E. coli infection is a widespread concern that affects millions of people worldwide each year. This bacterial infection can lead to a range of health issues, from mild gastrointestinal discomfort to severe complications that may be life-threatening. Understanding the nature of E. coli infections, their symptoms, and available treatment options is crucial for both healthcare professionals and the general public to effectively manage and prevent these infections.
This comprehensive guide aims to shed light on the essential aspects of E. coli infection. It will cover the basics of the bacteria, common clinical manifestations, cutting-edge diagnostic techniques, and current treatment strategies. By exploring these key areas, readers will gain valuable insights into the prevention, diagnosis, and management of E. coli infections, empowering them to make informed decisions about their health and well-being.
E. Coli Basics
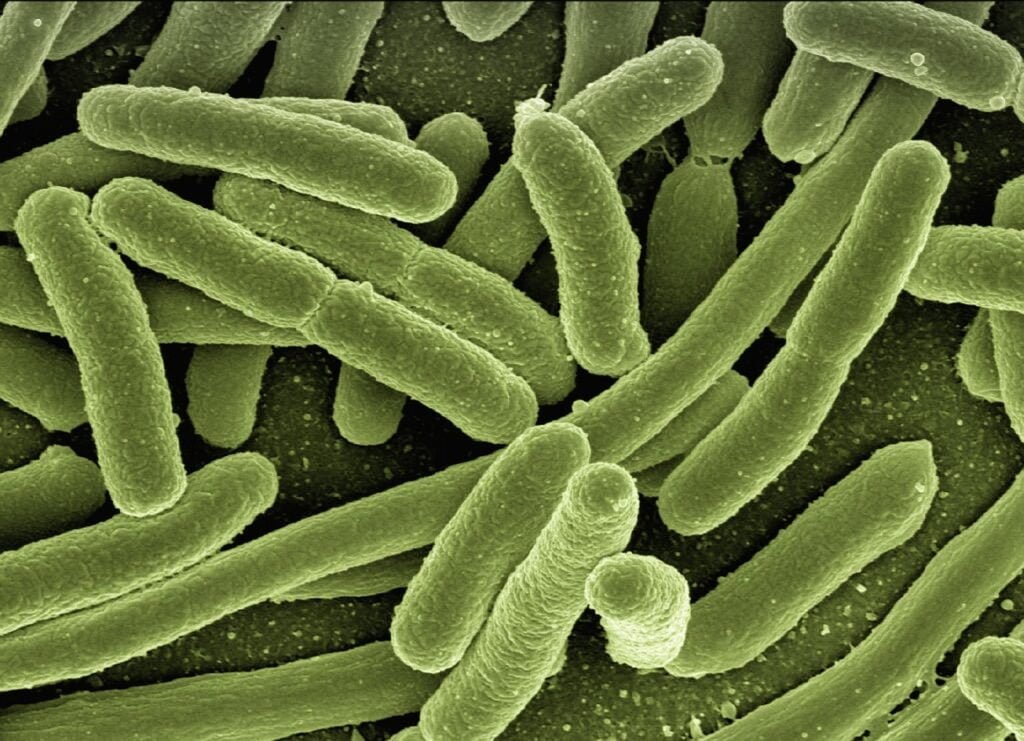
Escherichia coli (E. coli) is a type of bacteria commonly found in the intestines of people and animals. While most strains of E. coli are harmless, some can cause serious illness. The strains that cause diarrhea are the focus of this article.
Definition and Overview
E. coli are bacteria that normally live in the gut as part of a healthy intestinal tract. They help with digestion, vitamin production, and protection against harmful germs. However, certain strains of E. coli can lead to infections causing diarrhea, urinary tract infections, pneumonia, and sepsis.
Groups at increased risk for E. coli infection include:
- Children younger than 5
- Adults 65 and older
- People with weakened immune systems
- International travelers
Shiga toxin-producing E. coli (STEC) infections can be particularly serious, potentially leading to hemolytic uremic syndrome (HUS), which can cause kidney failure, permanent health problems, and even death.
RELATED: A Detailed Look at Plantar Fasciitis: Causes, Symptoms, and Treatments
Common Sources of Infection
E. coli infections often occur after ingesting contaminated food or water, or through contact with animals, environments, or infected individuals. Some common sources include:
- Undercooked ground meat products
- Raw milk and unpasteurized dairy products
- Contaminated raw fruits and vegetables
- Contaminated water sources (e.g., lakes, streams, pools, drinking water)
STEC outbreaks have been linked to various foods, such as undercooked hamburgers, salami, unpasteurized apple cider, yogurt, and raw milk cheese. Contaminated fruits and vegetables, such as sprouts, spinach, lettuce, and salads, have also been implicated in outbreaks.
