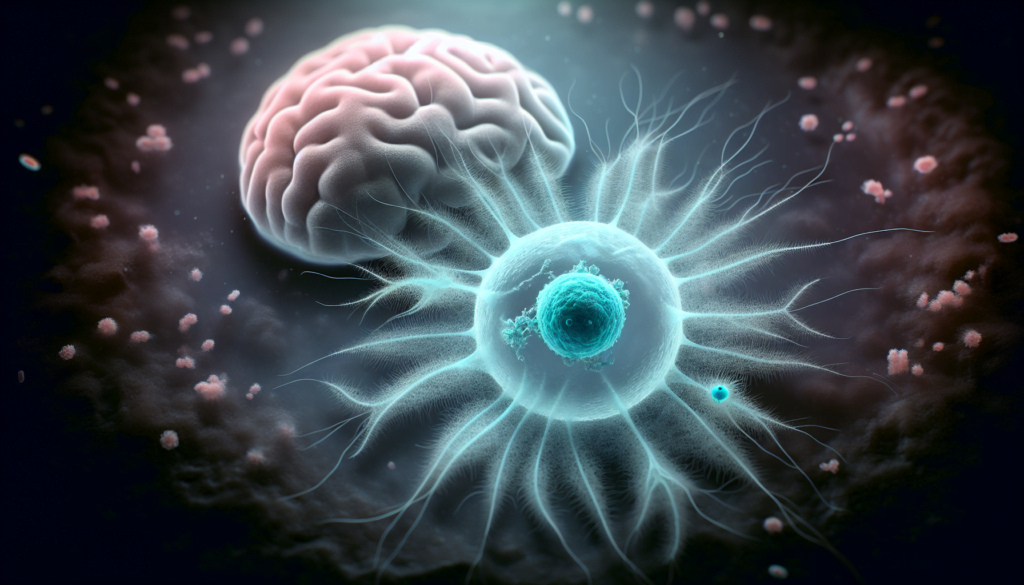
The Brain-Eating Amoeba, a rare but deadly microorganism, has gained attention due to its alarming effects on the human body. This microscopic creature, scientifically known as Naegleria fowleri, thrives in warm freshwater environments and can cause a fatal infection when it enters the human brain through the nose. Its ability to destroy brain tissue rapidly has led to widespread concern and a need for increased awareness among the public and medical professionals alike.
This article delves into the critical aspects of the Brain-Eating Amoeba, providing essential information for readers. It explores the nature of this organism, highlights early warning signs to watch for, and examines current treatment approaches. Additionally, the article discusses survival rates and presents case studies to offer a comprehensive understanding of this rare but serious condition. By shedding light on this topic, we aim to equip readers with knowledge that could potentially save lives.
Understanding Brain-Eating Amoeba
Scientific classification
Naegleria fowleri, commonly known as the brain-eating amoeba, belongs to the phylum Percolozoa and is classified as an amoeboflagellate excavate. This free-living microorganism is capable of behaving as both an amoeba and a flagellate. It was named after Malcolm Fowler, who described the initial cases of primary amebic meningoencephalitis (PAM) caused by N. fowleri in Australia.
Geographic distribution
N. fowleri is ubiquitous and found mostly in freshwater lakes, hot water springs, poorly chlorinated pools, and thermally polluted water bodies worldwide. It has been reported in Australia, where this organism was first identified, as well as New Zealand, Europe, Africa, Asia, and Latin America. In the United States, it has mostly been found in the southern states, with more than half of all infections occurring in Florida and Texas. However, more recently, it has also been isolated from thermally polluted waters in northern states like Connecticut and Minnesota.
RELATED: Toxic Shock Syndrome: Key Information for Safe Tampon Use
Infection mechanism
N. fowleri causes severe damage to the central nervous system because of its pathogenicity and the intense immune response it elicits. The trophozoite stage is the infective phase for humans, during which the organism can actively feed and replicate. The trophozoite attaches to the olfactory epithelium, follows the axons of olfactory receptor neurons through the cribriform plate in the nasal cavity, and enters the brain. Once N. fowleri reaches the olfactory bulbs, it elicits a significant innate immune response through activation of macrophages and neutrophils. The amoeba’s virulence depends on the protein Nfa1, nitric oxide production, and pore-forming proteins. Nfa1 mediates amebic attachment to target cells, while the secretion of cytolytic molecules like cysteine proteases, phospholipases, and phospholipolytic enzymes mediates extensive necrosis. This intense immune response and the amoeba’s virulence lead to significant destruction of brain parenchymal tissue in PAM.
Recognizing Early Warning Signs
Common initial symptoms
The initial symptoms of a brain-eating amoeba infection usually appear within 1 to 9 days after exposure to contaminated water. These symptoms can include headache, fever, nausea, and vomiting. It is crucial to seek medical attention immediately if these symptoms develop, especially if there has been recent exposure to warm freshwater.
Easily mistaken conditions
The early symptoms of a brain-eating amoeba infection are similar to those caused by other more common illnesses, such as bacterial meningitis. This similarity can make it challenging to diagnose the infection promptly. However, providing information about recent freshwater exposure to medical professionals can help them consider the possibility of a brain-eating amoeba infection.
