of 30 and 50 and is more prevalent in women than men. The condition is characterized by a gradual onset of symptoms, such as fatigue, muscle weakness, low mood, loss of appetite, and unintentional weight loss. As the disease progresses, additional symptoms may include dizziness, fainting, cramps, and exhaustion, as well as darkened skin patches or darkened lips and gums.
Causes of Addison’s Disease
The most common cause of Addison’s disease is an autoimmune response, responsible for 70% to 90% of cases in the UK. In this scenario, the body’s immune system mistakenly attacks the outer layer of the adrenal gland (the adrenal cortex), disrupting the production of cortisol and aldosterone. The exact reason for this autoimmune response is not clear. Other potential causes include conditions that can damage the adrenal glands, such as tuberculosis (TB), although this is uncommon in the UK.
RELATED: Syphilis: Key Symptoms, Diagnosis Methods, and Treatment
Types of Adrenal Insufficiency
Adrenal insufficiency can be classified into three types: primary, secondary, and tertiary. Primary adrenal insufficiency, often called Addison’s disease, occurs when the adrenal glands are damaged and cannot produce enough cortisol and sometimes aldosterone. Secondary adrenal insufficiency originates in the pituitary gland, which fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenal glands to make cortisol. Tertiary adrenal insufficiency starts in the hypothalamus, which does not make enough corticotropin-releasing hormone (CRH) to signal the pituitary to produce ACTH, ultimately leading to insufficient cortisol production by the adrenal glands.
Recognizing the Symptoms
Addison’s disease has a gradual onset, with symptoms developing over months or even years. The most common symptoms include:
- Extreme fatigue
- Weight loss and loss of appetite
- Areas of darkened skin
- Low blood pressure, even fainting
- Salt craving
- Low blood sugar (hypoglycemia)
- Nausea, diarrhea, or vomiting
- Abdominal pain
- Muscle and joint pain
- Irritability
- Depression
- Body hair loss or sexual issues in some people
As the disease progresses, additional symptoms may include dizziness, fainting, cramps, and exhaustion. Patients with Addison’s disease may also have darkening of their skin, most visible on scars, skin folds, pressure points such as the elbows, knees, knuckles, and toes, lips, and mucous membranes such as the lining of the cheek.
Because the symptoms of Addison’s disease come on slowly over time, they may be overlooked or confused with other illnesses. If a person always feels tired, weak, or is losing weight, they should ask their healthcare provider if they might have adrenal insufficiency. Early treatment can help avoid an adrenal crisis.
Addisonian Crisis
Sometimes, the symptoms of Addison’s disease appear suddenly, leading to a condition called acute adrenal failure or addisonian crisis. This is a life-threatening situation that results in low blood pressure, low blood levels of sugar, and high blood levels of potassium. It requires immediate medical care.
Symptoms of an addisonian crisis may include:
- Severe weakness
- Confusion
- Pain in the lower back or legs
- Severe abdominal pain, vomiting, and diarrhea, leading to dehydration
- Reduced consciousness or delirium
- Low blood pressure
An addisonian crisis frequently occurs in patients with known adrenal insufficiency. The most frequent triggers are infectious causes. Patients with primary adrenal insufficiency are slightly more likely than those with secondary adrenal insufficiency to have a crisis.
Recognizing the symptoms of Addison’s disease early is crucial for prompt diagnosis and treatment. Patients and healthcare providers should be aware of the signs and symptoms, especially in those with a history of autoimmune disorders or chronic steroid use. Regular follow-up with an endocrinologist can help manage the condition and prevent complications like an addisonian crisis.
Diagnosis and Testing
Diagnosing Addison’s disease involves a comprehensive evaluation of the patient’s medical history, symptoms, and laboratory tests. The GP will examine the skin for evidence of hyperpigmentation, particularly in areas such as the creases on the palm, elbow crease, scars, lips, and gums. However, hyperpigmentation does not occur in all cases of Addison’s disease. The patient will also be tested for low blood pressure (hypotension) while lying down and shortly after standing up to check for postural or orthostatic hypotension.
Blood Tests
If Addison’s disease is suspected, blood tests will be carried out to measure the levels of sodium, potassium, and cortisol in the body. A low sodium, high potassium, or low cortisol level may indicate Addison’s disease. The patient may need to see a hospital hormone specialist (endocrinologist) for further blood tests, including:
- A low level of the hormone aldosterone
- A high level of adrenocorticotrophic hormone (ACTH)
- A low level of glucose (sugar used for energy)
- Positive adrenal antibodies (antibodies designed to attack the adrenal gland)
Any of the above could be a sign of Addison’s disease.
