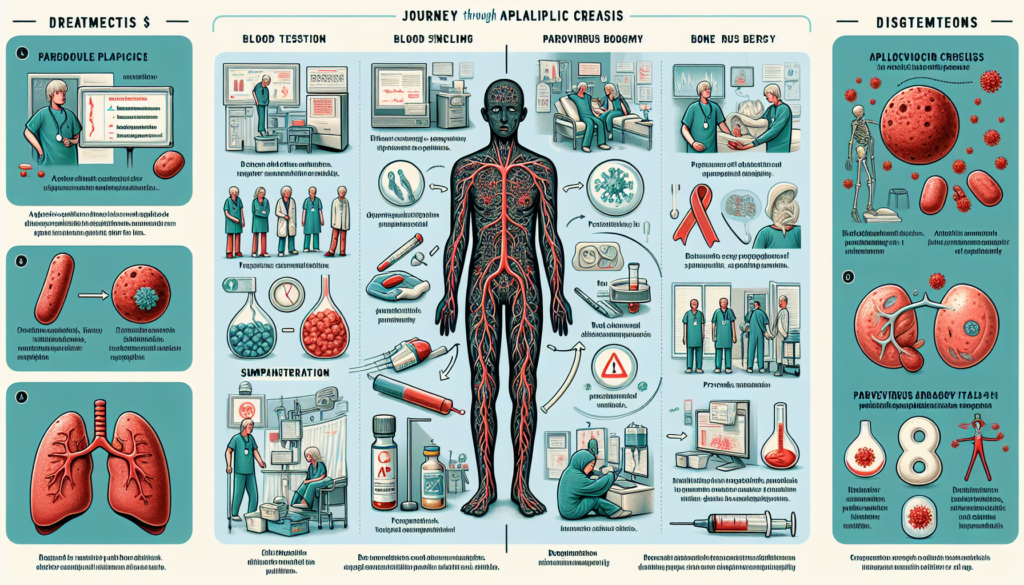
Understanding aplastic crisis and its management is critical for patients and healthcare providers alike, particularly when it intersects conditions like sickle cell disease. Aplastic crisis represents a severe, albeit usually transient, failure of the bone marrow to produce red blood cells, leading to significant health challenges. This condition, often distinguished from aplastic anemia by its temporary nature, demands prompt recognition and management to prevent serious complications. The significance of addressing aplastic crisis lies not only in mitigating immediate health risks but also in safeguarding against potential long-term impacts on patient health.
This guide delves into the essential aspects of aplastic crisis, including its causes—ranging from infections like parvovirus to underlying genetic conditions such as sickle cell disease. Readers will explore the hallmark symptoms that signal an aplastic crisis, the diagnostic journey to accurately identify this condition, and the effective treatment options currently available. Further, the article will cover preventive measures and provide an outlook for those affected by aplastic crisis, aiming to offer comprehensive insights into managing this medical challenge efficiently.
What is Aplastic Crisis?
An aplastic crisis is a medical condition characterized by a sudden and severe reduction in the production of red blood cells by the bone marrow. This abrupt halt in red blood cell production leads to severe anemia, which can be life-threatening if not promptly addressed. Aplastic crises are particularly prevalent among individuals with underlying blood disorders such as sickle cell anemia.
The primary trigger for an aplastic crisis is often an infection by parvovirus B19, commonly known as the virus responsible for the childhood illness fifth disease. This virus specifically targets the bone marrow, temporarily shutting down its ability to produce red blood cells. While parvovirus B19 is a widespread virus, an aplastic crisis typically occurs only in individuals with specific blood disorders who are also infected with this virus.
Aplastic crises are more commonly observed in children than in adults due to the higher prevalence of parvovirus B19 infections among younger populations. However, any individual with a predisposition to conditions that destroy red blood cells or cause hemolytic anemia is at an increased risk of experiencing an aplastic crisis if they contract the parvovirus B19 infection.
It is crucial to differentiate an aplastic crisis from the chronic anemia seen in conditions like sickle cell disease. Unlike chronic anemia, which is a constant feature of such diseases, an aplastic crisis represents a temporary yet severe cessation of red blood cell production. This distinction is vital for accurate diagnosis and appropriate management of the condition.
In summary, an aplastic crisis is a critical condition marked by a sudden stop in the production of red blood cells, leading to severe anemia. It is most commonly triggered by parvovirus B19 and poses a significant risk to individuals with certain blood disorders. Prompt recognition and treatment are essential to prevent serious health complications.
Causes of Aplastic Crisis
Parvovirus B19 Infection
A significant cause of aplastic crisis is the infection by Parvovirus B19, a common viral agent known for its impact on individuals with pre-existing blood disorders. This virus specifically targets the bone marrow’s ability to produce red blood cells by attacking and destroying immature red blood cells. The disruption caused by Parvovirus B19 is particularly detrimental in individuals who rely on a steady production of these cells due to underlying hematologic conditions. Infection with this virus can lead to severe anemia as the bone marrow fails to compensate for the loss of red blood cells.
