Moles are a common skin feature that many people have, yet they often raise questions and concerns. These small, pigmented growths can appear anywhere on the body and vary in size, shape, and color. While most moles are harmless, some can be a sign of serious skin conditions, making it crucial to understand their nature and potential implications.
This article delves into the world of moles, covering everything from their causes to available treatment options. It explores the different types of moles, what triggers their formation, and how to spot potential warning signs. Readers will also learn about diagnostic methods used by healthcare professionals and the various ways to manage or remove moles when necessary. By the end, you’ll have a comprehensive understanding of these intriguing skin marks and how to care for them properly.
What Are Moles?



Moles, also known as nevi, are common skin growths that develop when pigment-producing cells called melanocytes grow in clusters. These growths can appear anywhere on the skin or mucous membranes, either alone or in groups. Most moles are harmless and typically develop during childhood and adolescence, with the average person having between 10 to 40 moles by adulthood.
The life cycle of a mole is approximately 50 years. Over time, moles may change slowly, becoming raised and lighter in color. Some moles may develop hairs, while others remain unchanged or gradually fade away.
Types of Moles
There are several types of moles, including:
- Common Nevi: These are normal moles that are small, round, and have a distinct edge. They can be pink, tan, or brown in color.
- Congenital Nevi: These moles are present at birth and occur in about one in 100 people. Congenital nevi that are larger than 20 cm in diameter have a higher risk of developing into melanoma.
- Dysplastic Nevi: Also known as atypical moles, these are larger than a pencil eraser and have irregular shapes and colors. They tend to be hereditary and may indicate a higher risk of developing melanoma.
- Spitz Nevi: These moles are often pink, raised bumps that can also be red, blue, or black. They are most common in children and adolescents and may resemble melanoma, requiring surgical removal for proper diagnosis.
- Blue Nevi: These moles are blue-gray to blue-black in color and can be found on the head, neck, and arms. They are usually benign but may rarely become cancerous.
RELATED: What is an Arcuate Uterus? Symptoms and Treatments
Common Characteristics
Moles can vary in color, texture, and shape. They may be:
- Brown, tan, black, blue, red, or pink in color
- Smooth, wrinkled, flat, or raised in texture
- Round or oval in shape
- Less than 6 mm in diameter (about the size of a pencil eraser)
Some moles may have hair growing from them. It is important to monitor moles for any changes in color, size, shape, or texture, as these changes may indicate the development of skin cancer, particularly melanoma. If a mole becomes itchy, painful, or bleeds, it should be evaluated by a healthcare professional.
Causes of Moles
Moles, also known as nevi, are common skin growths that develop when pigment-producing cells called melanocytes grow in clusters. These growths can appear anywhere on the skin or mucous membranes, either alone or in groups. Most moles are harmless and typically develop during childhood and adolescence, with the average person having between 10 to 40 moles by adulthood.
The formation of moles is influenced by several factors, including:
Melanocyte Clusters
Melanocytes are the cells responsible for producing melanin, the pigment that gives skin its color. When these cells grow in clusters instead of being evenly distributed throughout the skin, they form moles. The reason why melanocytes sometimes grow in clusters is not fully understood, but it is thought to be related to genetic and environmental factors.
Genetic Factors
Genetics play a significant role in the development of moles. If a person has a family history of moles, they are more likely to develop them as well. Some specific gene variations, such as those in the FGFR3, PIK3CA, HRAS, and BRAF genes, have been linked to the formation of benign moles. The most-studied of these is the BRAF gene, which leads to the production of an altered protein that causes melanocytes to aggregate into moles.
RELATED: Arachnophobia (Fear of Spiders) Explained: Causes, Symptoms, and Solution
Sun Exposure
Exposure to ultraviolet (UV) radiation from the sun is another important factor in the development of moles. UV radiation can cause damage to the DNA in skin cells, leading to mutations that may trigger the growth of moles. People who spend a lot of time in the sun, especially during childhood and adolescence, tend to have more moles than those who have less sun exposure.
Studies have shown that sun exposure can play a role in the development of moles, and some trials have demonstrated that staying safe in the sun can reduce the number of new moles developing on children’s skin. However, it is important to note that not all moles are caused by sun exposure, and some may develop on areas of the body that are not typically exposed to the sun.
In rare cases, the combination of certain gene variations, such as those in the BRAF and CDKN2A genes, along with excessive sun exposure, can increase the risk of moles becoming cancerous (malignant). This highlights the importance of protecting the skin from UV radiation and monitoring moles for any changes in color, size, shape, or texture.