RELATED: Effective Treatments for Pancreatitis: What You Need to Know
Imaging Studies
In some cases, the specialist may refer the patient for a scan of the adrenal glands, such as a CT scan or an MRI scan. These imaging tests can help identify any changes in the size or appearance of the adrenal glands that may be causing Addison’s disease.
Additionally, the thyroid gland may also be tested to see if it is working properly. People with Addison’s disease often have an underactive thyroid (hypothyroidism), where the thyroid gland does not produce enough hormones. By testing the levels of certain hormones in the blood, the endocrinologist can determine whether the patient has hypothyroidism.
It is important to note that during an adrenal crisis, there may not be enough time to perform a stimulation test to confirm Addison’s disease. In such cases, blood will be taken and tested for any abnormalities, and treatment may be started with steroid injections and fluids containing salt and glucose while waiting for the results.
Treatment Options
The treatment of Addison’s disease involves replacing the hormones that the adrenal glands are not producing sufficiently. This is typically achieved through hormone replacement therapy and lifestyle modifications. In cases of adrenal crisis, emergency treatment is necessary to prevent life-threatening complications.
Hormone Replacement Therapy
Patients with Addison’s disease require daily medication to replace the lost hormones. The most commonly prescribed medications include:
- Hydrocortisone: This synthetic form of cortisol is usually taken orally two to three times a day. It replaces the cortisol that the adrenal glands are not producing.
- Dehydroepiandrosterone (DHEA): Some patients may benefit from taking DHEA supplements to improve their stamina and libido. However, this medication is not available on the NHS and requires a private prescription.
The dosage of these medications may need to be adjusted during times of physical stress, such as illness, surgery, or injury. Patients should work closely with their healthcare provider to determine the appropriate dosage adjustments.
Lifestyle Modifications
In addition to hormone replacement therapy, patients with Addison’s disease may need to make certain lifestyle changes to manage their condition effectively. These may include:
- Maintaining a balanced diet with adequate salt intake
- Staying hydrated by drinking enough fluids
- Getting regular exercise, but avoiding overexertion
- Managing stress through relaxation techniques or counseling
- Wearing a medical alert bracelet or carrying an emergency card that identifies their condition
Patients should also be aware of the signs and symptoms of an adrenal crisis and have an emergency plan in place.
RELATED: How to Prevent and Treat Pink Eye (Conjunctivitis)
Emergency Treatment
An adrenal crisis is a life-threatening emergency that requires immediate medical attention. Patients experiencing an adrenal crisis may present with the following symptoms:
- Severe weakness and fatigue
- Low blood pressure
- Confusion or loss of consciousness
- Abdominal pain, nausea, and vomiting
Treatment for an adrenal crisis involves:
- Administering an emergency injection of hydrocortisone (100mg) intramuscularly
- Seeking immediate medical attention and calling for an ambulance
- Informing medical professionals about the patient’s steroid-dependent condition and describing the symptoms of adrenal crisis
- Providing emergency medical personnel with the patient’s steroid emergency card or information
In the hospital, treatment will include intravenous fluids to restore hydration and electrolyte balance, as well as continued administration of hydrocortisone. Any underlying causes of the adrenal crisis, such as an infection, will also be addressed.
Patients with Addison’s disease and their families should be educated on the proper use of emergency hydrocortisone injections and the importance of seeking prompt medical attention during an adrenal crisis.
Conclusion
Addison’s disease has a significant impact on the lives of those affected, requiring ongoing management and vigilance. Understanding its symptoms, causes, and treatment options is crucial to improve the quality of life for patients. Early diagnosis and proper hormone replacement therapy, along with lifestyle adjustments, can help individuals with Addison’s disease lead normal, active lives. However, the importance of educating patients and their families about the condition, especially to recognize and respond to an adrenal crisis, cannot be overstated.
Research into Addison’s disease continues to advance, offering hope for better diagnostic tools and treatment methods in the future. While living with this condition presents challenges, with proper care and support, many people with Addison’s disease can effectively manage their symptoms and thrive. Ongoing communication with healthcare providers and staying informed about the latest developments in adrenal insufficiency management are key to ensuring the best possible outcomes for those affected by this rare but serious endocrine disorder.