Blood Disorders Associated with Aplastic Crisis
Individuals with certain blood disorders are at an increased risk of developing an aplastic crisis, particularly when infected with Parvovirus B19. These conditions include:
- Sickle Cell Anemia and Similar Disorders: These are genetic disorders that affect the shape and function of red blood cells. An aplastic crisis in these patients can lead to severe complications due to the already compromised state of the red blood cells.
- Hereditary Spherocytosis: This condition involves a defect in the red blood cell membrane, making them more prone to destruction.
- Hemoglobin C Disease: Another genetic disorder affecting hemoglobin, the protein in red blood cells that carries oxygen.
- Thalassemia: A group of inherited blood disorders characterized by abnormal formation of hemoglobin.
- G6PD Deficiency: A metabolic disorder that can lead to hemolytic anemia under certain conditions such as infection or exposure to certain medications.
- Pyruvate Kinase Deficiency: This condition affects the enzyme which is crucial for energy production in red blood cells.
- Autoimmune Hemolytic Anemia: Where the immune system mistakenly destroys red blood cells.
- Paroxysmal Nocturnal Hemoglobinuria: A rare, life-threatening disease that leads to the destruction of red blood cells.
- Hereditary Elliptocytosis: Another genetic condition leading to abnormally shaped red blood cells that are prone to breakdown.
These disorders exacerbate the risk of an aplastic crisis as they inherently affect the lifespan and function of red blood cells. When coupled with a Parvovirus B19 infection, the impact on the bone marrow’s ability to produce new red blood cells can lead to a critical reduction in these cells, manifesting as an aplastic crisis.
Symptoms of Aplastic Crisis
Common Symptoms
Individuals experiencing an aplastic crisis typically exhibit symptoms associated with severe anemia. These symptoms are primarily due to the body’s inability to produce an adequate amount of red blood cells, which are crucial for carrying oxygen throughout the body. Common symptoms include:
- Fatigue: Individuals often experience extreme tiredness that is not relieved by rest.
- Dizziness: A lack of red blood cells can lead to decreased oxygen in the brain, causing dizziness.
- Shortness of Breath (Dyspnea): With fewer red blood cells to transport oxygen, shortness of breath can occur even during mild activities.
- Irregular or Rapid Heartbeat: The heart may pump faster and harder to compensate for the lack of oxygen in the blood.
- Fever: A temperature of 101 degrees Fahrenheit (38 degrees Celsius) or higher can be a sign of an underlying infection or the body’s response to severe anemia.
- Pallor: Noticeable paleness of the skin, lips, gums, or fingernails indicates reduced blood flow and oxygenation.
Severity in Different Age Groups
The severity of symptoms can vary significantly among different age groups:
- Babies and Young Children: In younger patients, symptoms of aplastic crisis can manifest as increased fussiness or irritability. The limited ability of infants and young children to communicate their discomfort makes it particularly important for caregivers to note any changes in behavior or appearance that may indicate severe anemia.
- Adults: While adults may better articulate their symptoms, the impact of aplastic crisis can be equally severe, potentially disrupting daily activities and requiring immediate medical attention.
In all cases, the onset of these symptoms requires prompt evaluation and management to prevent further complications and to address the underlying causes effectively.
Diagnosis of Aplastic Crisis
Blood Tests
Blood tests are fundamental in diagnosing aplastic crisis. These tests typically reveal pancytopenia, which is a reduction in the number of red blood cells, white blood cells, and platelets. A complete blood count (CBC) is often the initial test used to detect these abnormalities. It measures various components such as hematocrit, hemoglobin levels, and the number and types of blood cells. Additional blood tests may check for unusual amounts of folate, vitamin B12, and erythropoietin, which is a hormone essential for the production of red blood cells.
Bone Marrow Biopsy
A bone marrow biopsy is a critical diagnostic tool for aplastic crisis. This procedure involves extracting a small sample of bone marrow tissue using a needle, typically from a large bone like the hipbone. The sample is then examined under a microscope to assess the cellularity of the marrow and the presence of blood-forming cells. In cases of aplastic crisis, the bone marrow is usually markedly hypocellular, meaning it has fewer cells than normal, particularly those involved in blood cell formation. This test helps distinguish aplastic crisis from other blood-related diseases.
Parvovirus B19 Test
Testing for Parvovirus B19 is essential in the diagnosis of aplastic crisis, especially when the patient has a history of exposure to the virus or presents with symptoms indicative of a recent infection. The presence of Parvovirus B19 can be confirmed through serological analysis using ELISA (Enzyme-Linked Immunosorbent Assay) to detect specific antibodies, or through polymerase chain reaction (PCR) assays that identify the viral DNA. Positive results for Parvovirus B19 IgM antibodies or DNA confirm an acute infection, which is a crucial step in diagnosing aplastic crisis triggered by this virus.
