Diverticulosis is a common digestive condition that affects millions of people worldwide, particularly those over the age of 50. This condition occurs when small, bulging pouches form in the lining of the digestive tract, most often in the colon. While many individuals with diverticulosis experience no symptoms, it can lead to complications and discomfort for others, making it crucial to understand its nature and impact on overall health.
This article delves into the various aspects of diverticulosis, shedding light on its symptoms, causes, and available treatments. We’ll explore the risk factors that contribute to its development, discuss how doctors diagnose the condition, and examine the range of treatment options available to manage symptoms and prevent complications. By the end of this piece, readers will have a comprehensive understanding of diverticulosis and be better equipped to recognize its signs and seek appropriate care.
What is Diverticulosis?
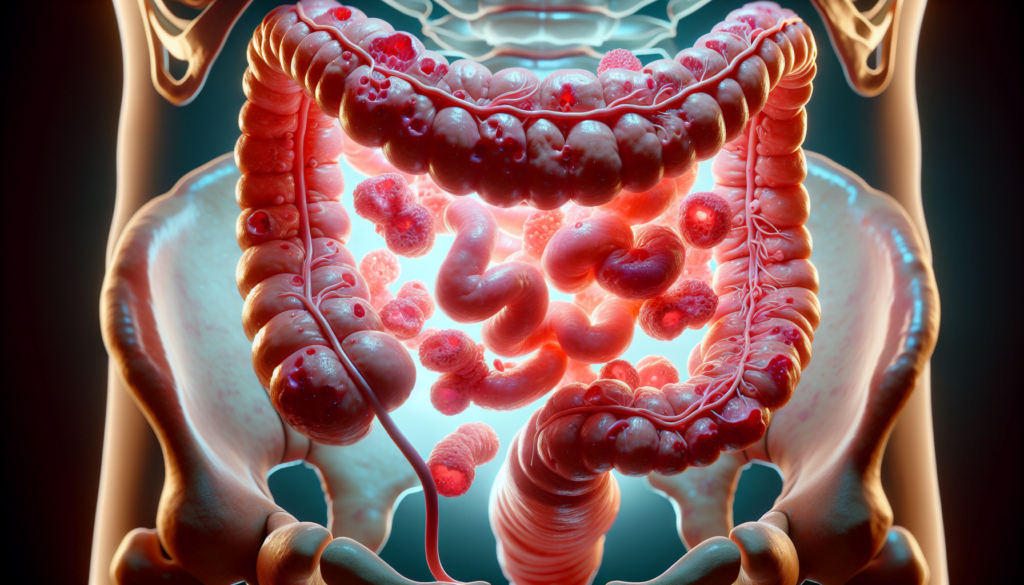
Diverticulosis is a condition in which small, bulging pouches called diverticula develop in the digestive tract, particularly in the colon. These pouches form at weak spots in the intestinal wall, typically in the lower part of the colon known as the sigmoid colon. Diverticulosis is quite common, especially as people age, with more than 30% of U.S. adults between 50 and 59 and over 70% of those older than 80 having the condition.
Definition
Diverticulosis describes the presence of diverticula in the colon. Most people with diverticulosis do not experience any symptoms or problems. The term “diverticular disease” is used when diverticulosis leads to chronic symptoms, diverticular bleeding, diverticulitis, or its complications.
RELATED: Bartholin Cyst Explained: Symptoms, Causes, and Treatment Methods
Diverticula formation
Diverticula form gradually over time when the inner lining of the intestines pushes through weak spots in the outer wall. This usually happens due to pressure in the colon, possibly from spasms or straining during bowel movements. Factors such as a low-fiber diet, lack of exercise, and certain medications may contribute to the development of diverticulosis.
Difference from diverticulitis
While diverticulosis refers to the presence of diverticula, diverticulitis occurs when one or more of these pouches become inflamed or infected. Diverticulitis can cause sudden, severe abdominal symptoms and may lead to serious complications if left untreated. Less than 5% of people with diverticulosis develop diverticulitis.
In summary, diverticulosis is a common condition characterized by the formation of small pouches in the colon wall. It is important to distinguish between diverticulosis and diverticulitis, as the latter involves inflammation or infection of the diverticula and requires prompt medical attention.
Symptoms of Diverticulosis
Most people with diverticulosis do not experience any symptoms, as the condition itself is not dangerous. In these asymptomatic cases, diverticulosis is usually discovered during examinations for other conditions, such as colorectal cancer.
However, some individuals with diverticulosis may experience a range of symptoms, including:
- Abdominal pain and bloating
- Constipation and diarrhea
- Flatulence
- Minor blood in the feces, which can sometimes be more severe if a diverticulum becomes inflamed or is near a blood vessel
- Anemia resulting from repeated bleeding
It is important to note that many of these symptoms are similar to those of bowel cancer. While diverticulosis is more common, it is crucial to have these symptoms assessed by a specialist to rule out more serious conditions.
