Atherosclerosis of the aorta is a condition marked by the buildup of plaque within the walls of the aorta, the body’s main artery. This gradual process can lead to significant cardiovascular complications if left unchecked, underscoring the importance of understanding both the disease and its potential impact on health. Given its pivotal role in circulating blood from the heart to the rest of the body, aortic atherosclerosis represents a critical area of concern within cardiovascular health. Addressing this condition not only involves managing symptoms but also mitigating risks of severe outcomes, rendering the topic essential for both individuals at risk and healthcare professionals.
This article delves into the intricacies of atherosclerosis of the aorta, covering its causes, risk factors, and the mechanisms behind its development. It will further outline the signs that may indicate the presence of this condition, alongside the latest diagnostic methods for identifying atherosclerosis of the aorta. Treatment options will be thoroughly explored, from lifestyle modifications and medications to more invasive procedures, providing a comprehensive overview of how to treat atherosclerosis of the aorta effectively. Additionally, preventative strategies and the potential complications arising from untreated atherosclerotic disease of the abdominal aorta will be discussed, offering a holistic view of managing this widespread yet often preventable disease.
Understanding Atherosclerosis of the Aorta
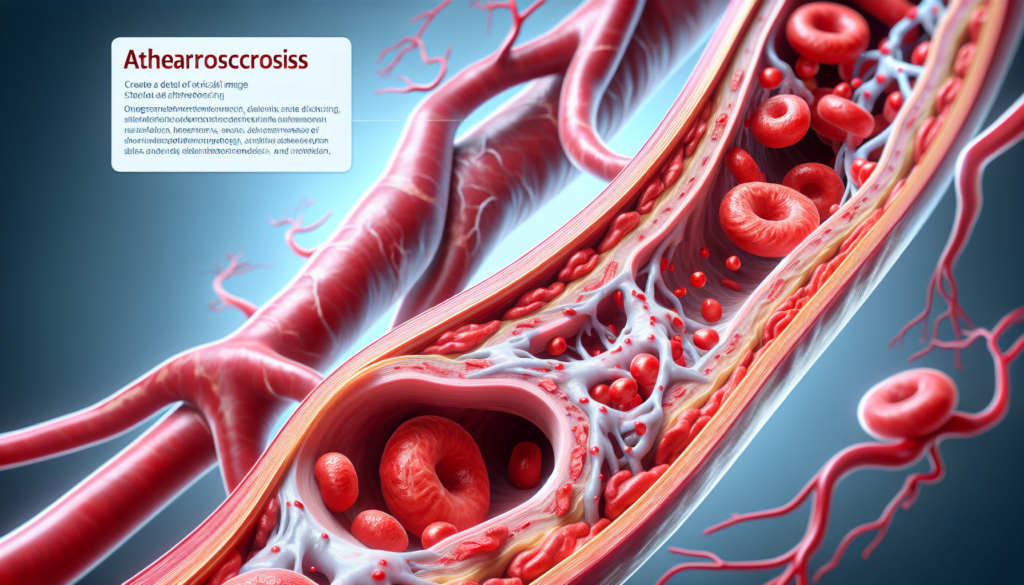
Atherosclerosis of the aorta, often referred to as aortic atherosclerosis, is a progressive condition characterized by the buildup of plaque within the aorta, the largest artery in the human body. This condition is a specific type of arteriosclerosis, which involves the stiffening and hardening of artery walls. However, atherosclerosis is distinguished by its cause— the accumulation of fats, cholesterol, and other substances in and on the artery walls, forming a substance known as plaque.
Definition and Overview
Atherosclerosis begins with damage to the endothelial cells that line the artery walls, which can lead to inflammation and further complications. Over time, these damaged cells accumulate deposits of cholesterol, fats, and other inflammatory cells, forming plaque. This plaque buildup can start as early as childhood and generally progresses with age. The aorta, extending more than one foot long from the heart to the pelvis, is particularly susceptible to severe plaque accumulation, especially in the abdominal section. This buildup can significantly hinder the flow of oxygen-rich blood to various organs and tissues, increasing the risk of ischemia.
Differences Between Atherosclerosis and Arteriosclerosis
While both atherosclerosis and arteriosclerosis involve changes to the arterial walls, they are not synonymous. Arteriosclerosis refers to the general hardening and loss of elasticity in the arteries, often due to aging and the breakdown of elastin fibers in the arterial walls. This condition can lead to increased blood pressure and other cardiovascular issues. On the other hand, atherosclerosis specifically refers to the buildup of plaque within the arteries, which can narrow these vessels and restrict blood flow. The plaque can also rupture, causing blood clots that may lead to severe cardiovascular events.
