Dysentery is a devastating intestinal infection that affects millions of people worldwide. This potentially life-threatening condition causes severe diarrhea, often accompanied by blood and mucus in the stool. Understanding what dysentery is, its symptoms, and available treatments is crucial for early detection and effective management of the disease.
This article delves into the causes and risk factors associated with dysentery, helping readers recognize its symptoms and potential complications. It explores the journey from diagnosis to treatment, offering insights into various management strategies. Additionally, the article discusses prevention methods and provides a long-term outlook for those affected by this serious illness, equipping readers with valuable knowledge to protect themselves and their loved ones.
Dysentery Unveiled: Causes and Risk Factors
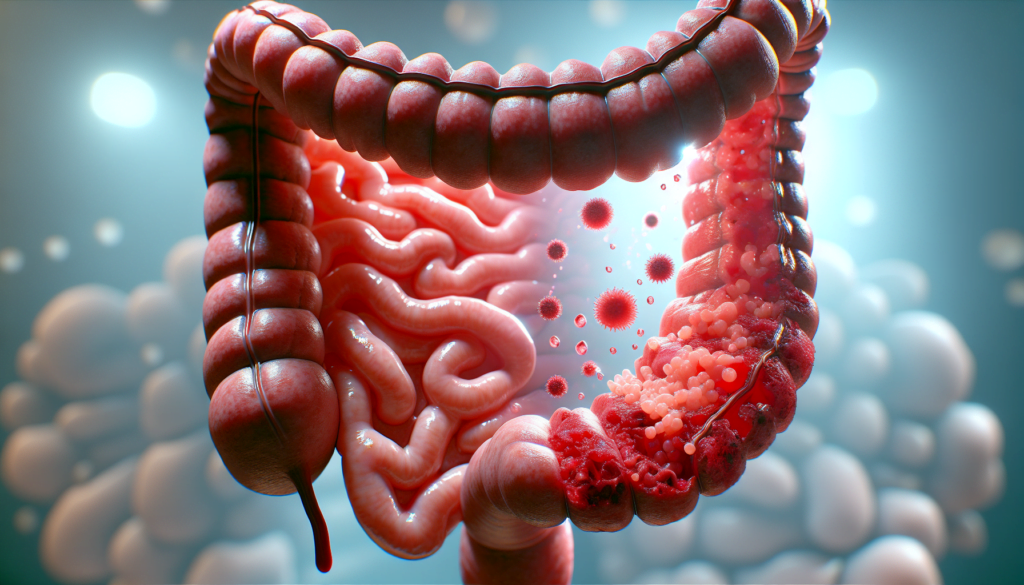
Dysentery is an intestinal infection caused by bacteria or parasites, resulting in severe diarrhea, often accompanied by blood and mucus in the stool. Understanding the causes and risk factors associated with dysentery is crucial for early detection and effective management of the disease.
Bacterial Causes
Bacillary dysentery, the most common type of dysentery, is caused by bacteria called Shigella. This infection, also known as shigellosis, affects approximately 500,000 people in the United States annually. Shigella bacteria are highly contagious, with as few as 10 organisms capable of causing infection. Transmission occurs through the fecal-oral route, either directly from person-to-person contact or indirectly through contaminated food, water, or fomites.
Parasitic Causes
Amoebic dysentery, another form of the disease, is caused by a parasite called Entamoeba histolytica. This type of dysentery is more prevalent in tropical locations with poor sanitation. Infection occurs when a person ingests food or water contaminated with the parasite or comes into contact with contaminated surfaces, such as toilet handles or sink knobs. Swimming in contaminated water, such as lakes or pools, can also lead to infection.
RELATED: Hyperlipidemia: Key Symptoms and How to Treat Them
High-Risk Populations
Certain populations are at a higher risk of contracting dysentery:
- International travelers visiting areas with poor sanitation
- Children, particularly those in daycare settings
- People with compromised immune systems
- Men who have sex with men (MSM)
- People experiencing homelessness
Shigella infections are also more common in low- and middle-income countries, with S. flexneri being the predominant species. In high-income countries, S. sonnei is the primary cause of shigellosis.
By understanding the causes and risk factors associated with dysentery, healthcare providers and public health officials can develop targeted prevention strategies and provide timely treatment to those affected by this potentially life-threatening condition.
Recognizing Dysentery: Symptoms and Complications
Dysentery symptoms can vary depending on the type of infection, but they typically involve severe diarrhea, often accompanied by blood and mucus in the stool. Recognizing the early signs and severe symptoms of dysentery is crucial for prompt treatment and preventing potential complications.
Early Signs
In the initial stages of dysentery, individuals may experience:
- Diarrhea with abdominal cramps
- Nausea and vomiting
- Fever
- Weight loss
Bacillary dysentery, caused by Shigella bacteria, usually presents with diarrhea and abdominal cramps within 1-3 days of infection. Amoebic dysentery, caused by the parasite Entamoeba histolytica, may not cause symptoms initially, but when they do appear, it’s typically 2-4 weeks after infection.
