Avascular necrosis, also known as osteonecrosis, is a serious condition that affects bone tissue. This debilitating disorder occurs when blood supply to a bone is disrupted, leading to bone cell death and eventual collapse of the affected area. Avascular necrosis can have a profound impact on a person’s quality of life, causing pain, limited mobility, and potentially requiring joint replacement surgery if left untreated.
Understanding the early signs, causes, and effective treatments of avascular necrosis is crucial to manage this condition. This article delves into the key symptoms across different joints, explores the underlying factors that trigger the disease, and examines comprehensive strategies to address it. By shedding light on these aspects, individuals can better recognize the warning signs and seek timely medical attention, potentially improving their outcomes and preserving joint function.
Avascular Necrosis: An Overview
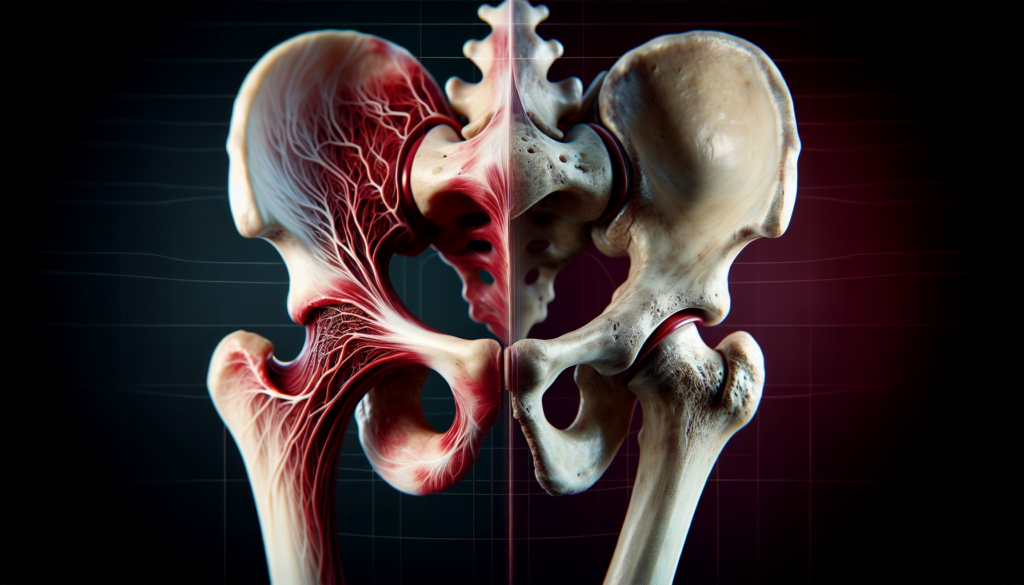
Avascular necrosis, also known as osteonecrosis, is a serious condition that results from the temporary or permanent loss of blood supply to the bone. This disruption in blood flow leads to the death of bone tissue and eventual collapse of the affected area. If avascular necrosis occurs near a joint, it may cause the joint surface to collapse. While this condition can affect any bone, it most commonly impacts the ends of long bones, such as the femur.
The prevalence of avascular necrosis varies depending on the underlying cause and the specific joint affected. However, it is estimated that up to 20,000 new cases are diagnosed each year in the United States alone. This condition typically affects individuals between the ages of 30 and 50, with males being more commonly affected than females.
Avascular necrosis can occur in any bone, but it most frequently affects the following joints:
- Hip (femoral head)
- Knee (femoral condyles)
- Shoulder (humeral head)
- Ankle (talus)
- Wrist (scaphoid and lunate)
RELATED: Chickenpox: In-Depth Look at Causes and Treatments
The consequences of avascular necrosis can be both short-term and long-term. In the short term, patients may experience pain, stiffness, and reduced range of motion in the affected joint. As the condition progresses, the bone and joint may begin to collapse, leading to more severe pain and disability.
If left untreated, avascular necrosis can have significant long-term consequences. The progressive destruction of the joint can result in osteoarthritis, requiring joint replacement surgery to restore function and alleviate pain. In some cases, the affected bone may fracture, leading to further complications and prolonged recovery times.
Understanding the risk factors, early signs, and available treatment options for avascular necrosis is crucial for timely intervention and the preservation of joint function. By recognizing the warning signs and seeking prompt medical attention, individuals can improve their outcomes and minimize the long-term impact of this debilitating condition.
Identifying Early Symptoms Across Different Joints
Avascular necrosis (AVN) can affect various joints in the body, with the hip being the most common site, followed by the knee, shoulder, ankle, elbow, and wrist. Early recognition of symptoms is crucial for timely intervention and preserving joint function.
In the early stages of AVN, patients may experience minimal joint pain, which gradually increases as the bone and joint begin to collapse. Limited range of motion due to pain is another common symptom. However, the specific signs and symptoms can vary depending on the affected joint.
Hip-specific signs
Osteonecrosis of the hip often has early stages that are asymptomatic. As the condition progresses, patients may experience pain in the hip and groin area, especially during weight-bearing activities. Associated symptoms can include referred pain in the buttock and thigh, as well as stiffness and changes in gait.
Knee and shoulder symptoms
Osteonecrosis of the knee most commonly presents as acute onset knee pain that occurs while weight-bearing and at night. On physical examination, pain with palpation over the medial femoral condyle and decreased range of motion are observed.
