Colon polyps, also known as colonic polyps, are a common occurrence in the digestive tract that can potentially lead to serious health issues if left untreated. Understanding the causes, symptoms, and available treatment options for colon polyps is crucial for maintaining optimal digestive health and preventing the development of more severe conditions, such as colorectal cancer.
This comprehensive overview will delve into the different types of colon polyps, explore their causes and risk factors, and discuss the various symptoms that may indicate their presence. Additionally, the article will cover the diagnostic tests used to identify colon polyps and outline the treatment options available, depending on the type and severity of the polyps discovered.
What Are Colon Polyps?
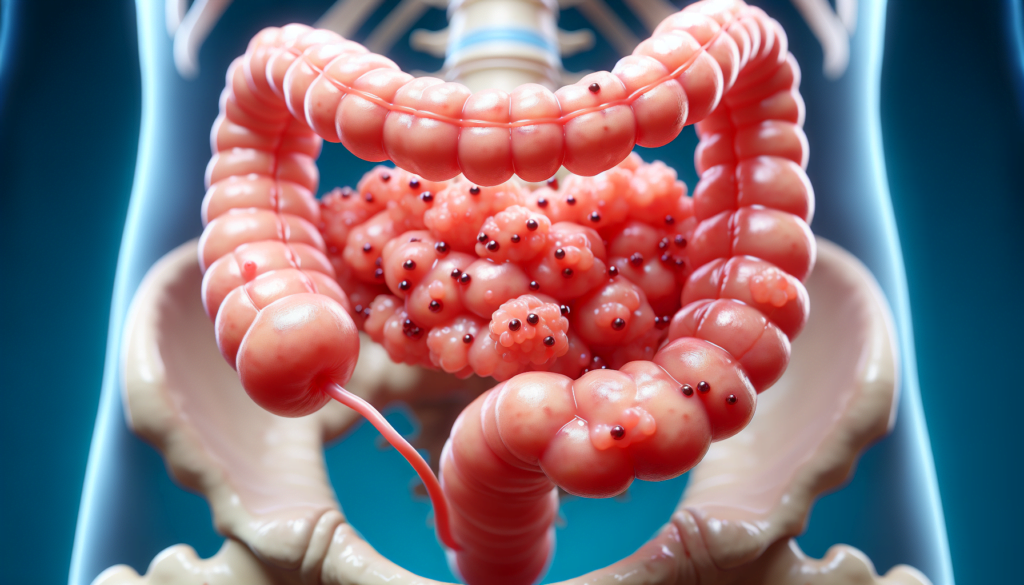
Colon polyps are small growths that develop on the lining of the colon or rectum. These growths are usually harmless, but some types of polyps can potentially turn into colorectal cancer if left untreated over time. Polyps can vary in size and shape, ranging from tiny bumps to larger, mushroom-like structures.
Most colon polyps do not cause any symptoms, and they are typically discovered during routine screening tests, such as a colonoscopy. Healthcare providers remove colon polyps when they are found to prevent the development of colorectal cancer.
Colon polyps are common in American adults, with an estimated 15 to 40 percent of adults having them. The likelihood of developing colon polyps increases with age, and they are more common in men than in women. Although most polyps are not cancerous, some may turn into cancer over time if not removed.
There are two main categories of colon polyps:
- Nonneoplastic polyps: These polyps typically do not become cancerous and include hyperplastic polyps and inflammatory polyps.
- Neoplastic polyps: These polyps have the potential to turn into cancer and include adenomas and serrated types. Adenomas are the most likely to become cancerous if given enough time to grow, while serrated polyps may also become cancerous depending on their size and location.
The risk of a polyp turning into cancer increases with its size. Regular screening and early detection through tests like colonoscopies can help prevent the growth and spread of cancerous polyps by allowing for their timely removal.
Causes and Risk Factors
Several factors can contribute to the development of colon polyps, including genetic predisposition and lifestyle factors. Understanding these causes and risk factors is crucial for preventing the formation of polyps and reducing the risk of colorectal cancer.
Genetic factors
Family history plays a significant role in the development of colon polyps and colorectal cancer. Individuals with a family history of adenomatous polyps or colorectal cancer are at higher risk of developing polyps themselves.
Certain genetic conditions, such as familial adenomatous polyposis (FAP) and Lynch syndrome (hereditary nonpolyposis colorectal cancer), greatly increase the likelihood of developing multiple polyps at a young age. These conditions are caused by inherited mutations in specific genes, such as APC in FAP and DNA mismatch repair genes (MLH1, MSH2, MSH6, PMS2) in Lynch syndrome.
Lifestyle factors
Age is a significant risk factor for colon polyps and colorectal cancer. Polyps become more common as individuals age, with the majority of cases occurring in individuals over 50. However, it’s essential to note that polyps can occur at any age, and younger individuals may also be at risk, particularly if there is a family history of the condition.
