Autonomic dysreflexia is a serious medical condition that can have life-threatening consequences if not properly managed. This condition affects individuals with spinal cord injuries above the T6 level, causing a sudden and dangerous increase in blood pressure. Understanding the causes, symptoms, and treatment options for autonomic dysreflexia is crucial for those at risk and their caregivers to ensure prompt and effective intervention.
This article delves into the complexities of autonomic dysreflexia treatment, exploring its underlying mechanisms and diagnostic approaches. It also examines long-term management strategies to help individuals with spinal cord injuries maintain their health and quality of life. By shedding light on this critical topic, we aim to equip readers with the knowledge to recognize and respond to autonomic dysreflexia symptoms, potentially saving lives and improving overall well-being for those affected by this condition.
Pathophysiology of Autonomic Dysreflexia
The Autonomic Nervous System
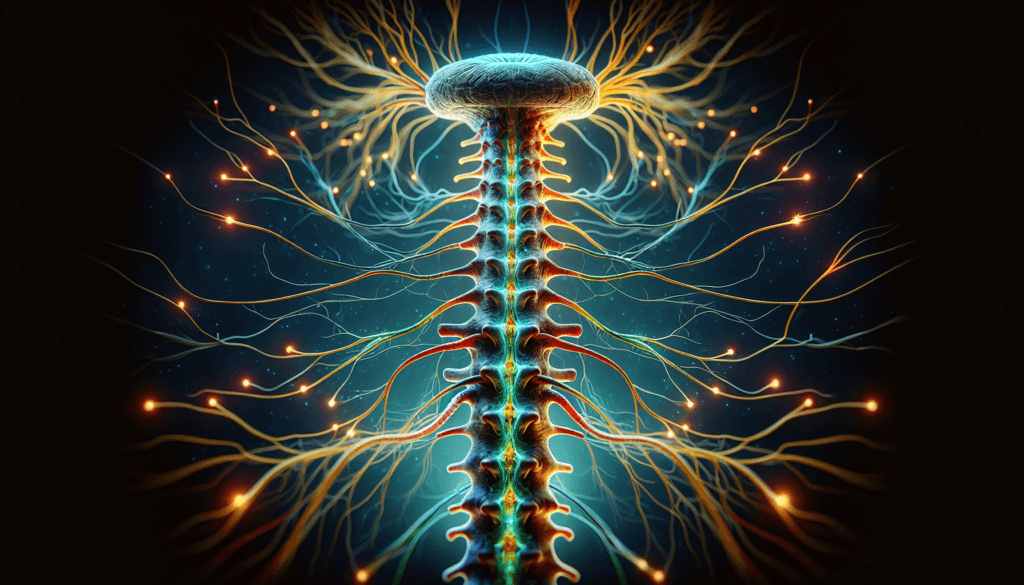
The autonomic nervous system regulates involuntary functions such as heart rate, blood pressure, and digestion. It consists of two main divisions: the sympathetic and parasympathetic nervous systems. The sympathetic nervous system is responsible for the “fight or flight” response, increasing heart rate and blood pressure in response to stress or danger. The parasympathetic nervous system, on the other hand, promotes rest and relaxation, slowing heart rate and decreasing blood pressure.
In a healthy individual, these two systems work together to maintain homeostasis. However, in individuals with spinal cord injuries, the balance between the sympathetic and parasympathetic nervous systems can be disrupted, leading to autonomic dysreflexia.
Spinal Cord Injury and AD
Spinal cord injuries above the T6 level can disrupt the descending control of the sympathetic nervous system, leaving the spinal cord below the injury level without regulation. When a noxious stimulus, such as a full bladder or bowel, occurs below the level of the injury, it can trigger an uncontrolled sympathetic response. This response causes vasoconstriction, leading to a sudden and dangerous increase in blood pressure.
Simultaneously, the parasympathetic nervous system attempts to counteract this hypertension by slowing the heart rate and dilating blood vessels above the level of the injury. However, due to the spinal cord injury, the parasympathetic signals cannot travel past the lesion to counteract the sympathetic response below the injury, resulting in the characteristic symptoms of autonomic dysreflexia.
RELATED: Pseudomyxoma Peritonei: Diagnosis, Treatment Options, and Prognosis
Neurological Mechanisms
The exact neurological mechanisms underlying autonomic dysreflexia are not fully understood, but several factors are thought to contribute to its development. One proposed mechanism involves the sprouting of new sympathetic nerve fibers around the injury site, leading to an increased sensitivity to stimuli below the lesion.
Additionally, changes in the properties of spinal cord neurons below the injury may also play a role. These neurons may become more excitable and responsive to stimuli, further contributing to the exaggerated sympathetic response seen in autonomic dysreflexia.
Research suggests that alterations in the balance of neurotransmitters, such as glutamate and GABA, in the spinal cord may also be involved in the pathogenesis of autonomic dysreflexia. An increased ratio of excitatory to inhibitory neurotransmitters could lead to the heightened sympathetic activity observed in this condition.
