Cholesteatoma is a rare but potentially serious condition that affects the middle ear. This abnormal growth of skin cells can lead to hearing loss, balance problems, and other complications if left untreated. Understanding the key symptoms, causes, and treatment methods of cholesteatoma is crucial for early detection and effective management of this condition.
This article aims to shed light on the nature of cholesteatoma, its telltale signs, and risk factors that may increase its likelihood. It will also explore various treatment approaches, including surgical options and follow-up care. By gaining insight into this condition, readers can better recognize its symptoms and seek timely medical attention, improving their chances of successful treatment and recovery.
What is a Cholesteatoma?
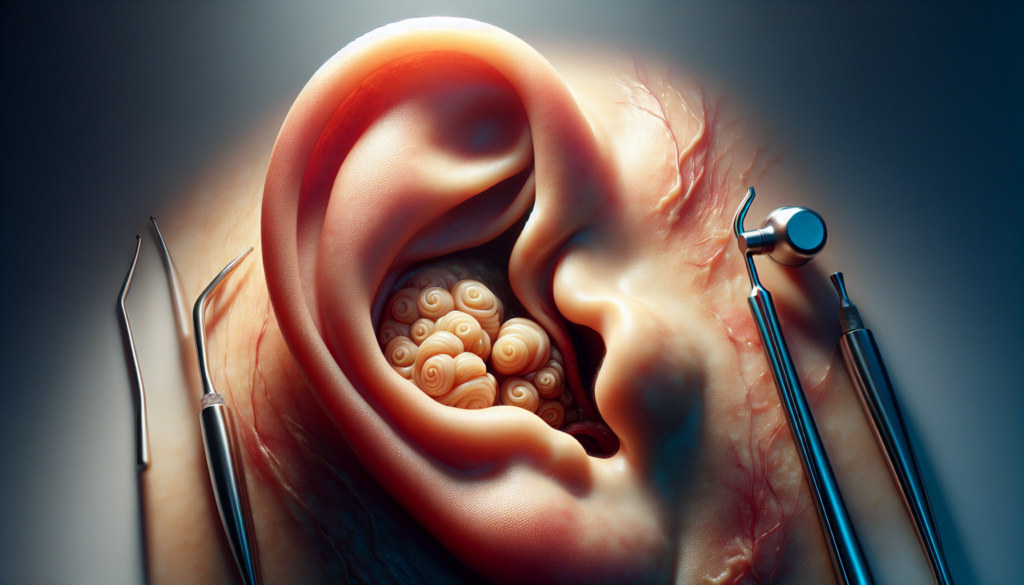
A cholesteatoma is an abnormal growth of skin-lined cyst that develops in the middle ear and mastoid bone behind the eardrum. It is not cancerous, but it can expand and cause destruction to the surrounding structures if left untreated. The classic definition of a congenital cholesteatoma is a cyst that develops behind an intact tympanic membrane in a child with no history of middle ear disease. However, since most children have some history of middle ear issues during infancy, cholesteatomas are considered congenital if they occur in children who have an intact eardrum and no history of ear surgery.
RELATED: Popcorn Lung (Bronchiolitis Obliterans): Symptoms and Treatment Explained
There are three main types of cholesteatomas: congenital, primary acquired, and secondary acquired. Congenital cholesteatomas form when skin cells become trapped in the middle ear before birth. Primary acquired cholesteatomas develop when the eustachian tube fails to drain properly or equalize pressure inside the ear, causing the eardrum to weaken and retract. This retraction pocket can accumulate skin cells and earwax, eventually forming a cholesteatoma. Secondary acquired cholesteatomas occur when skin cells pass through a ruptured eardrum and accumulate in the middle ear space.
The pathophysiology of cholesteatoma involves the abnormal accumulation of keratinized squamous epithelium within the middle ear and mastoid. This epithelium forms a matrix that is surrounded by inflammatory tissue known as the perimatrix. The cholesteatoma can progressively enlarge, surrounding and destroying the ossicles, which are the tiny bones responsible for transmitting sound vibrations from the eardrum to the inner ear. This bone erosion is thought to be caused by various enzymes and mediators released by the perimatrix.
Recognizing Cholesteatoma Symptoms
The symptoms of cholesteatoma can vary depending on the stage and severity of the condition. In the early stages, symptoms may be subtle or even absent, making it challenging to detect the presence of a cholesteatoma. As the growth progresses, however, it can lead to more noticeable signs and complications that require prompt medical attention.
Early Warning Signs
One of the earliest and most common symptoms of cholesteatoma is a persistent or recurring discharge from the affected ear. This discharge may have a foul odor and can be watery or thick in consistency. Individuals with cholesteatoma may also experience a feeling of fullness or pressure in the ear, as well as mild discomfort or pain. Gradual hearing loss in the affected ear is another potential early sign, particularly in cases of secondary acquired cholesteatoma.
