Understanding the complexities and implications of an atrial septal aneurysm (ASA) is crucial for both patients and healthcare providers. This heart condition, characterized by a significant bulge in the atrial septum, can lead to serious cardiovascular complications if left untreated. Despite its severity, awareness and knowledge about atrial septal aneurysm, including its types, symptoms, and treatment options, remain relatively low. Highlighting the importance of timely diagnosis and intervention, this article aims to shed light on the critical aspects of ASA, underlining why understanding this condition is vital for ensuring patient health and well-being.
The forthcoming sections will provide an in-depth exploration of atrial septal aneurysm, starting with a comprehensive atrial septal aneurysm definition that lays the foundation for a better understanding of the condition. Following this, the article will delve into the various atrial septal aneurysm types, elucidate on the common and less apparent atrial septal aneurysm symptoms, and discuss the potential causes and risk factors. The process of diagnosing ASA, including the critical role of echocardiography in its detection, will be addressed, leading to a discussion on the latest atrial septal aneurysm treatment options available, from medications to surgery. Moreover, the potential complications, the condition’s relation to patent foramen ovale (PFO), and its impact on atrial septal aneurysm life expectancy will be examined, providing a comprehensive overview of what patients and their families should expect and how they can navigate the challenges associated with ASA.
What is Atrial Septal Aneurysm (ASA)?
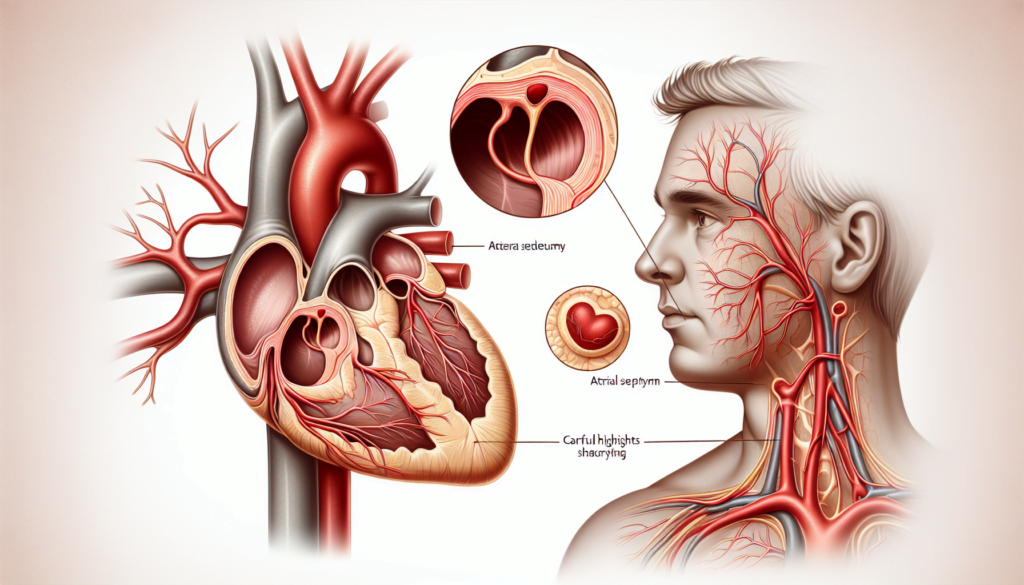
An atrial septal aneurysm (ASA) is a congenital anomaly characterized by an abnormal protrusion of the interatrial septum, the wall that separates the two upper chambers of the heart, known as the atria. This condition manifests as a saccular deformity that bulges into either the right or left atrium and is visible through diagnostic imaging techniques like echocardiography.
The criteria for diagnosing an ASA vary but typically include a protrusion of the interatrial septum by more than 15 mm from its original position in adults, and 5 mm in children. The extent of the protrusion can either be confined to the area of the fossa ovalis—the region in the atrial septum where a patent foramen ovale may occur—or it may involve the entire interatrial septum.