Signs and Symptoms
Most moles are harmless and do not cause any symptoms. A normal mole typically has the following characteristics:
- Round or oval shape with a distinct edge
- Smooth surface
- Even color (tan, brown, or flesh-colored)
- Diameter less than 6mm (about the size of a pencil eraser)
However, it is important to be aware of the warning signs that may indicate a mole could be cancerous. The ABCDE rule is a helpful guide for identifying potentially problematic moles:
- Asymmetry: One half of the mole does not match the other half
- Border: The edges are ragged, notched, or blurred
- Color: The color is uneven, with shades of black, brown, tan, white, gray, red, pink, or blue
- Diameter: The mole is larger than 6mm (about 1/4 inch) wide
- Evolving: The mole has changed in size, shape, or color over the past few weeks or months
In addition to the ABCDE rule, other warning signs to look out for include:
- A mole that looks different from other moles on your body (the “ugly duckling” sign)
- Itching, tenderness, or pain in a mole
- A mole that bleeds or oozes
- A mole with a dry, scaly, or crusted surface
It is normal for moles to change slowly over time. As people age, moles may:
- Become raised
- Develop hairs
- Lighten in color
- Fade away completely
However, rapid or significant changes in a mole’s appearance should be evaluated by a healthcare professional. If a mole starts to look different from other moles or displays any of the ABCDE warning signs, it is important to have it checked by a doctor.
Regular self-examination of the skin can help detect any new or changing moles early on. It is recommended to perform a thorough skin self-exam once a month, using a full-length mirror and a hand mirror to check hard-to-see areas. If you notice any concerning changes or new moles, schedule an appointment with a dermatologist for a professional evaluation.
Diagnosis and Evaluation
Diagnosing moles involves a combination of self-examination, professional skin checks, and biopsy procedures. It’s important to be proactive in monitoring your skin for any suspicious changes or growths.
Self-Examination
Regularly examining your own skin is a crucial step in detecting potential issues early on. The American Academy of Dermatology recommends performing a thorough skin self-exam once a month. To conduct a self-exam:
- Use a well-lit room, a full-length mirror, and a hand-held mirror.
- Check your face, ears, neck, chest, and belly, lifting breasts to examine the skin underneath.
- Inspect your underarms, arms, hands, fingers, and under your fingernails.
- Examine the front and back of your thighs, shins, feet, toes, and toenails.
- Use a hand mirror to check your buttocks, genital area, lower and upper back, and the back of your neck and ears.
- Part your hair to examine your scalp thoroughly.
Look for any new, expanding, or changing growths, spots, or bumps on the skin. Pay attention to sores that bleed or don’t heal, rough or scaly patches, wart-like growths, and moles that are asymmetrical, have irregular borders, vary in color, or are larger than a pencil eraser.
RELATED:
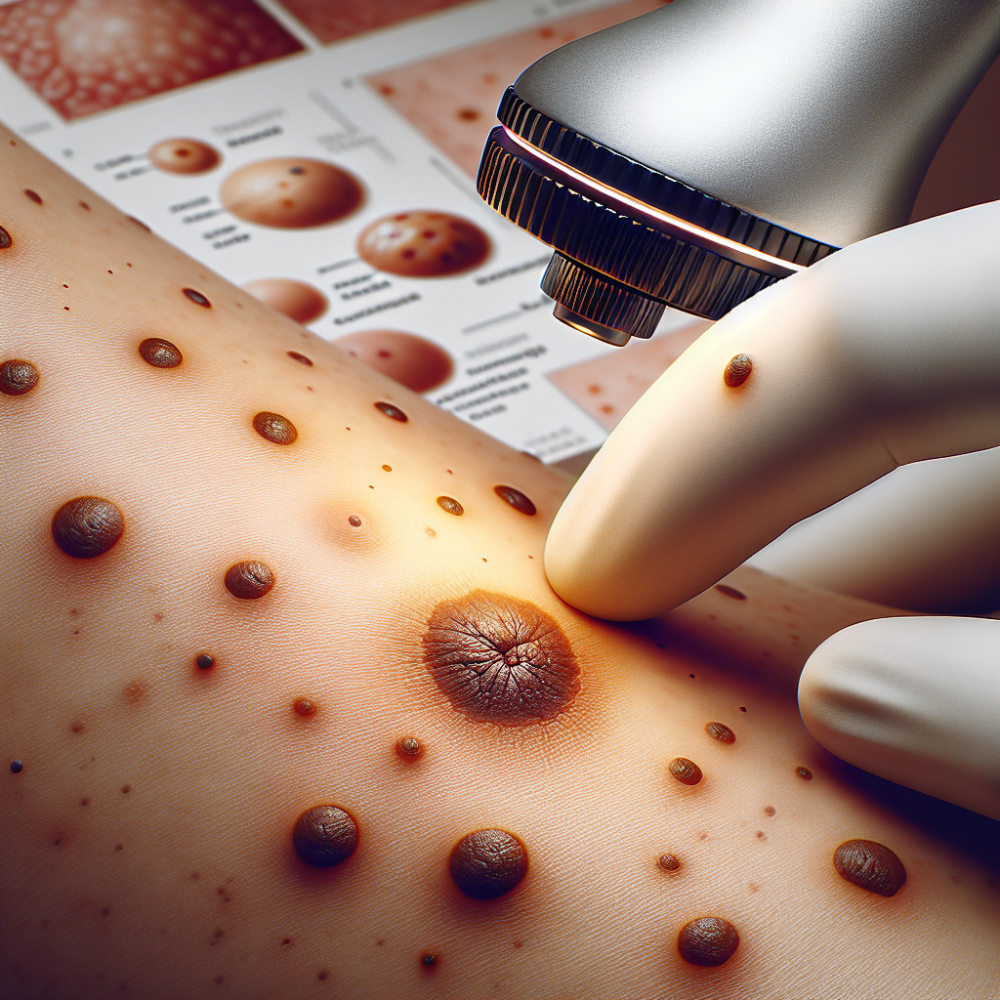
Professional Skin Checks
In addition to self-exams, it’s essential to have regular professional skin checks performed by a dermatologist or healthcare provider. The frequency of these checks may vary depending on your individual risk factors, such as a history of skin cancer or a large number of moles.