When to seek medical help
If you or a loved one experiences a sudden onset of symptoms such as fever, headache, stiff neck, and vomiting, it is essential to seek medical care immediately. These symptoms can progress rapidly, and prompt medical attention is critical for the best possible outcome. As the infection progresses, additional symptoms may include confusion, lack of attention to surroundings, loss of balance, seizures, and hallucinations. Timely diagnosis and treatment are crucial in the fight against this rare but deadly infection caused by the brain-eating amoeba, Naegleria fowleri.
Current Treatment Approaches
Standard treatment protocol
The standard treatment protocol for primary amebic meningoencephalitis caused by the brain-eating amoeba Naegleria fowleri involves a combination of medications. The cornerstone of therapy is amphotericin B, administered both intravenously and intrathecally. The Centers for Disease Control and Prevention (CDC) recommends conventional amphotericin B over liposomal formulations due to its lower minimum inhibitory concentration against N. fowleri. The recommended intravenous dose is 1.5 mg/kg/day in two divided doses for three days, followed by 1 mg/kg/day once daily for an additional 11 days, totaling a 14-day course. Intrathecal amphotericin B should be administered at 1.5 mg/day for two days, followed by 1 mg/day every other day for eight days, resulting in a 10-day course. Additional medications in the standard regimen include azithromycin, fluconazole, rifampin, miltefosine, and dexamethasone. These drugs have demonstrated antiamebic activity against N. fowleri in laboratory studies and have been used in successful survivor cases.
RELATED: Torticollis: A Detailed Look at Symptoms, Causes, and Management
Emerging therapies
While amphotericin B remains the primary drug of choice for treating brain-eating amoeba infections, its use is associated with significant side effects, including potentially use-limiting renal toxicity. Corifungin, a new drug entity granted orphan drug status for the treatment of primary amebic meningoencephalitis, has shown superior activity to amphotericin B in mouse models. Its increased aqueous solubility may enhance blood-brain barrier penetration and reduce renal toxicity, although human studies have yet to confirm these potential therapeutic benefits. Miltefosine, an oral medication, has also emerged as a promising treatment option, with in vitro efficacy against N. fowleri and successful use in recent survivor cases. The CDC has made miltefosine available through an investigational new drug protocol for infections caused by free-living amoebae.
Challenges in treatment
Despite advances in treatment options, the mortality rate for primary amebic meningoencephalitis caused by brain-eating amoeba remains exceptionally high, with few survivors documented worldwide. The rapid progression of the disease and the difficulty in early diagnosis pose significant challenges in initiating timely and effective treatment. Moreover, the rarity of N. fowleri infections has precluded clinical trials to assess the comparative efficacy of different treatment regimens, leaving clinicians to rely on case reports and in vitro studies to guide therapeutic decisions. Balancing the potential benefits and risks of aggressive treatment, such as the use of high-dose amphotericin B and investigational drugs like miltefosine, further complicates the management of this devastating infection. Continued research into new therapeutic agents and strategies is crucial to improve outcomes for patients affected by brain-eating amoeba.
Survival Rates and Case Studies
Historical survival statistics
Historically, the survival rate for primary amebic meningoencephalitis caused by the brain-eating amoeba Naegleria fowleri has been extremely low, with a case-fatality rate of over 97%. From 1962 to 2018, only 7 out of 381 well-documented cases worldwide were reported to have survived this devastating infection. The majority of these survivors were from the United States, where 4 out of 143 known cases managed to recover from PAM between 1962 and 2017. This underscores the critical nature of this rare but highly lethal disease.
Recent successful treatments
In recent years, a combination of factors, including early diagnosis, aggressive antimicrobial therapy, and intensive supportive care, has led to a few remarkable stories of survival. In 2013, two children in the United States, an 8-year-old boy and a 12-year-old girl, managed to survive PAM after being treated with a combination of drugs, including the anti-parasitic medication miltefosine. The 12-year-old girl also underwent therapeutic hypothermia, which may have played a role in her full neurological recovery. Another case of successful treatment was reported in 2016, where a 16-year-old boy from Florida survived after receiving a similar combination of drugs, including miltefosine.
RELATED: Top Toenail Fungus Treatments You Should Know About
Factors influencing survival
Several factors appear to influence the chances of survival in patients with PAM due to N. fowleri. Early recognition of the disease and prompt initiation of appropriate antimicrobial therapy are crucial, as the infection progresses rapidly and can cause extensive brain damage within a matter of days. The use of a combination of drugs, including amphotericin B, azithromycin, fluconazole, rifampin, and miltefosine, seems to improve outcomes compared to the use of single agents. Aggressive management of elevated intracranial pressure, using measures such as therapeutic hypothermia, may also contribute to better survival rates. However, the rarity of the disease and the lack of controlled clinical trials make it challenging to draw definitive conclusions about the most effective treatment strategies.
Conclusion
The Brain-Eating Amoeba remains a rare but deadly threat, with a significant impact on those affected. This article has shed light on the nature of Naegleria fowleri, its infection mechanism, early warning signs, and current treatment approaches. Understanding these aspects is key to raising awareness and potentially saving lives. The low survival rates and challenging treatment process highlight the need for ongoing research and improved diagnostic methods.
Looking ahead, there’s hope for better outcomes as medical knowledge grows and new therapies emerge. The recent successful treatments, though few, show that survival is possible with early detection and aggressive care. To move forward, it’s crucial to keep studying this organism, develop more effective treatments, and educate the public about prevention. By staying informed and vigilant, we can work to reduce the impact of this rare but serious infection.