Atherosclerosis of the aorta is particularly dangerous because it affects the main artery that distributes blood from the heart to the rest of the body. Plaque in the aorta can lead to the formation of emboli—obstructions such as thromboembolism (blood clots) or atheroembolism (cholesterol crystals) that travel through the bloodstream and can block blood flow to critical organs. This condition not only disrupts the systemic distribution of blood but also raises the risk of acute cardiovascular events, highlighting the importance of early diagnosis and effective management.
Causes and Risk Factors
Damage to Arterial Walls
Atherosclerosis of the aorta begins with damage to the endothelial cells lining the artery walls. This damage can be triggered by various factors, including high blood pressure, high levels of cholesterol and triglycerides, and smoking. These conditions disrupt the integrity of the arterial wall, facilitating the accumulation of inflammatory cells and the subsequent formation of plaque. This process not only thickens the walls but also reduces the elasticity of the arteries, impairing blood flow and oxygen supply to vital organs.
Common Risk Factors
The risk factors for atherosclerosis are often interconnected, with lifestyle choices playing a significant role. Key risk factors include:
- Smoking: Tobacco use significantly raises the risk of vascular inflammation and plaque buildup.
- Unhealthy Diet: High intake of saturated fats increases cholesterol levels, contributing to plaque formation.
- Physical Inactivity: Lack of exercise contributes to obesity and poor cardiovascular health, which can accelerate atherosclerosis.
- Diabetes and Insulin Resistance: These conditions lead to higher blood sugar levels, which can damage blood vessels.
- High Blood Pressure: Consistently elevated blood pressure can cause direct harm to the arterial walls.
- Obesity: Excess body weight exacerbates other risk factors like high blood pressure and diabetes.
- Inflammatory Diseases: Conditions such as lupus or rheumatoid arthritis can cause chronic inflammation, affecting the arteries.
Genetic and Lifestyle Influences
Genetics also play a crucial role in the development of atherosclerosis. A family history of the condition can increase an individual’s risk, particularly if relatives have had early onset of cardiovascular diseases. Genetic factors can influence levels of lipoproteins and the body’s inflammatory response, which are critical in the development of atherosclerosis. Lifestyle choices, such as diet and exercise, interact with these genetic predispositions, often determining the severity and progression of the disease. Conditions like familial hypercholesterolemia, a genetic disorder characterized by high cholesterol levels, significantly heighten the risk of developing atherosclerotic plaques from a young age.
Understanding these causes and risk factors is essential for both prevention and management of atherosclerosis, highlighting the importance of regular health screenings and lifestyle modifications.
Symptoms and Diagnosis
Identifying Common Symptoms
Atherosclerosis of the aorta often progresses silently, with symptoms manifesting only when the condition becomes severe. Typically, symptoms occur when an artery is significantly narrowed or clogged, reducing blood flow to vital organs and tissues. This can lead to a variety of symptoms depending on the affected arteries:
- Heart Arteries: If atherosclerosis affects the heart arteries, individuals may experience chest pain or pressure, known as angina.
- Brain Arteries: Atherosclerosis in arteries leading to the brain can cause sudden numbness or weakness in arms or legs, difficulty speaking or slurred speech, temporary loss of vision in one eye, or drooping muscles in the face, signaling a transient ischemic attack (TIA), which, if untreated, can progress to a stroke.
- Peripheral Arteries: In the arms and legs, symptoms may include leg pain when walking (claudication) or decreased blood pressure in an affected limb.
- Renal Arteries: Affecting the kidneys, it may lead to high blood pressure or kidney failure.
Additional severe symptoms include sudden, intense pain and the formation of emboli, which can cause medical emergencies such as heart attacks or strokes. Symptoms of a heart attack include chest pain, dizziness, nausea, and a sudden, severe headache among others. Acute limb ischemia might present with symptoms such as cool or pale skin, numbness, and a weak pulse.
Diagnostic Approaches and Tests
Early detection of atherosclerosis is crucial for effective management and prevention of severe complications. Healthcare providers utilize a range of diagnostic tests to identify and assess the extent of atherosclerosis:
- Physical Examination and History: Initial evaluation includes a detailed review of medical and family history, physical examination, and checking for signs like a bruit—a whooshing sound heard over an artery suggesting turbulent blood flow.
- Blood Tests: These tests check levels of cholesterol, triglycerides, blood sugar, and proteins that indicate inflammation like C-reactive protein.
- Imaging Tests: Various imaging modalities are employed to visualize the arteries and check for plaque buildup.
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI): These provide detailed images of the arteries.
- Transesophageal Echocardiogram: Offers a close look at the heart and aorta.
- Angiography: Involves the use of a special dye to visualize blood flow through the arteries.
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart, indicating any abnormal rhythms or heart muscle stress.