During a professional skin check, the doctor will:
- Ask about your medical history, sun exposure, and any concerning symptoms
- Thoroughly examine your skin from head to toe, including hard-to-see areas
- Use a dermatoscope, a specialized magnifying tool, to closely evaluate suspicious moles or spots
- Measure and document the size, shape, color, and texture of any concerning areas
- Refer you to a dermatologist for further evaluation if necessary
Biopsy Procedures
If a mole or skin lesion appears suspicious during a self-exam or professional skin check, a biopsy may be recommended to determine whether it is cancerous. There are several types of skin biopsies:
- Shave biopsy: A thin layer of the mole is shaved off using a razor-like tool. This method is often used for small, superficial lesions.
- Punch biopsy: A circular tool is used to remove a small, cylindrical sample of the mole, including deeper layers of skin. This technique is useful for diagnosing potential melanomas.
- Excisional biopsy: The entire mole or lesion is surgically removed, along with a margin of surrounding healthy skin. This approach is preferred for larger or more concerning moles.
The biopsied tissue is then sent to a laboratory for microscopic examination by a pathologist or dermatopathologist. These specialists are trained to identify the presence of cancer cells and determine the type and stage of skin cancer, if present.
By combining regular self-exams, professional skin checks, and prompt biopsy of suspicious moles, you can significantly improve the chances of early detection and successful treatment of skin cancer.
Treatment Options
When it comes to treating moles, there are several options available depending on the type of mole and its potential for developing into skin cancer. Healthcare providers will assess the mole and recommend the most appropriate treatment plan.
Monitoring
For non-cancerous moles that do not display any suspicious characteristics, monitoring may be the preferred approach. In this case, the healthcare provider will closely observe the mole over time, typically every three months, to check for any changes in size, shape, or color. Photographs of the mole may be taken to help track its appearance and detect any concerning developments. If the mole remains stable and harmless, no further intervention may be necessary.
Surgical Removal
If a mole is suspected to be cancerous or presents with worrisome features, surgical removal is often the recommended treatment. There are two main methods for surgically removing moles:
- Excision: In this procedure, the mole is cut out using a scalpel, along with a small margin of surrounding healthy skin. The area is numbed with a local anesthetic before the mole is removed. Stitches may be required to close the wound, especially if the mole was deep within the skin.
- Shave Removal: This method involves using a razor-like tool to shave off the mole until it is level with the surrounding skin. A local anesthetic is administered to ensure patient comfort during the procedure. Stitches are generally not necessary after a shave removal, although a small pink patch may be visible where the mole was removed.
The choice between excision and shave removal depends on factors such as the location, size, and type of mole, as well as the healthcare provider’s assessment of the mole’s potential for malignancy.
RELATED: Understanding Arachnoiditis: Symptoms, Causes, and Treatments
Alternative Removal Methods
In some cases, non-surgical methods may be used to remove moles, particularly if they are small, flat, and non-cancerous. These alternative removal methods include:
- Laser Mole Removal: This technique uses targeted bursts of light radiation to destroy the mole tissue. Multiple treatments may be required to completely remove the mole. Laser removal is often preferred for moles in hard-to-reach or sensitive areas, such as the face or ears.
- Freezing (Cryotherapy): Liquid nitrogen is applied to the mole to freeze and destroy the tissue. This method is generally used for small, superficial moles that are limited to the skin’s surface. A blister may form where the mole was located after the procedure.
It is essential to note that while these alternative removal methods can be effective for certain types of moles, they may not provide a tissue sample for biopsy, which is crucial in determining whether a mole is cancerous. Therefore, it is always best to consult with a healthcare professional to determine the most appropriate treatment approach for your specific case.
Conclusion
Understanding moles and their potential implications has a significant impact on our overall skin health. From their various types and causes to the warning signs and treatment options, this comprehensive overview equips readers with the knowledge to monitor their skin effectively. Regular self-exams, coupled with professional skin checks, play a crucial role in early detection and successful management of any concerning moles.
To wrap up, being proactive about mole care is key to maintaining healthy skin. By staying informed and vigilant, individuals can work closely with healthcare providers to address any issues promptly. This approach not only helps to manage existing moles but also contributes to the prevention and early detection of potential skin cancers, ultimately promoting long-term skin health and well-being.