In the shoulder, osteonecrosis involving the proximal humerus is characterized by pulsating pain that radiates to the elbow and a decreased active range of motion.
Less common sites of AVN
Osteonecrosis of the talus is associated with polyarticular disease and trauma. Patients often complain of pain and difficulty ambulating well beyond the expected recovery time following a traumatic event.
In the wrist, osteonecrosis of the lunate (Kienböck disease) and scaphoid (Preiser disease) most often presents without a history of trauma. Patients, usually skilled laborers, complain of unilateral pain in the dorsal and radial aspects of the wrist, along with decreased range of motion, swelling, and weakened grip strength.
Recognizing these early signs and symptoms across different joints is essential for prompt diagnosis and appropriate management of avascular necrosis, potentially improving outcomes and preserving joint function.
Underlying Causes and Triggering Factors
Avascular necrosis has a multifactorial etiology, with various factors contributing to the disruption of blood supply to the bone. These factors can be broadly categorized into traumatic and non-traumatic causes.
Traumatic vs. non-traumatic causes
Traumatic causes of avascular necrosis include fractures and dislocations that can damage nearby blood vessels, leading to a compromised blood supply to the bone. On the other hand, non-traumatic causes encompass a wide range of factors, such as medication side effects, alcohol abuse, and certain medical conditions that can impair blood flow to the bone.
Medication-induced AVN
Long-term use of corticosteroids is a significant risk factor for developing avascular necrosis. These medications can increase lipid levels in the blood, reducing blood flow and leading to the formation of fat emboli within the bone vasculature. Other medications, such as bisphosphonates used to treat osteoporosis and certain cancers, have also been associated with an increased risk of osteonecrosis, particularly in the jaw.
RELATED: Bell’s Palsy: Symptoms, Causes, and Comprehensive Treatment Guide
Systemic diseases linked to AVN
Several systemic diseases have been linked to the development of avascular necrosis. These include:
- Sickle cell anemia: The abnormally shaped red blood cells can obstruct small blood vessels, leading to decreased blood flow to the bone.
- Systemic lupus erythematosus (SLE): This autoimmune disorder can cause inflammation and damage to blood vessels, compromising the blood supply to the bone.
- HIV/AIDS: The virus itself and the medications used to treat it can increase the risk of developing avascular necrosis.
- Gaucher’s disease: This genetic disorder leads to the accumulation of fatty substances within cells, which can impair blood flow and cause avascular necrosis.
Other factors that may contribute to the development of avascular necrosis include alcohol abuse, which can lead to fatty deposits in the blood vessels, and radiation therapy, which can weaken the bone and damage blood vessels. In some cases, the exact cause of avascular necrosis remains unknown, and these instances are classified as idiopathic osteonecrosis.
Comprehensive Management Strategies
The management of avascular necrosis (AVN) involves a comprehensive approach tailored to the stage and severity of the disease, as well as the affected joint. Treatment options range from conservative measures to surgical interventions, with the goal of preserving joint function and alleviating pain.
Early-stage treatments for AVN aim to prevent further progression of the disease and promote bone healing. These may include:
- Protected weight-bearing and activity modification to reduce stress on the affected joint
- Pharmacological therapies, such as bisphosphonates which may slow disease progression and delay the need for surgical intervention
- Extracorporeal shockwave therapy (ESWT) and hyperbaric oxygen therapy (HBOT), which have shown beneficial effects in early-stage AVN of the femoral head
RELATED: Bipolar Disorder: Symptoms, Diagnosis, and Treatment
When conservative measures fail or the disease progresses to advanced stages, surgical options become necessary. The choice of surgical procedure depends on the location and extent of the necrotic lesion, as well as patient factors such as age and overall health. Surgical options for advanced AVN include:
- Core decompression: A minimally invasive procedure that involves drilling small holes into the affected bone to reduce pressure and stimulate blood flow. This is most effective in early-stage AVN.
- Bone grafting: The use of healthy bone tissue to support the affected area and promote healing. This may be combined with core decompression.
- Osteotomy: A procedure that involves cutting and realigning the bone to shift weight-bearing away from the necrotic area.
- Arthroplasty: In advanced cases with severe joint damage, joint replacement surgery (e.g., total hip arthroplasty) may be necessary to restore function and alleviate pain.
Rehabilitation and follow-up care are crucial components of the comprehensive management of AVN. Physical therapy plays a vital role in postoperative recovery, helping patients regain strength, mobility, and function. Rehabilitation programs are tailored to the specific surgical procedure and the patient’s individual needs. Regular follow-up with the healthcare team is essential to monitor the patient’s progress, assess the effectiveness of the treatment, and make any necessary adjustments to the management plan.
Conclusion
Avascular necrosis has a significant impact on bone health and joint function, causing pain and potentially leading to joint collapse. Early detection and proper management are crucial to slow down its progression and preserve joint integrity. Understanding the risk factors, recognizing early symptoms across different joints, and being aware of the available treatment options empower patients and healthcare providers to tackle this condition head-on.
The journey to manage avascular necrosis is ongoing, with advancements in both conservative and surgical approaches offering hope to those affected. From activity modification and medication to cutting-edge surgical techniques, the range of treatments continues to expand. As research progresses, new insights into the underlying mechanisms of avascular necrosis may pave the way for more targeted and effective therapies, improving outcomes for patients grappling with this challenging condition.