- Stress Tests: These tests assess heart function under stress, either through exercise or medication that simulates exercise, to identify potential heart issues not evident at rest.
- Ankle-Brachial Index (ABI): This test compares blood pressures in the ankle and arm to detect peripheral artery disease, a common complication of atherosclerosis.
Through these diagnostic tools, healthcare providers can not only confirm the presence of atherosclerosis but also determine the severity and specific locations affected, guiding appropriate treatment strategies.
Treatment Options
Lifestyle Changes
Managing atherosclerosis of the aorta often begins with lifestyle modifications aimed at mitigating the overall risk factors associated with the disease. Key lifestyle changes recommended include:
- Smoking Cessation: Individuals are advised to stop smoking as tobacco use significantly increases the risk of vascular diseases including atherosclerosis.
- Dietary Adjustments: Adopting a heart-healthy diet is crucial. This includes consuming a diet rich in fruits, vegetables, and whole grains while limiting intake of saturated fats and cholesterol. Such dietary practices help reduce the buildup of cholesterol in the arteries.
- Regular Physical Activity: Engaging in regular exercise, such as 30 to 45 minutes of aerobic activity 4 to 5 days a week, can improve cardiovascular health and aid in weight management.
- Stress Management: Finding effective ways to manage stress, such as through yoga, meditation, or social activities, can help reduce the physiological impacts of stress on the cardiovascular system.
- Regular Health Screenings: Especially for those over the age of 65 or those with a history of heart conditions, regular checkups with healthcare providers are essential for monitoring heart health and managing any changes in condition.
Medications
A variety of medications are utilized to slow the progression of atherosclerosis and manage its symptoms:
- Cholesterol-lowering Medications: Statins are commonly prescribed to lower cholesterol levels and reduce the risk of plaque buildup. Other types include niacin, fibrates, and bile acid sequestrants.
- Blood Pressure Medications: While these do not reverse atherosclerosis, they are crucial in managing blood pressure levels and reducing the risk of heart attacks.
- Anti-platelet Drugs: Medications like aspirin are used to thin the blood and prevent clot formation, which is vital in preventing heart attacks and strokes. However, these should only be used under a doctor’s supervision due to potential side effects.
- Diabetes Medications: For individuals with diabetes, specific medications are prescribed to control blood sugar levels, which is important in managing the risk factors associated with atherosclerosis.
Surgical Interventions
In cases where atherosclerosis is advanced, surgical interventions may be necessary:
- Angioplasty and Stent Placement: This procedure involves inserting a catheter to widen the blocked artery and placing a stent to keep the artery open.
- Endarterectomy: In this surgical procedure, plaque is physically removed from the walls of the artery to improve blood flow.
- Coronary Artery Bypass Grafting (CABG): This involves using vessels from other parts of the body to bypass blocked coronary arteries and improve blood flow to the heart.
- Fibrinolytic Therapy: Used to dissolve clots that are blocking blood flow, this treatment is critical in acute cases where immediate restoration of blood flow is necessary.
These interventions are complemented by continuous monitoring and follow-up care to ensure the long-term management of atherosclerosis and prevention of future cardiovascular events. Each treatment strategy is tailored to the individual’s specific health needs, taking into account the severity of the disease and any other underlying health conditions.
Preventing Atherosclerosis
Preventing atherosclerosis involves a multifaceted approach that includes dietary recommendations, physical activity, smoking cessation, and regular health screenings. Each of these components plays a crucial role in reducing the risk of developing atherosclerosis and its associated complications.
Dietary Recommendations
A heart-healthy diet is essential for preventing the progression of atherosclerosis. The American Heart Association (AHA) and other health organizations recommend a diet rich in vegetables, fruits, legumes, nuts, whole grains, and fish to decrease atherosclerosis of the aorta and coronary heart disease (CHD) risk factors. Key dietary changes include:
- Reducing Intake of Saturated and Trans Fats: Replace these with monounsaturated (MUFA) and polyunsaturated fatty acids (PUFA), which can lower the risk of cardiovascular disease.
- Increasing Fiber Intake: Foods high in viscous fiber, such as oats and legumes, can help reduce LDL cholesterol levels.
- Limiting Sodium and Cholesterol: Aim to consume less than 200 mg of cholesterol per day and reduce sodium intake to improve blood pressure.
- Incorporating Omega-3 Fatty Acids: These are found in oily fish and flaxseeds and have anti-inflammatory properties that reduce the risk of heart disease.
- Avoiding Processed Meats and Refined Sugars: These contribute to poor cardiovascular health and should be minimized in the diet.
Physical Activity and Smoking Cessation
Regular physical activity is strongly linked to reduced risks of CHD and atherosclerosis. The AHA recommends at least 30 minutes of moderate-intensity exercise most days of the week. Benefits of physical activity include:
- Improved lipid and lipoprotein metabolism, resulting in higher HDL cholesterol and lower triglycerides.
