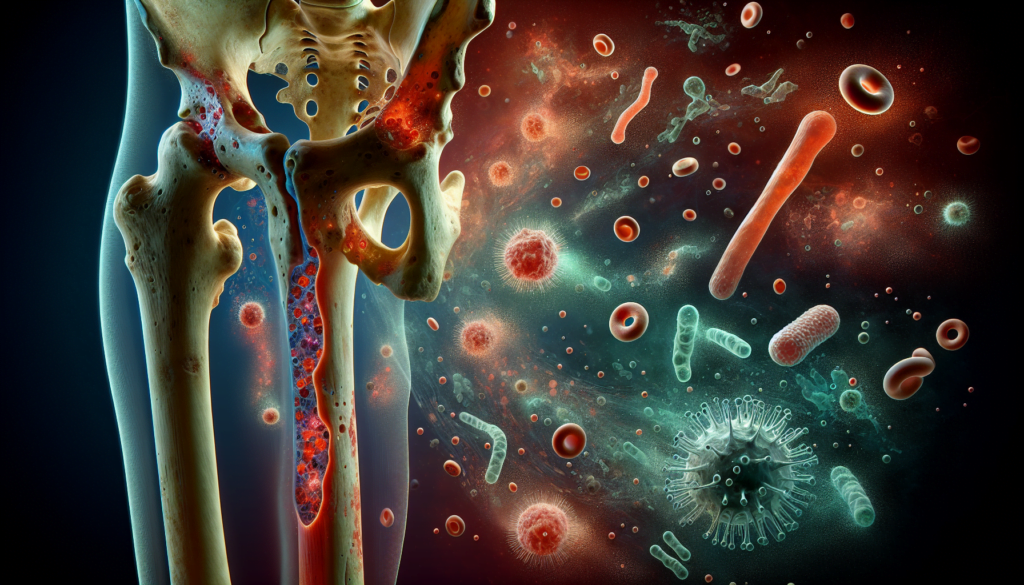
Bone infections, known medically as osteomyelitis, pose a significant health challenge that can affect people of all ages. This condition occurs when bacteria or fungi invade bone tissue, leading to inflammation and potential damage. Osteomyelitis (Bone Infection) can have serious consequences if left untreated, making early detection and proper management crucial for better outcomes.
Understanding the symptoms, diagnosis, and treatment options for osteomyelitis is essential for both patients and healthcare providers. This article delves into the nature of bone infections, exploring common signs to watch for and the various approaches used to identify and address this condition. It also sheds light on the available treatment strategies, highlighting the importance of prompt and appropriate care to combat this potentially debilitating infection.
What is Osteomyelitis?
Osteomyelitis is a serious infection of the bone that can be either acute or chronic. It is an inflammatory process involving the bone and its structures caused by pyogenic organisms that spread through the bloodstream, fractures, or surgery.
Definition
Osteomyelitis can be broken down into “osteo” meaning bone, and “myelitis”, meaning inflammation of the fatty tissues within the bone. It is caused by an infection of the bone or joint, and can be both acute and chronic. It can occur at any age and involve any bone.
Types of Osteomyelitis
Traditionally, osteomyelitis is classified into three categories:
- Hematogenous osteomyelitis: a bone infection that has spread through the bloodstream
- Osteomyelitis caused by bacteria that gain access to bone directly from an adjacent focus of infection (seen with trauma or surgery)
- Osteomyelitis that is the result of diabetic foot infection or any other reason for diminished blood supply to the bones
RELATED: Spinal Stenosis Explained: Symptoms, Diagnosis, and Treatment Options
Causes and Risk Factors
These infections can be due to one, or many types of bacteria and/or fungi. In order of frequency, osteomyelitis can be the result of:
- Trauma, surgery, or joint insertion or any type of prosthetic material
- Lack of blood flow in diabetes associated foot infections
- An infection that has spread via the blood and has reached the bone (seen mostly in prepubescent children or the elderly)
Among children and teens, the long bones of the legs and arms are most frequently affected. In adults, osteomyelitis most often affects the vertebrae of the spine and/or the hips. However, extremities are frequently involved due to skin wounds, trauma and surgeries.
Recognizing Osteomyelitis Symptoms
The signs and symptoms of osteomyelitis can vary depending on the location and severity of the infection. Patients may experience localized pain, swelling, warmth, and redness over the affected area. Fever, chills, and fatigue are also common systemic symptoms. In some cases, particularly in infants, older adults, and immunocompromised individuals, the signs and symptoms may be subtle or difficult to distinguish from other conditions.
Common Signs and Symptoms
- Pain in the affected area, which may worsen with movement or pressure
- Swelling, warmth, and redness over the site of infection
- Fever, which can be high in acute osteomyelitis cases
- Fatigue and general malaise
- Drainage of pus from the infected area in some cases
Symptoms in Children vs. Adults
While the general symptoms of osteomyelitis are similar in children and adults, there are some key differences to note:
| Children | Adults |
|---|---|
| More likely to have acute osteomyelitis | More likely to have chronic osteomyelitis |
| Long bones of the arms and legs are most frequently affected | Vertebrae and hips are more commonly involved |
| May present with irritability, lethargy, or refusal to bear weight on the affected limb | May experience back pain or neurological symptoms if the spine is involved |
RELATED: SIDS (Sudden Infant Death Syndrome): Comprehensive Guide for Parents
When to Seek Medical Attention
It is crucial to seek prompt medical attention if you or your child experience:
- Worsening bone pain accompanied by fever
- Signs of infection, such as redness, swelling, or drainage
- Persistent pain or limited movement in a joint
- Symptoms that do not improve with rest or over-the-counter pain medication
Early diagnosis and treatment are essential for preventing complications and ensuring the best possible outcome in osteomyelitis cases. If you are at a higher risk of infection due to a medical condition, recent surgery, or injury, be particularly vigilant for signs and symptoms of osteomyelitis.