Diagnostic Approaches
Clinical Assessment
Diagnosing autonomic dysreflexia begins with a thorough clinical assessment. Healthcare providers must be vigilant in identifying the signs and symptoms of this potentially life-threatening condition, especially in individuals with spinal cord injuries above the T6 level. Key elements of the clinical assessment include measuring blood pressure, assessing heart rate, and evaluating the presence of other autonomic dysreflexia symptoms such as headache, sweating, and flushing above the level of the injury.
Obtaining a detailed medical history is crucial, particularly regarding the individual’s spinal cord injury and any previous episodes of autonomic dysreflexia. This information can help healthcare providers determine the severity of the condition and identify potential triggers. Additionally, a physical examination should be performed to assess for any noxious stimuli below the level of the injury, such as a distended bladder, fecal impaction, or pressure ulcers.
Blood Pressure Monitoring
Monitoring blood pressure is a critical component of diagnosing autonomic dysreflexia. A sudden increase in systolic blood pressure of 20-40 mmHg above the individual’s baseline is a hallmark sign of this condition. Healthcare providers should measure blood pressure frequently during an episode of autonomic dysreflexia and continue monitoring it closely until the episode resolves.
In some cases, individuals with spinal cord injuries may experience silent autonomic dysreflexia, where they have elevated blood pressure without any other apparent symptoms. Regular blood pressure monitoring during routine activities can help detect these episodes and prompt further investigation into potential triggers.
RELATED: Progeria: Essential Information on Symptoms and Treatment
Additional Tests
In addition to clinical assessment and blood pressure monitoring, several tests may be performed to rule out other conditions that can mimic autonomic dysreflexia symptoms or to identify underlying triggers. These tests may include:
- Urinalysis and urine culture: To detect urinary tract infections, which can trigger autonomic dysreflexia.
- Imaging studies: Such as X-rays, CT scans, or MRI scans, to identify potential sources of noxious stimuli, such as fractures, kidney stones, or spinal cord compression.
- Electrocardiogram (ECG): To assess heart rhythm and rule out cardiac causes of symptoms.
- Blood tests: To evaluate electrolyte imbalances, anemia, or other systemic conditions that may contribute to autonomic instability.
By combining a thorough clinical assessment, regular blood pressure monitoring, and appropriate diagnostic tests, healthcare providers can accurately diagnose autonomic dysreflexia and identify potential triggers. This approach allows for prompt and effective treatment, which is essential for preventing complications and ensuring the well-being of individuals with spinal cord injuries.
Long-term Management Strategies
Lifestyle Modifications
Lifestyle modifications play a crucial role in the long-term management of autonomic dysreflexia. Individuals with spinal cord injuries should be educated about potential triggers and how to avoid them. This includes maintaining a regular bladder and bowel routine to prevent distension and irritation. Wearing loose-fitting clothing and shoes can help minimize skin irritation and pressure sores. Daily skin inspections are essential to identify and treat any cuts, bruises, or other signs of trauma below the level of injury. Avoiding extreme temperatures and using appropriate clothing for the weather conditions can also help prevent episodes of autonomic dysreflexia.
Medication Management
In some cases, lifestyle modifications alone may not be sufficient to control autonomic dysreflexia, and medication management may be necessary. Alpha-adrenergic blocking agents, such as terazosin, have been shown to be effective in reducing the frequency and severity of autonomic dysreflexia episodes. These medications work by blocking the effects of norepinephrine, a neurotransmitter that causes vasoconstriction and increases blood pressure. Nitrates, such as nitroglycerin paste, may also be used to help reduce hypertension and irregular heartbeats during an episode. It is essential for individuals with spinal cord injuries to work closely with their healthcare providers to develop an appropriate medication regimen based on their specific needs and medical history.
RELATED: Prion Disease: What You Need to Know About This Rare Condition
Rehabilitation Techniques
Rehabilitation techniques can also play a role in the long-term management of autonomic dysreflexia. Techniques such as biofeedback training and relaxation exercises may help individuals with spinal cord injuries better control their physiological responses to triggers. Biofeedback involves using electronic devices to monitor bodily functions, such as heart rate and blood pressure, and providing feedback to help the individual learn to control these functions consciously. Relaxation techniques, such as deep breathing and progressive muscle relaxation, can help reduce stress and anxiety, which may contribute to episodes of autonomic dysreflexia. Physical therapy and occupational therapy can also help individuals with spinal cord injuries maintain their overall health and function, reducing the risk of complications that may trigger autonomic dysreflexia.
Conclusion
Managing autonomic dysreflexia effectively requires a comprehensive approach that combines medical intervention, lifestyle adjustments, and ongoing education. By understanding the triggers and symptoms of this condition, individuals with spinal cord injuries can take proactive steps to prevent episodes and respond quickly when they occur. This knowledge empowers patients and caregivers alike, leading to improved quality of life and reduced risk of complications.
The strategies discussed in this article offer a roadmap to better health for those affected by autonomic dysreflexia. From careful monitoring and prompt treatment to long-term management through medication and rehabilitation techniques, these approaches provide a solid foundation for managing this complex condition. As research continues, new insights and treatments may emerge, offering hope for even more effective ways to address the challenges of autonomic dysreflexia in the future.