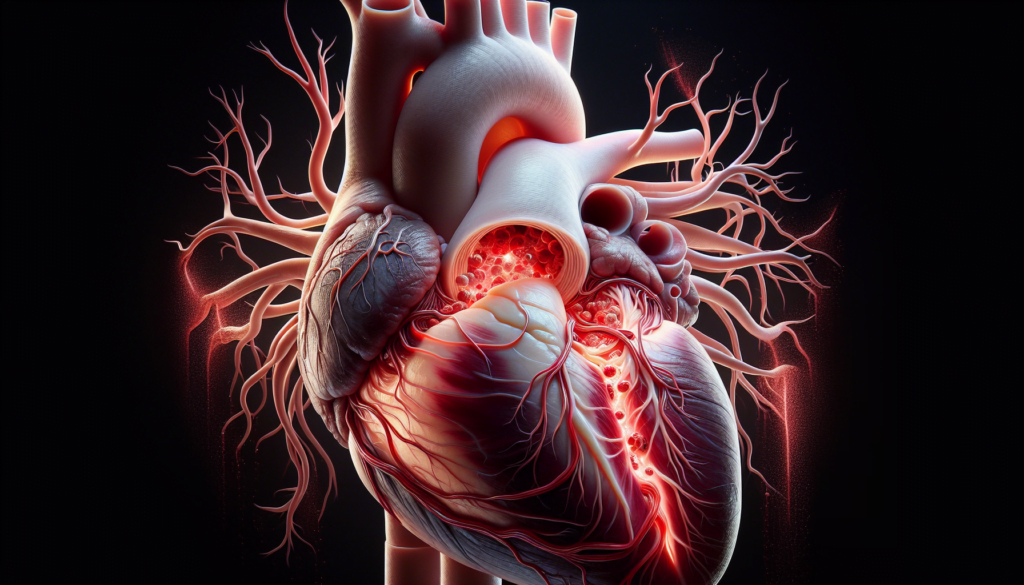
Aortic dissection is a life-threatening condition that occurs when the inner layer of the aorta, the body’s main artery, tears. This tear allows blood to flow between the layers of the aortic wall, causing the layers to separate. It’s a medical emergency that requires immediate attention and treatment. Aortic dissection can lead to severe complications, including reduced blood flow to vital organs, aortic rupture, and even death if not promptly addressed.
This article aims to provide a comprehensive look at aortic dissection. It will explore the underlying causes of this condition, discuss the telltale symptoms that patients and healthcare providers should watch for, and explain the diagnostic procedures used to confirm an aortic dissection. Additionally, it will delve into the various treatment options available, ranging from medication to surgery, and examine the long-term outlook for those who have experienced this serious cardiovascular event.
Understanding Aortic Dissection
Aortic dissection is a life-threatening condition that occurs when a tear develops in the inner layer of the aorta, allowing blood to flow between the layers of the aortic wall. This separation of the layers can lead to the formation of a false lumen, which can extend along the length of the aorta and potentially rupture, causing severe complications or death.
Definition and Types
There are two main types of aortic dissection, classified according to the Stanford system:
- Type A: Involves the ascending aorta, regardless of the site of the primary intimal tear. This type is more common and often requires immediate surgical intervention.
- Type B: Originates distal to the left subclavian artery and involves only the descending aorta. Treatment may include medication or surgery, depending on the severity and complications.
RELATED: Understanding Argyria: Causes, Symptoms, and Treatments
Anatomy of the Aorta
The aorta is the largest artery in the body, originating from the left ventricle of the heart. It is divided into four sections:
- Ascending aorta
- Aortic arch
- Descending thoracic aorta
- Abdominal aorta
Aortic dissections most commonly occur in the ascending aorta and descending thoracic aorta, where the blood pressure is highest.
Pathophysiology of Aortic Dissection
The development of an aortic dissection involves a weakening of the aortic wall, often due to a combination of factors such as hypertension, connective tissue disorders, and age-related degeneration. When a tear occurs in the intimal layer, blood surges through the tear, causing the inner and middle layers to separate.
As the dissection progresses, it can lead to:
- Reduced blood flow to vital organs
- Aortic valve damage
- Cardiac tamponade
- Aortic rupture
Understanding the anatomy, types, and pathophysiology of aortic dissection is crucial for prompt diagnosis and appropriate treatment, which can significantly impact patient outcomes.
Recognizing the Symptoms
Aortic dissection has a sudden onset and can occur at any time, even while resting or sleeping. The most common symptom is a sudden, severe, sharp pain in the chest or upper back, often described as a tearing, stabbing, or ripping sensation. This pain may spread to the neck or down the back.
Common Signs and Symptoms
In addition to the sudden, severe pain, other signs and symptoms of aortic dissection include:
- Shortness of breath
- Fainting or dizziness
- Low blood pressure, especially when there is a 20 mmHg difference between arms
- Diastolic heart murmur or muffled heart sounds
- Rapid, weak pulse
- Heavy sweating
- Confusion
- Loss of vision
- Stroke symptoms, such as weakness or paralysis on one side of the body and difficulty speaking
RELATED: What is an Arcuate Uterus? Symptoms and Treatments
Differences in Type A and Type B Symptoms
The location of the dissection can influence the symptoms experienced. Type A dissections, which involve the ascending aorta, are more likely to cause symptoms related to the heart, such as chest pain, shortness of breath, and fainting. Type B dissections, which occur in the descending aorta, may cause more back pain and symptoms related to reduced blood flow to organs, such as abdominal pain or leg pain.