RELATED: Understanding Placenta Previa: Symptoms, Causes, and Treatments
Advanced Symptoms
As a cholesteatoma grows larger, it can cause more severe symptoms and complications. Advanced signs may include significant hearing loss, vertigo or dizziness, and tinnitus (ringing in the ears). The growth may also lead to recurrent ear infections that do not respond well to conventional treatments. In some cases, individuals may experience numbness or pain in the ear or surrounding areas due to the pressure exerted by the expanding cholesteatoma.
Complications
If left untreated, a cholesteatoma can result in serious complications. The growth can erode the delicate bones of the middle ear, leading to permanent hearing loss. It may also damage the facial nerve, causing facial paralysis or weakness. In rare instances, the infection from a cholesteatoma can spread to the inner ear or brain, leading to life-threatening conditions such as meningitis or brain abscess. Recognizing the symptoms of cholesteatoma and seeking timely medical intervention is crucial to prevent these severe complications and preserve ear health.
Identifying Causes and Risk Factors
Several factors can contribute to the development of cholesteatoma, including genetic predisposition, anatomical abnormalities, and chronic middle ear infections. Understanding these causes and risk factors is crucial for early detection and prevention of this condition.
Eustachian Tube Dysfunction
Eustachian tube dysfunction is a significant risk factor for developing cholesteatoma. The Eustachian tube connects the middle ear to the back of the nose and helps regulate air pressure and drain fluid from the middle ear. When this tube fails to function properly, negative pressure can develop in the middle ear, causing the eardrum to retract and form a pocket. This pocket can accumulate skin cells and debris, eventually leading to cholesteatoma formation.
Chronic Ear Infections
Recurrent or chronic middle ear infections, such as otitis media, can also increase the risk of cholesteatoma. These infections can cause inflammation and damage to the eardrum, making it more susceptible to retraction and pocket formation. Additionally, chronic infections can lead to the accumulation of fluid and debris in the middle ear, providing an ideal environment for cholesteatoma growth.
Genetic Predisposition
While the exact role of genetics in cholesteatoma development is not fully understood, some evidence suggests that genetic factors may influence an individual’s susceptibility to this condition. Familial clustering of cholesteatoma has been reported in several case studies, with multiple family members affected across generations. This observation indicates that certain genetic variants or mutations may increase the risk of developing cholesteatoma, possibly by altering ear morphology or immune function. However, more research is needed to identify specific genes and understand their contribution to cholesteatoma pathogenesis.
Treatment Approaches for Cholesteatoma
The primary goal of cholesteatoma treatment is to remove the abnormal growth and prevent serious complications. The specific approach depends on factors such as the size and location of the cholesteatoma, the extent of damage to surrounding structures, and the patient’s overall health.
Medical Management
In some cases, small cholesteatomas may be managed with regular ear cleanings, medicated ear drops, and close monitoring. Antibiotics, either in the form of ear drops or oral medications, can be used to treat infections that often accompany cholesteatomas. However, medical management alone is rarely sufficient to cure the condition, and surgery is usually necessary to remove the growth completely.
RELATED: Pica: An In-Depth Guide to Causes, Symptoms, and Effective Treatments
Surgical Interventions
Surgery is the mainstay of cholesteatoma treatment. The type of surgery performed depends on the extent of the disease and the surgeon’s preferred technique. The two main surgical approaches are the canal wall–up (closed) and canal wall–down (open) mastoidectomy.
In a canal wall–up procedure, the surgeon removes the cholesteatoma while preserving the posterior wall of the ear canal and reconstructing the middle ear structures. This approach maintains the normal anatomy of the ear but carries a higher risk of cholesteatoma recurrence.
In a canal wall–down mastoidectomy, the posterior wall of the ear canal is removed along with the cholesteatoma, creating a large open cavity. This technique offers better exposure and a lower recurrence rate but requires regular cleaning and maintenance of the cavity.
In some cases, surgeons may employ a combination of these techniques or use endoscopic assistance to improve visualization and remove the cholesteatoma more effectively.
Follow-up Care
Regardless of the surgical approach used, close follow-up is crucial after cholesteatoma surgery. Patients require regular check-ups to monitor for any signs of recurrence, which can occur even years after the initial surgery. Imaging studies, such as MRI or CT scans, may be used to detect residual or recurrent disease.
In some cases, a second-look surgery may be necessary to ensure complete removal of the cholesteatoma and to reconstruct the middle ear if needed. Long-term follow-up care may also involve regular ear cleanings, hearing assessments, and management of any complications that arise.
Conclusion
To wrap up, cholesteatoma poses a significant threat to ear health, with the potential to cause hearing loss and other serious complications. Early detection and proper treatment are crucial to manage this condition effectively. Surgical intervention often plays a key role in removing the abnormal growth and preventing its recurrence, while follow-up care is essential to monitor for any signs of the disease returning.
Understanding the symptoms, causes, and treatment options for cholesteatoma empowers individuals to seek timely medical attention. By staying vigilant and working closely with healthcare providers, patients can improve their chances of successful treatment and recovery. This knowledge not only helps those affected by cholesteatoma but also raises awareness about the importance of ear health in general.