Severe Symptoms
As the infection progresses, more severe symptoms may develop:
- Bloody or mucus-filled stools
- Severe abdominal pain
- High fever
- Dehydration due to excessive fluid loss
In rare cases of amoebic dysentery, the infection can spread to the liver, causing a liver abscess. Symptoms of a liver abscess include:
- Nausea and vomiting
- High fever
- Pain in the upper right abdomen
- Swollen liver
RELATED: Top Home Remedies and Treatments for Gingivitis
Potential Complications
If left untreated, dysentery can lead to serious complications:
- Severe dehydration: The most common complication, which can cause life-threatening electrolyte imbalances and organ damage.
- Hemolytic uremic syndrome (HUS): A type of kidney damage that can occur in severe cases of bacillary dysentery.
- Toxic megacolon: A rare complication characterized by severe inflammation and dilation of the colon.
- Rectal prolapse: A condition in which the rectum protrudes through the anus due to repeated straining during bowel movements.
Recognizing the symptoms of dysentery and seeking prompt medical attention is essential for effective treatment and preventing these potentially life-threatening complications. If you experience severe diarrhea, abdominal cramps, or other concerning symptoms, especially after traveling to areas with poor sanitation, consult your healthcare provider immediately.
Dysentery Management: From Diagnosis to Treatment
Dysentery management involves a comprehensive approach that includes accurate diagnosis and effective treatment strategies. Healthcare professionals rely on various diagnostic techniques to identify the underlying cause of dysentery and develop a tailored treatment plan.
To diagnose dysentery, your healthcare provider will ask about your symptoms, conduct a physical exam, and order tests. The most common diagnostic test is a stool culture, where a sample of your stool is analyzed for the presence of bacteria, parasites, or ova. In some cases, a sigmoidoscopy may be recommended to examine the inside of your lower colon and rectum.
Once the cause of dysentery is determined, treatment can begin. Antibiotics may also be prescribed, along with over-the-counter medications to manage nausea and other symptoms.
Bacillary dysentery often resolves on its own within a week, but in some cases, antibiotics and IV fluids may be necessary. Rarely, a blood transfusion might be required.
In addition to medical treatment, home care plays a crucial role in managing dysentery symptoms and preventing complications. It’s essential to:
- Stay hydrated by drinking plenty of fluids, such as water, broths, and juices.
- Avoid caffeine and alcohol, which can worsen dehydration.
- Gradually reintroduce semisolid and low-fiber foods as your stool returns to normal.
- Avoid dairy products, fatty foods, high-fiber foods, or highly seasoned foods for a few days.
Over-the-counter antidiarrheal medicines, such as loperamide and bismuth subsalicylate, may help reduce the frequency of watery stools and control severe symptoms. However, it’s important to consult your healthcare provider before taking these medications, as they may not be suitable for everyone.
By combining accurate diagnosis, appropriate medical treatment, and effective home care strategies, most people with dysentery can expect to recover within a couple of weeks and return to their normal activities.
Beyond Treatment: Prevention and Long-Term Outlook
Preventing dysentery involves practicing good hygiene habits and taking precautions when traveling to areas with poor sanitation. Thorough hand washing with soap and running water after using the bathroom and before handling food is crucial. Avoiding sharing personal items like toothbrushes, drinking glasses, and towels can also help prevent the spread of infection.
When traveling, it’s essential to:
- Drink only bottled or chlorine-treated water
- Avoid ice cubes, fountain drinks, and unpasteurized dairy products
- Wash all fruits and vegetables with clean running water and peel them before eating
- Thoroughly cook all food
If you have dysentery, stay away from others, avoid sexual contact, and don’t prepare food for anyone else to prevent spreading the infection. Regularly clean toilets, sinks, and door handles with disinfecting products, and wash laundry in hot water at temperatures of at least 130°F (60°C).
RELATED: Everything You Need to Know About Gallstones: Symptoms and Treatments
Long-Term Health Implications
Most people with dysentery recover fully within a few weeks with proper treatment. However, severe cases can lead to complications such as dehydration, which can cause life-threatening electrolyte imbalances and organ damage. In rare instances, bacillary dysentery may result in hemolytic uremic syndrome (HUS), a type of kidney damage, while amoebic dysentery can cause liver abscesses if left untreated.
To ensure a full recovery and prevent long-term health issues, it’s essential to seek medical attention if symptoms persist or worsen, and to complete the prescribed course of treatment. Maintaining a healthy diet, staying hydrated, and allowing your body sufficient time to rest and recover can also promote long-term digestive health after a bout of dysentery.
Conclusion
Sometimes, an additional medication may be prescribed to ensure all parasites are eradicated. In severe cases, a doctor might also recommend intravenous (IV) therapy to replenish fluids and prevent dehydration.
Dysentery infections can range from mild or asymptomatic to severe, typically lasting between several days to a few weeks, with an average duration of 4 to 7 days. The condition tends to be more severe in children than in adults. Vulnerable populations, including the elderly, those with weakened health, and individuals suffering from malnutrition, are especially at risk.