- Enhanced endothelial function, which is crucial for maintaining the health of the vascular system.
- Reduction in inflammation and improvement in heart muscle function.
Smoking cessation is critical, as tobacco use is a major risk factor for atherosclerosis. Quitting smoking can significantly lower cardiovascular risks, although heavy smokers may still face residual risks. Comprehensive anti-smoking campaigns and support systems at a population level are necessary to combat tobacco use effectively.
Regular Health Screenings
Regular screenings play a pivotal role in early detection and management of atherosclerosis risk factors. These screenings can motivate individuals to adopt healthier lifestyles and adhere to necessary medication regimens. Important screening tests include:
- Blood Pressure Checks: Regular monitoring can detect hypertension early, allowing for timely intervention.
- Cholesterol Levels: Checking cholesterol helps manage and reduce the risk of plaque buildup in the arteries.
- Vascular Screenings: These non-invasive tests, such as carotid artery screening and lower extremity arterial screening, assess blood flow and check for blockages or abnormalities in the arteries.
Implementing these preventive measures can significantly reduce the risk of atherosclerosis and its severe health consequences. By adopting a heart-healthy lifestyle, individuals can improve their overall cardiovascular health and prevent the onset of atherosclerotic disease.
Complications of Atherosclerosis
Atherosclerosis, a progressive condition characterized by the buildup of plaque in the arteries, can lead to several serious health complications. These complications include heart attacks and strokes, peripheral artery disease (PAD), and aortic aneurysms, each associated with significant morbidity and mortality.
Heart Attack and Stroke
The accumulation of atherosclerotic plaque can severely narrow and block arteries, leading to ischemic events such as heart attacks and strokes. Plaque rupture in these arteries can result in the formation of a blood clot, obstructing blood flow to the heart or brain. Heart attacks typically present with symptoms such as chest pain, shortness of breath, and dizziness. Strokes may manifest as sudden numbness or weakness, particularly on one side of the body, difficulty speaking, and loss of coordination. Both conditions are medical emergencies and require immediate treatment to prevent long-term damage or death.
Peripheral Artery Disease
Peripheral artery disease is another significant complication of atherosclerosis, primarily affecting the arteries in the legs and arms. This condition leads to reduced blood flow which can cause symptoms such as leg pain, especially during walking or exercise, and can progress to more severe symptoms including ischemic rest pain. Ischemic rest pain refers to persistent pain in the feet or toes and is often worse at night. PAD can also lead to critical limb ischemia, where severe blockage in the arteries severely reduces blood flow, leading to tissue death and potentially gangrene, which may necessitate limb amputation if left untreated.
Aortic Aneurysms
Atherosclerosis can also lead to the development of aortic aneurysms, particularly abdominal aortic aneurysms (AAA). These aneurysms occur when the wall of the aorta weakens and begins to bulge, which can rupture if not detected and treated early. Rupture of an AAA is a critical condition that can lead to life-threatening internal bleeding. The risk of cardiovascular events, including heart attacks, is also elevated in patients with AAA due to the common underlying atherosclerotic disease.
These complications underscore the importance of managing atherosclerosis through lifestyle changes, medication, and, in some cases, surgical intervention to reduce the progression of the disease and prevent these severe outcomes. Regular health screenings and monitoring of symptoms are crucial for early detection and treatment, helping to improve prognosis and quality of life for those affected by atherosclerosis.
Conclusion
As we have explored, atherosclerosis of the aorta is a complex and progressive disease that poses significant risks to cardiovascular health, but with timely diagnosis and comprehensive management, its impact can be mitigated. The detailed insights into its causes, risk factors, symptoms, and the broad spectrum of diagnostic tools and treatment options highlight the critical importance of early intervention and sustained lifestyle modifications. By understanding the intricate mechanisms of the disease, individuals and healthcare providers can work collaboratively towards preventing its onset or slowing its progression, thereby reducing the potential for severe complications such as heart attacks, strokes, and peripheral artery disease.
Preventive strategies, including adherence to a heart-healthy diet, regular physical activity, smoking cessation, and regular health screenings, are paramount in combating atherosclerosis. The emphasis on managing risk factors and embracing a proactive approach to health underscores the power of preventive care in the realm of cardiovascular diseases. As research continues to evolve, it brings hope for more effective treatments and strategies to address atherosclerosis of the aorta, reinforcing the importance of continual engagement with healthcare professionals and commitment to health-promoting behaviors. Ultimately, this multifaceted approach can significantly enhance the quality of life and outcomes for individuals at risk or already impacted by atherosclerosis.