Despite being a rare condition, atrial septal aneurysms are significant due to their association with increased risks of peripheral arterial embolism and stroke. The presence of an ASA can also coincide with other heart anomalies such as atrial septal defects and patent foramen ovale, which can complicate the clinical picture and influence treatment approaches.
In many cases, an ASA does not interfere with the normal flow of blood through the heart and may not require immediate treatment. However, the potential for serious complications necessitates careful monitoring and management, particularly in individuals who exhibit symptoms or have concurrent cardiovascular issues. The development of an ASA is considered to be influenced by congenital factors, specifically anomalies in the septum primum layer of the interatrial septum, although variations in interatrial pressure have also been suggested as contributing factors.
Symptoms of Atrial Septal Aneurysm
Atrial septal aneurysm (ASA) often does not present with noticeable symptoms and is usually identified incidentally during routine echocardiographic examinations or while evaluating other cardiovascular conditions. However, when symptoms do occur, they are typically related to concurrent cardiovascular issues such as arrhythmias, blood clots, or the presence of a patent foramen ovale (PFO).
Common Symptoms
Patients with atrial septal aneurysm may experience a range of symptoms if associated cardiovascular conditions are present:
- Chest Pain or Discomfort: This can occur as a sporadic symptom, often related to the stress on the heart due to the aneurysm’s impact on normal cardiac function.
- Heart Palpitations: Individuals may feel their heart beating rapidly or skipping beats, a direct consequence of arrhythmias often associated with ASA.
- Dizziness: Episodes of dizziness or light-headedness can result from decreased blood flow to the brain due to irregular heart rhythms.
Rare Symptoms
In cases where the ASA leads to more severe complications or coincides with other significant heart defects, additional symptoms may include:
- Shortness of Breath: Particularly noticeable during physical activity, this symptom arises from the heart’s decreased ability to pump blood effectively.
- Fatigue and Reduced Exercise Tolerance: Patients might find themselves unusually tired, especially during or after activities, due to the heart’s impaired functionality.
- Swelling of Legs, Feet, or Belly Area: This can occur due to fluid retention, a common issue in various heart conditions.
It is crucial for individuals diagnosed with ASA, particularly those displaying any of the above symptoms, to undergo thorough medical evaluations to determine the presence of any related cardiovascular issues and to receive appropriate management to mitigate the risk of more serious complications.
Causes and Risk Factors for ASA
The etiology of atrial septal aneurysm (ASA) remains not fully understood, but several factors have been identified that may contribute to its development. These factors can be broadly categorized into congenital links and associated heart conditions.
Congenital Links
ASA is often considered a congenital anomaly, which means it is present at birth. The formation of the heart during fetal development is a complex process that can be influenced by genetic and environmental factors. Research suggests that changes in genes and some medical conditions experienced by the mother during pregnancy can affect this process. Specific risk factors include:
- Genetic Predispositions: Some types of congenital heart defects, including ASA, may run in families, suggesting a genetic component to their development.
- Environmental Influences: Exposure to certain substances or conditions during pregnancy can increase the risk of developing congenital heart defects. These include:
- German measles (rubella) during the first few months of pregnancy.
- Maternal diabetes or lupus.
- Use of certain medications during pregnancy, especially those used to treat seizures and mood disorders.
- Lifestyle factors such as smoking, alcohol misuse, and cocaine use during pregnancy.
These factors highlight the importance of genetic counseling and prenatal care in identifying and managing potential risks to the fetus.
Associated Heart Conditions
Individuals with ASA often have other related heart conditions, which may complicate their clinical picture and influence treatment approaches. The presence of an ASA can increase the risk of:
- Peripheral Arterial Embolism and Stroke: Due to the structural abnormalities in the heart, individuals with ASA are at an increased risk of blood clots, which can lead to stroke.
- Atrial Septal Defects (ASD): ASA is frequently associated with ASD, a condition where there is a hole in the wall between the two upper chambers of the heart.
- Patent Foramen Ovale (PFO): ASA may occur alongside PFO, a small opening in the atrial septum that normally closes shortly after birth but remains open in some individuals.