Poor dietary habits, including a high intake of red and processed meats, saturated fats, and low fiber, have been linked to an increased risk of colon polyps and colorectal cancer. Diets lacking in fruits, vegetables, and whole grains tend to contribute to chronic inflammation in the colon and promote the growth of polyps.
Other lifestyle factors that can elevate the risk of developing polyps and colorectal cancer include:
- Excessive alcohol consumption
- Smoking or using tobacco products
- Being overweight or obese
- Having type 2 diabetes mellitus
- Physical inactivity
Individuals with advanced forms of certain gastrointestinal conditions, such as Crohn’s disease or ulcerative colitis, are also at a higher risk of developing colon polyps.
By understanding these causes and risk factors, healthcare providers can identify individuals who may benefit from earlier and more frequent screening for colon polyps. Additionally, adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, can help reduce the risk of developing colon polyps and colorectal cancer.
Types of Colon Polyps
Colon polyps are classified into different types based on their histological characteristics and malignant potential. The two main categories of colon polyps are adenomatous polyps and serrated polyps.
Adenomatous polyps
Adenomatous polyps, also known as adenomas, are the most common type of colon polyp, accounting for approximately 70% of all polyps. They are considered precancerous lesions as they have the potential to develop into colorectal cancer over time. Adenomas are further classified based on their histological features:
- Tubular adenomas: These are the most common subtype, making up more than 80% of adenomatous polyps. They are characterized by the presence of tubular glands.
- Villous adenomas: These account for 5-15% of adenomas and have a higher risk of malignant transformation compared to tubular adenomas. They exhibit finger-like projections of epithelial cells.
- Tubulovillous adenomas: These polyps have a combination of tubular and villous features and comprise 5-15% of adenomas. Their malignant potential lies between that of tubular and villous adenomas.
The risk of an adenomatous polyp transforming into cancer increases with its size. Polyps larger than 1 cm in diameter have a higher likelihood of harboring high-grade dysplasia or becoming malignant.
Serrated polyps
Serrated polyps are characterized by a saw-tooth appearance of the crypt epithelium. They are further classified into three subtypes:
- Hyperplastic polyps: These are the most common type of serrated polyp, typically found in the distal colon. They have minimal malignant potential and are considered benign lesions.
- Sessile serrated lesions (SSLs): Previously known as sessile serrated adenomas or polyps, SSLs are flat or slightly elevated lesions commonly found in the proximal colon. They have the potential to develop into colorectal cancer through the serrated pathway.
- Traditional serrated adenomas (TSAs): TSAs are the least common subtype of serrated polyps, accounting for less than 1% of all colorectal polyps. They can have either sessile or pedunculated morphology and exhibit cytological dysplasia, indicating a higher risk of malignant transformation.
Hyperplastic polyps
Hyperplastic polyps are non-neoplastic lesions that result from an overgrowth of normal colonic mucosa. They are typically small (less than 5 mm) and found in the distal colon and rectum. Hyperplastic polyps have a very low malignant potential and are generally considered benign. However, some studies suggest that large hyperplastic polyps (>5 mm) located in the proximal colon may have a higher risk of developing into sessile serrated lesions or colorectal cancer.
Regular screening and removal of colon polyps through colonoscopy can significantly reduce the risk of developing colorectal cancer. The management and surveillance strategies for individuals with colon polyps depend on the type, size, number, and location of the polyps found during the examination.
Symptoms of Colon Polyps
Most people with colon polyps do not experience any symptoms. Polyps are usually discovered during routine screening tests or exams conducted for other digestive issues. However, in some cases, individuals may notice certain signs and symptoms that could indicate the presence of colon polyps:
- Rectal bleeding: This is the most common symptom associated with colon polyps. Blood may appear as red streaks in the stool or cause the stool to appear black. However, rectal bleeding can also be a sign of other conditions, such as hemorrhoids or minor tears in the anus.
- Change in bowel habits: Constipation or diarrhea that lasts longer than a week may suggest the presence of a larger colon polyp or cancer. It is important to note that several other conditions can also cause changes in bowel habits.
- Abdominal pain: Large colon polyps can partially block the bowel, leading to crampy abdominal pain or discomfort.
- Change in stool color: In addition to visible blood, polyps can cause slow, chronic bleeding that may lead to changes in stool color. Minor bleeding can result in red streaks, while heavier bleeding may make the stool appear black. However, certain foods, medicines, and dietary supplements can also alter the color of the stool.
- Iron deficiency anemia: Slow, chronic bleeding from polyps can lead to iron deficiency anemia over time. Symptoms of anemia include fatigue, weakness, pale skin, and shortness of breath.