If you experience any of the following symptoms, seek medical attention promptly:
- Persistent abdominal pain or cramping
- Alterations in bowel habits
- Blood in the stool
Your healthcare provider will conduct a thorough evaluation to determine the cause of your symptoms and provide appropriate treatment. They may recommend tests such as a colonoscopy, barium enema, or CT scan to confirm the diagnosis of diverticular disease and rule out other potential causes.
Remember, while diverticulosis is usually asymptomatic, it is essential to be aware of the potential symptoms and complications associated with the condition. By maintaining a healthy lifestyle, including a high-fiber diet and regular exercise, you can help prevent the development of diverticulitis and its associated complications.
Causes and Risk Factors
The exact causes of diverticulosis are not fully understood, but several risk factors have been identified that may contribute to the development of this condition. These include age-related changes, dietary influences, and genetic predisposition.
Age-related factors
Diverticulosis is more common in older individuals, with the prevalence increasing significantly after the age of 50. As people age, the colon wall may become weaker and more susceptible to the formation of diverticula. This age-related risk factor is thought to be due to changes in the structure and function of the colon over time.
Dietary influences
Diet plays a significant role in the development of diverticulosis. A low-fiber diet, which is common in Western countries, is associated with an increased risk of developing diverticula. Fiber helps to bulk up the stool and promotes regular bowel movements, reducing the pressure within the colon. Conversely, a diet high in red meat and low in fiber may increase the risk of diverticulosis.
RELATED: Balanitis Symptoms and Treatments: What You Need to Know
Genetic predisposition
Recent studies suggest that genetics may also play a role in the development of diverticulosis. Twin studies have estimated that 40-53% of an individual’s risk for diverticular disease may be attributed to genetic factors. Genome-wide association studies (GWAS) have identified several genetic variants associated with an increased risk of diverticular disease, although more research is needed to fully understand the specific genes involved and their mechanisms of action.
Other potential risk factors for diverticulosis include obesity, lack of physical activity, and certain medications that may alter bowel motility. The interplay between these various risk factors likely contributes to the development of diverticula in the colon. Understanding these risk factors can help guide preventive strategies and lifestyle modifications to reduce the risk of diverticulosis and its potential complications.
Diagnosis and Treatment Options
Diagnosing diverticulosis involves a thorough evaluation by a gastroenterologist. The process begins with a physical exam, during which the doctor gently touches different parts of the abdomen to identify pain or tenderness. They may also perform a pelvic exam to rule out diseases of the female reproductive organs.
Several diagnostic tests can help confirm the presence of diverticulosis and rule out other conditions:
- Blood tests to check for signs of infection and immune-system activity
- Urine test
- Stool test
- Pregnancy test
- Liver enzyme test to rule out liver disease
- Computerized tomography (CT) scan to show inflamed diverticula, abscesses, fistulas, or other complications
A colonoscopy is the most precise tool for diagnosing diverticular disease. It allows the gastroenterologist to examine the lining of the colon and rectum wall for any problems, including diverticula, inflammation, or bleeding.
Once diverticulosis has been diagnosed, treatment depends on the severity of the condition. For mild cases, conservative management is often sufficient. This includes bowel rest, antibiotics, and a liquid or low-residue diet to decrease bulk and stool in the intestines, reducing irritation and promoting healing.
In more severe cases, such as when a perforation or abscess is suspected, hospitalization may be necessary for further treatment and monitoring. During hospitalization, diagnostic tests like CT scans and colonoscopies are performed to examine the colon and determine the best course of action.
If diverticular bleeding occurs, colonoscopy can help identify the source and stop the bleeding using techniques like epinephrine injection, bipolar cautery, or endoclips. Angiography is another option for controlling bleeding, either through the injection of selective embolization of bleeding vessels.
RELATED: Blepharitis: Exploring the Best Treatment Methods and Preventive Measures
When conservative measures fail, or in cases of severe complications, surgical interventions may be necessary. NYU Langone gastrointestinal surgeons may perform minimally invasive or conventional open surgery to remove the diseased portion of the colon. In emergency situations, a procedure called Hartmann’s procedure may be performed, which involves removing the affected colon segment and creating a temporary stoma.
Elective surgery, such as a sigmoidectomy, may be recommended for patients who have had multiple episodes of diverticulitis to prevent recurrence. This minimally invasive procedure involves removing the affected part of the colon, called the sigmoid colon.
Conclusion
Diverticulosis is a common digestive condition that has a significant impact on many people, especially as they age. This article has shed light on its symptoms, causes, and available treatments, giving readers a better understanding of this often-overlooked health issue. By exploring the risk factors and diagnostic methods, we’ve highlighted the importance of early detection and proper management to prevent complications.
To wrap up, knowing about diverticulosis is key to maintaining good digestive health. While it’s often symptomless, being aware of potential warning signs and risk factors can help people take steps to prevent its development or manage existing cases. With the right approach, including dietary changes and medical care when needed, most people with diverticulosis can lead normal, healthy lives.