Healthcare providers may conduct thorough assessments to check for these and other related heart issues when diagnosing and treating ASA. Understanding the full spectrum of associated conditions is crucial for effective management and prevention of complications.
Diagnosis of Atrial Septal Aneurysm
Diagnosing an atrial septal aneurysm (ASA) involves a combination of imaging techniques and a thorough evaluation of the patient’s family health history. These diagnostic tools are essential for confirming the presence of ASA and for assessing its severity and potential complications.
Imaging Techniques
The primary method for diagnosing ASA is echocardiography, which includes both transthoracic (TTE) and transesophageal echocardiography (TEE). TTE involves moving a device across the skin on the left side of the chest and is often the first step in detecting abnormalities in the heart’s structure. However, TTE may not always provide a complete view of the atrial septum.
For a more detailed examination, transesophageal echocardiography (TEE) is used. This procedure involves inserting a device down the esophagus, which allows for a clearer and more comprehensive view of the atrial wall. According to Hanley’s diagnostic criteria, an atrial septum is considered aneurysmal when a dilated segment protrudes at least 15 mm beyond the level surface of the atrial septum. This measurement helps in confirming the diagnosis of ASA.
Additional imaging techniques that may assist in diagnosing ASA include cardiac computed tomography (CT), heart MRI, and angiography. These methods are particularly useful when other heart conditions are suspected or when the echocardiographic findings are inconclusive.
Role of Family History
A detailed family health history is crucial in the diagnosis and management of ASA, as it can reveal genetic predispositions to heart conditions. Collecting a comprehensive family history involves documenting health information from at least three generations of relatives, including any known heart diseases, their onset, and any related complications.
Family health history helps in identifying individuals who may have a higher risk of developing ASA or related cardiovascular conditions. This information is vital for healthcare providers to recommend preventative measures, tailor treatments, and monitor the patient’s health more closely. A well-documented family history can also prompt earlier and more frequent screenings for those at increased risk, potentially leading to timely interventions.
In practice, healthcare providers may use patient questionnaires to gather family history efficiently. These questionnaires often cover various aspects of health and are designed to elicit detailed information about familial diseases, which can be crucial for diagnosing ASA and planning appropriate management strategies.
In conclusion, the diagnosis of atrial septal aneurysm relies heavily on advanced imaging techniques and a comprehensive evaluation of family health history. These diagnostic tools are essential for accurately identifying the condition, understanding its extent, and implementing effective treatment plans to manage the disease and prevent serious complications.
Treatment Options for ASA
Medication
For individuals diagnosed with atrial septal aneurysm (ASA), managing symptoms and reducing the risk of complications are primary goals if the anatomical defect does not warrant immediate surgical intervention. Medications play a crucial role in achieving these objectives, particularly in managing concurrent cardiovascular conditions that can accompany ASA.
- Beta Blockers: These medications are used to manage arrhythmias that can occur with ASA. They help in controlling the heart rate and reducing the incidence of palpitations.
- Anticoagulants (Blood Thinners): Given the increased risk of thrombus formation in patients with ASA, especially those with concurrent patent foramen ovale (PFO), anticoagulants are prescribed to lower the risk of blood clots which can lead to stroke.
- Diuretics: These are used to reduce fluid buildup in the body, a common issue in patients with various heart conditions, helping to alleviate symptoms such as swelling and exertional shortness of breath.
It is important for patients to follow their healthcare provider’s instructions carefully when taking these medications to manage the symptoms effectively and minimize side effects.
Surgical Interventions
Surgical intervention may be necessary for large ASAs or when there is a significant risk of complications like systemic thrombosis or cardiogenic embolism. The decision to proceed with surgery generally depends on the specific characteristics of the aneurysm and associated cardiac anomalies.
- Open-Heart Surgery: This is considered for large aneurysms or when associated defects such as ASD (atrial septal defects) are present. The procedure typically involves a median sternotomy to access the heart, followed by the resection of the ASA. The resection site is then closed with a pericardial patch under cardiopulmonary bypass.