When to Seek Medical Attention
Aortic dissection is a life-threatening condition that requires immediate medical attention. If you experience any of the above symptoms, especially sudden, severe chest or back pain, call 911 or seek emergency care immediately. Early diagnosis and treatment can significantly improve the chances of survival.
Diagnosing Aortic Dissection
Diagnosing aortic dissection can be challenging as its symptoms often mimic other conditions like acute myocardial infarction or pulmonary embolism. A high index of suspicion, thorough physical examination, imaging studies, and laboratory tests are crucial for an accurate diagnosis.
Physical Examination
Physical findings that may suggest aortic dissection include:
- Hypertension or hypotension
- Blood pressure differential between arms (>20 mmHg)
- Signs of aortic regurgitation (bounding pulses, wide pulse pressure, diastolic murmurs)
- Cardiac tamponade signs (muffled heart sounds, hypotension, pulsus paradoxus, jugular venous distention, Kussmaul sign)
- Neurological deficits (syncope, altered mental status)
- Peripheral paresthesias
- Horner syndrome
- New diastolic murmur
- Asymmetrical pulses (carotid, brachial, femoral)
- Progression or development of bruits
Imaging Techniques
Imaging studies are essential for confirming the diagnosis of aortic dissection. The preferred examinations include:
- Contrast-enhanced spiral computed tomography (CT): Widely available, high sensitivity and specificity (94-100% and 95-100%, respectively)
- Transesophageal echocardiography (TEE): Useful in emergency settings, reveals aortic valve and coronary artery ostia status
- Magnetic resonance imaging (MRI): Most sensitive method, specificity similar to CT, suitable for hemodynamically stable patients
CT and MR angiography have largely replaced conventional diagnostic angiography for assessing aortic dissection.
Laboratory Tests
Laboratory findings that may be present in aortic dissection include:
- Leukocytosis (stress state)
- Decreased hemoglobin and hematocrit (leaking or rupture of the dissection)
- Elevated blood urea nitrogen and creatinine levels (renal artery involvement or prerenal azotemia)
- Elevated myocardial muscle creatine kinase isoenzyme, myoglobin, and troponin I and T levels (myocardial ischemia from coronary artery involvement)
- Lactate dehydrogenase elevation (hemolysis in the false lumen)
- Smooth muscle myosin heavy-chain assay (increased levels in the first 24 hours, 90% sensitive and 97% specific)
- Fibrin degradation product (FDP) elevation (suggests possible aortic dissection with a patent false lumen or complete thrombosis of the false lumen, depending on the level)
A combination of clinical suspicion, physical examination findings, imaging studies, and laboratory tests is necessary for the prompt diagnosis of aortic dissection, which is crucial for initiating appropriate treatment and improving patient outcomes.
Treatment Options and Prognosis
The management of aortic dissection depends on the type and extent of the dissection. Treatment aims to prevent aortic rupture, restore blood flow to vital organs, and minimize complications. The two main treatment approaches are medical management and surgical interventions.
Medical Management
Medical therapy is the initial treatment for uncomplicated type B aortic dissections. The goal is to reduce blood pressure and heart rate, thereby decreasing the stress on the aortic wall. Intravenous beta-blockers, such as esmolol, are commonly used to achieve a target heart rate of 60 beats per minute. Other medications, including calcium channel blockers and vasodilators, may be added to control blood pressure.
Patients are closely monitored in the intensive care unit, with strict blood pressure control and pain management. Long-term antihypertensive therapy is essential to prevent disease progression and complications.
RELATED: Arachnophobia (Fear of Spiders) Explained: Causes, Symptoms, and Solution
Surgical Interventions
Surgical intervention is the primary treatment for type A aortic dissections and complicated type B dissections. The goal is to prevent aortic rupture, restore blood flow, and repair the damaged aorta.
- Open Surgical Repair: This involves replacing the dissected portion of the aorta with a synthetic graft. For type A dissections, the ascending aorta and aortic arch may be replaced, with reimplantation of the coronary arteries. Aortic valve repair or replacement may be necessary if the valve is damaged.
- Endovascular Repair: This minimally invasive technique involves placing a stent-graft within the aorta to seal the entry tear and redirect blood flow into the true lumen. It is an option for complicated type B dissections and patients who are not candidates for open surgery.
Long-term Outlook and Follow-up Care
The prognosis of aortic dissection depends on the type, extent, and promptness of treatment. Type A dissections have a higher mortality rate than type B dissections. Patients who survive the acute phase require lifelong surveillance and management of risk factors.
Regular follow-up with imaging studies, such as CT or MRI, is crucial to monitor the aorta for aneurysmal dilatation or late complications. Patients should maintain strict blood pressure control, quit smoking, and adopt a heart-healthy lifestyle to improve long-term outcomes.
Conclusion
Aortic dissection is a serious and potentially life-threatening condition that requires prompt diagnosis and treatment. The article has explored the various aspects of this condition, including its causes, symptoms, diagnostic methods, and treatment options. Understanding the different types of aortic dissection and their specific characteristics is crucial to provide appropriate care and improve patient outcomes.
To wrap up, early recognition of symptoms and quick medical intervention are key to managing aortic dissection effectively. The combination of advanced imaging techniques, medical management, and surgical interventions has a significant impact on patient survival rates. Long-term follow-up care and lifestyle modifications are essential to prevent complications and ensure the best possible quality of life for those who have experienced this critical cardiovascular event.