Diagnosis and Testing
Diagnosing osteomyelitis involves a combination of physical examination, imaging tests, laboratory tests, and bone biopsy. Physicians begin by examining the affected area for signs of tenderness, swelling, and warmth. They may also probe foot ulcers to assess the proximity of the underlying bone.
Imaging tests play a crucial role in diagnosing osteomyelitis. X-rays can reveal bone damage, but changes may not be visible until several weeks after the infection has developed. MRI scans provide detailed images of bones and surrounding soft tissues, making them highly sensitive for detecting early stages of osteomyelitis. CT scans offer cross-sectional views and are useful when MRI is not an option. Bone scans, such as three-phase bone scanning and labeled white blood cell scanning, can also aid in diagnosis.
Laboratory tests, including complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), are used to evaluate leukocytosis, anemia, and inflammation. Blood cultures may identify the causative pathogen in cases of hematogenous osteomyelitis. However, blood tests alone cannot definitively diagnose osteomyelitis.
Bone biopsy is the gold standard for diagnosing osteomyelitis and identifying the specific pathogen causing the infection. The procedure involves removing a sample of bone tissue through open surgery or needle biopsy. The sample undergoes histopathological examination and culture to determine the presence of infection and the responsible microorganism. This information is crucial for selecting the most effective antibiotic treatment.
Accurate diagnosis of osteomyelitis requires a comprehensive approach that combines physical examination findings, imaging results, laboratory data, and bone biopsy analysis. Early detection and identification of the causative pathogen are essential for initiating appropriate treatment and preventing complications associated with this serious bone infection.
Treatment Approaches
Treatment of osteomyelitis involves a combination of antibiotic therapy and surgical interventions to eliminate the infection, manage pain, and prevent complications. The specific approach depends on the severity and location of the infection, as well as the patient’s overall health.
Antibiotic Therapy
Antibiotics are the cornerstone of osteomyelitis treatment. The choice of antibiotic depends on the results of bone biopsy cultures and sensitivity tests. Intravenous antibiotics are usually administered for 4-6 weeks to achieve adequate bone penetration and maintain therapeutic levels. Common antibiotics used include:
- Beta-lactam antibiotics (e.g., penicillin, cephalosporins)
- Lincosamides
- Gyrase inhibitors (e.g., fluoroquinolones)
In some cases, combination therapy may be used to target specific pathogens or address implant-related infections. Oral antibiotics may be prescribed for an additional period after completing the intravenous course.
Surgical Interventions
Surgery plays a crucial role in the management of chronic osteomyelitis. The main goals of surgical treatment are to remove necrotic bone (sequestrum), drain abscesses, and promote healing. Surgical options include:
- Debridement: Removal of infected and necrotic bone tissue
- Sequestrectomy: Excision of sequestrum
- Dead space management: Filling the void left after debridement with antibiotic-impregnated materials (e.g., PMMA beads, bone grafts)
- Soft tissue reconstruction: Coverage of the wound with healthy tissue using local flaps or free tissue transfer
In some cases, external fixation devices may be used to stabilize the affected bone during the healing process.
RELATED: Salmonella Infections: Key Facts and Safety Tips
Pain Management
Pain control is an essential aspect of osteomyelitis management. Adequate analgesia helps improve patient comfort and facilitates early mobilization. Options for pain management include:
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Opioid analgesics
- Nerve blocks or regional anesthesia
Long-term Care
Patients with chronic osteomyelitis require long-term follow-up and care to prevent recurrence and manage any residual disability. This may involve:
- Regular monitoring of inflammatory markers (e.g., ESR, CRP)
- Periodic radiographic imaging to assess bone healing
- Rehabilitation and physical therapy to restore function
- Nutritional support to promote wound healing
- Patient education on proper wound care and signs of infection
In some cases, suppressive antibiotic therapy may be necessary to control the infection and prevent acute exacerbations.
Successful treatment of osteomyelitis requires a multidisciplinary approach involving orthopedic surgeons, infectious disease specialists, plastic surgeons, and rehabilitation professionals. Early diagnosis and prompt initiation of appropriate therapy are essential to achieve the best outcomes and minimize the risk of complications.
Conclusion
Osteomyelitis poses a significant health challenge, requiring prompt diagnosis and treatment to prevent serious complications. The condition has an impact on people of all ages, with varied symptoms and potential causes ranging from direct injury to bloodstream infections. Early recognition of signs such as localized pain, swelling, and fever is crucial to seek timely medical attention. Accurate diagnosis involves a combination of physical examination, imaging tests, and bone biopsy to identify the specific pathogen causing the infection.
Managing osteomyelitis calls for a multifaceted approach, combining antibiotic therapy with surgical interventions when necessary. Long-term care and follow-up are essential to monitor healing progress and prevent recurrence. By understanding the nature of bone infections and available treatment strategies, patients and healthcare providers can work together to tackle this potentially debilitating condition effectively. This knowledge empowers individuals to recognize warning signs early and seek appropriate care, ultimately leading to better outcomes in the fight against osteomyelitis.