Treatment Options
Blood Transfusions
Blood transfusions are a fundamental component of managing aplastic crisis. They do not cure the condition but are crucial for controlling bleeding and alleviating symptoms by providing the red blood cells and platelets that the bone marrow fails to produce. Patients might receive red blood cells to help relieve anemia and fatigue, and platelets to prevent excessive bleeding. While there is generally no limit to the number of blood transfusions one can have, repeated transfusions can lead to complications such as iron overload. This condition, known as hemochromatosis, occurs when iron from transfused red blood cells accumulates in the body, potentially damaging organs. Treatments are available to remove excess iron, thereby mitigating this risk.
Intravenous Immunoglobulin (IVIG)
Intravenous Immunoglobulin (IVIG) is another treatment used in managing aplastic crisis, particularly when the cause is linked to immune system activity. IVIG is administered through an intravenous tube, supplying antibodies that can alter the immune response. This treatment is often necessary when the body’s immune system is attacking its own blood cells, a common scenario in autoimmune-related aplastic anemia. Most patients show signs of recovery within 10 to 14 days of starting IVIG treatment.
Medications
Medications play a pivotal role in the treatment of aplastic crisis, especially when the condition is associated with an autoimmune disorder or when a patient cannot undergo a bone marrow transplant. Immunosuppressants such as anti-thymocyte globulin are used to suppress the immune cells that damage the bone marrow, aiding in its recovery and the production of new blood cells. These are often used in conjunction with corticosteroids to enhance their effectiveness.
Additionally, medicines called growth factors, such as erythropoietin and granulocyte colony-stimulating factor, are used to stimulate the bone marrow to produce more blood cells. Hypomethylating agents may be prescribed to prevent the growth of abnormal bone marrow stem cells and increase the number of healthy blood cells, improving the patient’s quality of life and reducing the risk of developing leukemia.
Antibiotics are also commonly used to combat infections, a frequent complication in patients with aplastic crisis due to their reduced white blood cell count. This approach helps manage the increased risk of bacterial infections that these patients face.
Prevention and Outlook
Risk Reduction Strategies
Preventing aplastic crisis, particularly in individuals with predisposing blood disorders, is challenging due to the ubiquitous nature of its common trigger, parvovirus B19. Currently, there is no vaccine available to prevent infection from this virus. However, healthcare providers recommend several precautionary measures for individuals with conditions like sickle cell anemia to minimize their risk of infection. These measures include frequent handwashing, avoiding close contact with individuals who are ill, and adhering to general hygiene practices to reduce the likelihood of contracting viral infections.
For those diagnosed with aplastic anemia, managing risks involves careful monitoring and proactive treatment of any underlying conditions or factors that could precipitate the disease. This includes avoiding medications known to suppress bone marrow function and being vigilant about any signs of infection or unusual bleeding, as these could indicate a worsening of the condition.
Prognosis After Treatment
The prognosis for individuals experiencing an aplastic crisis varies based on several factors, including the severity of the condition, the presence of underlying blood disorders, and the individual’s overall health. Most patients recover within 10 to 14 days after initiating appropriate treatment, which may include blood transfusions and medications to stimulate bone marrow function.
However, some individuals may experience recurrent episodes of aplastic crisis, especially if they have chronic underlying conditions such as sickle cell disease. In such cases, long-term management strategies are essential to minimize the frequency and severity of crises.
For aplastic anemia, treatment outcomes can significantly improve with interventions like allogeneic stem cell transplantation, particularly in younger patients and those under 40 years of age. Survival rates following such treatments are generally high, with studies indicating a survival rate of 96% post-transplant and even higher rates in younger demographics.
It is crucial for patients and their caregivers to maintain regular communication with healthcare providers to monitor the condition effectively and adjust treatment plans as needed. This ongoing management is vital to address any complications promptly and to enhance the quality of life for those affected by aplastic crisis and aplastic anemia.
Conclusion
Through the detailed exploration of aplastic crisis, its symptoms, causes, diagnostic pathways, and treatment options, we’ve underscored the complexity and the critical nature of managing this condition. A profound understanding of how aplastic crisis interplays with underlying blood disorders, particularly with triggers like Parvovirus B19, equips both patients and healthcare providers with the knowledge to anticipate and mitigate the adverse effects of this condition. The crucial role of prompt, accurate diagnosis and the implementation of effective treatment strategies cannot be overstated, as they form the linchpin in preventing severe outcomes and ensuring a positive prognosis for those afflicted.
Looking forward, the continuous advancement in medical research and treatment methodologies holds promise for improving the management of aplastic crisis and related blood disorders. While the journey from symptom onset to recovery can be fraught with challenges, the prospects for those facing an aplastic crisis are ever-improving thanks to these advancements. Encouraging further research and maintaining a proactive approach to health management remain paramount. Patients, caregivers, and medical professionals must work in concert to navigate this complex medical landscape, ensuring that those affected by an aplastic crisis can achieve the best possible health outcomes with the quality of life they deserve.