It is crucial for individuals experiencing any of these symptoms to consult with their healthcare provider for proper evaluation and diagnosis. Regular screening is essential for the early detection and removal of colon polyps, especially in older adults and those with risk factors such as a family history of colon cancer or personal history of inflammatory bowel disease.
Diagnosis and Tests
Several diagnostic tests can help detect colon polyps and determine their size, location, and type. The most common methods include:
Colonoscopy
Colonoscopy is considered the gold standard for diagnosing colon polyps. During this procedure, a long, flexible tube with a camera on the end (colonoscope) is inserted into the rectum and guided through the entire colon. The camera allows the doctor to visualize the inside of the colon and identify any polyps or abnormalities.
If polyps are found during a colonoscopy, the doctor can remove them using special tools passed through the colonoscope. The removed polyps are then sent to a laboratory for histological analysis to determine if they are benign, pre-cancerous, or cancerous.
Stool tests
Stool tests can be used as a non-invasive screening method for colon polyps and colorectal cancer. These tests look for hidden blood (occult blood) or specific genetic markers in the stool that may indicate the presence of polyps or cancer. The two main types of stool tests are:
- Fecal occult blood test (FOBT): This test detects blood in the stool, which can be a sign of polyps or colorectal cancer. However, blood in the stool can also be caused by other conditions, such as hemorrhoids or ulcers.
- Fecal immunochemical test (FIT): This test is more specific than the FOBT, as it detects human hemoglobin in the stool. FIT is less likely to produce false-positive results due to dietary factors or medications.
If a stool test comes back positive, a colonoscopy is typically recommended to confirm the presence of polyps or cancer and remove any polyps found.
Imaging tests
In some cases, imaging tests may be used to visualize the colon and detect polyps. These tests include:
- CT colonography (virtual colonoscopy): This test uses a CT scanner to create detailed images of the colon. A computer then assembles these images into a 3D view of the colon, allowing the doctor to identify any polyps or abnormalities. If polyps are found, a traditional colonoscopy may be needed to remove them.
- Barium enema: This test involves injecting a liquid containing barium into the rectum, which coats the lining of the colon. X-rays are then taken to visualize the colon and detect any polyps or abnormalities. However, this test is less sensitive than colonoscopy and is rarely used today.
In summary, colonoscopy remains the most accurate and effective method for diagnosing and removing colon polyps. Stool tests and imaging tests can be used as non-invasive screening tools, but positive results typically require a follow-up colonoscopy for confirmation and treatment.
Treatment Options for Colon Polyps
The primary treatment for colon polyps is removal during a colonoscopy, a procedure known as a polypectomy. In most cases, the polyp can be completely removed during the colonoscopy itself, using special tools passed through the colonoscope. After removal, the polyp tissue is sent to a laboratory for analysis to determine if it contains cancerous or precancerous cells.
Polypectomy
There are several techniques used for polypectomy, depending on the size, location, and type of polyp:
- Cold forceps polypectomy: This method is used for small polyps, typically less than 5 mm in size. The polyp is grasped with forceps and twisted off the colon wall.
- Hot forceps polypectomy: For slightly larger polyps, electrocautery (heat) is applied to the forceps to cauterize the polyp base and prevent bleeding.
- Snare polypectomy: Larger polyps are removed using a wire loop called a snare. The snare is placed around the polyp base and tightened, while electrocautery is applied to cut the polyp off and seal the base.
- Endoscopic mucosal resection (EMR): This technique is used for larger, flat polyps. A solution is injected under the polyp to lift it, and then a snare is used to remove the polyp.
Surgery (if needed)
In rare cases, if a polyp is too large or difficult to remove during a colonoscopy, surgery may be necessary. Surgical options include:
- Laparoscopic surgery: Small incisions are made in the abdomen, and the polyp is removed using specialized instruments.
- Open surgery: A larger incision is made in the abdomen to remove the polyp and surrounding tissue if there is a concern for cancer.
After polypectomy, patients are advised to follow up with their healthcare provider for regular surveillance colonoscopies to monitor for the development of new polyps or signs of colorectal cancer. The frequency of these follow-up exams depends on factors such as the number, size, and type of polyps removed, as well as the individual’s overall risk for colorectal cancer.
Conclusion
Colon polyps are a common occurrence in the digestive tract, and while most are benign, some types have the potential to develop into colorectal cancer if left untreated. Understanding the causes, risk factors, and symptoms associated with colon polyps is crucial for early detection and prevention. Regular screening through colonoscopy remains the most effective method for identifying and removing polyps, significantly reducing the risk of colorectal cancer.
By adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, individuals can lower their risk of developing colon polyps. Those experiencing symptoms or with a family history of colorectal cancer should consult their healthcare provider to determine the most appropriate screening schedule. With proper awareness, prevention, and treatment, the impact of colon polyps on overall health can be significantly minimized.