- Catheter-Based Repair: Used primarily for secundum type atrial septal defects, this minimally invasive procedure involves the insertion of a catheter into a vein, usually in the groin, and guiding it to the heart. A mesh patch or plug is then maneuvered through the catheter to close the defect. Over time, heart tissue grows around the patch, effectively sealing the defect.
- Minimally Invasive and Robot-Assisted Heart Surgery: For some patients, particularly those with less extensive aneurysms or those who are high-risk candidates for open-heart surgery, minimally invasive techniques or robot-assisted surgeries may be appropriate. These methods involve smaller incisions, which can lead to quicker recovery times and reduced postoperative complications.
The choice of surgical technique is influenced by various factors including the size and location of the aneurysm, the presence of additional cardiac anomalies, and the overall health of the patient. Continuous monitoring and follow-up care are crucial after surgical intervention to ensure the long-term success of the treatment and to manage any potential complications.
Complications and Associated Conditions
Risk of Stroke
Atrial septal aneurysm (ASA) is associated with a significantly increased risk of stroke, particularly ischemic stroke. This risk is compounded when ASA coexists with patent foramen ovale (PFO), a condition that allows a direct pathway for blood clots to travel from the right to the left side of the heart, potentially reaching the cerebral circulation. Research has shown that ASA is a more critical predictor of recurrent stroke than the size of the PFO itself. In individuals with ASA and recent PFO-associated stroke, the adjusted hazard ratio for recurrent stroke is notably high, emphasizing the need for careful management and consideration of PFO closure in these patients.
The mechanism through which strokes occur in ASA patients often involves the formation of thrombi within the aneurysmal sac of the interatrial septum. These thrombi can dislodge and embolize to the brain, leading to stroke. This process may be exacerbated by the presence of atrial fibrillation, which is commonly associated with ASA and further increases the risk of thrombus formation.
Other Health Issues
In addition to stroke, individuals with atrial septal aneurysm face several other health complications, particularly if the condition is associated with larger atrial septal defects (ASD). These complications can include:
- Right-Sided Heart Failure: The increased blood flow to the right side of the heart can lead to dilation and eventual heart failure.
- Arrhythmias: Irregular heartbeats are common due to the structural changes in the heart and increased strain.
- Pulmonary Hypertension: This serious condition arises from increased pressure in the lung arteries and can lead to permanent lung damage and Eisenmenger syndrome. Eisenmenger syndrome develops over many years and is characterized by reversed blood flow due to high pulmonary artery pressure, leading to cyanosis, dyspnea on exertion, and an increased risk of infection.
- Exercise Intolerance and Increased Mortality: Large defects that remain untreated can severely limit physical activity and increase the risk of early death.
- Increased Incidence of Pneumonia: The altered blood flow and pressure dynamics in the lungs make individuals more susceptible to respiratory infections.
Managing these complications often requires a multifaceted approach, including medication to manage symptoms, and in some cases, surgical interventions to repair the structural defects. Continuous monitoring and comprehensive cardiovascular care are crucial to mitigate these risks and improve the quality of life for individuals affected by ASA and associated conditions.
Conclusion
Through this article, we have traversed the intricate landscape of atrial septal aneurysm (ASA), unveiling its complexities from definition and diagnosis to treatment options and potential complications. The importance of early detection and tailored management strategies has been underscored, highlighting the role of echocardiography in diagnostics and the spectrum of treatment modalities available, from medications to address symptomatic concerns to surgical interventions for more severe manifestations. This journey underscores the significance of a comprehensive understanding of ASA, not only for healthcare professionals but also for patients and their families navigating this condition.
Reflecting on the broader implications, it’s clear that ASA represents a critical concern within cardiovascular health that demands ongoing attention and research. The discussion of its association with increased risks, particularly of stroke, reinforces the need for heightened awareness and proactive management. As the medical community continues to explore innovative treatment approaches and preventive measures, this article serves as a reminder of the power of informed awareness and the importance of advancing our collective knowledge to improve outcomes for individuals affected by atrial septal aneurysm.