Transmission Methods
E. coli primarily spreads through fecal-oral transmission, which occurs when bacteria from feces enter the mouth and digestive tract. This can happen through:
- Consuming contaminated foods or beverages
- Drinking or accidentally swallowing contaminated water
- Touching feces or contaminated surfaces and then touching the mouth
- Improper wiping after using the bathroom, leading to the spread of E. coli from feces to the urinary tract
Person-to-person transmission is also possible, especially when caring for someone with an E. coli infection or sharing contaminated objects or surfaces. Newborns can sometimes acquire E. coli infections during birth.
Understanding the basics of E. coli, including its definition, common sources of infection, and transmission methods, is crucial for preventing and managing these potentially serious infections.
Clinical Manifestations
The clinical manifestations of an E. coli infection can range from mild to severe, depending on the strain of bacteria and the individual’s overall health. Understanding the signs and symptoms is crucial for prompt diagnosis and treatment.
Mild to Moderate Symptoms
In most cases, an E. coli infection causes mild to moderate gastrointestinal symptoms, which may include:
- Diarrhea, which can be watery or bloody
- Abdominal cramps and pain
- Nausea and vomiting
- Low-grade fever
These symptoms typically appear within 3 to 4 days after exposure to the bacteria but can occur as early as 1 day or as late as a week post-exposure.
Severe Symptoms and Red Flags
In some instances, E. coli infections can lead to more severe symptoms that require immediate medical attention. These red flags include:
- Persistent, severe, or bloody diarrhea
- Extreme abdominal pain and tenderness
- High fever (over 102°F or 38.9°C)
- Decreased urine output or blood in the urine
- Pallor and easy bruising or bleeding
- Seizures or neurological changes
If any of these severe symptoms occur, it is essential to seek medical care promptly to prevent potentially life-threatening complications.
RELATED: Lupus: Understanding Symptoms, Causes, and Treatment Options
Hemolytic Uremic Syndrome
One of the most serious complications of E. coli infection, particularly with the O157:H7 strain, is hemolytic uremic syndrome (HUS). This condition affects the blood and blood vessels, leading to:
- Destruction of blood platelets
- Low red blood cell count (anemia)
- Kidney failure due to damage to the tiny blood vessels in the kidneys
HUS is more common in young children and older adults, and it requires immediate hospitalization and treatment to prevent permanent kidney damage or even death.
By recognizing the clinical manifestations of E. coli infection, from mild gastrointestinal symptoms to severe complications like HUS, healthcare providers and patients can work together to ensure timely diagnosis and appropriate treatment, minimizing the risk of long-term health consequences.
Diagnostic Techniques
The diagnosis of an e. coli infection involves a combination of clinical assessment, laboratory tests, and imaging studies. The specific diagnostic approach depends on the suspected site and severity of the infection.
Stool Culture
For gastrointestinal e. coli infections, stool culture is the primary diagnostic method. A sample of the patient’s stool is collected and sent to the laboratory for analysis. The stool sample is cultured on selective media to promote the growth of e. coli while inhibiting the growth of other bacteria. After incubation, the presence of e. coli colonies is confirmed through biochemical tests and serotyping.
Stool culture allows for the identification of the specific strain of e. coli responsible for the infection. This information is crucial for determining the appropriate treatment and assessing the potential for complications, such as hemolytic uremic syndrome (HUS) associated with Shiga toxin-producing e. coli (STEC) infections.
Molecular Testing
In addition to stool culture, molecular testing techniques have emerged as valuable tools for the rapid and accurate diagnosis of e. coli infections. These tests detect specific genes or virulence factors associated with pathogenic e. coli strains.
- Polymerase Chain Reaction (PCR): PCR is a highly sensitive and specific molecular technique that amplifies and detects specific DNA sequences. PCR assays can be designed to target genes encoding virulence factors, such as Shiga toxins (Stx1 and Stx2) produced by STEC strains. Real-time PCR allows for the rapid detection and quantification of e. coli in clinical samples.
- Multiplex PCR: Multiplex PCR assays simultaneously detect multiple virulence genes associated with different pathogenic e. coli strains. This approach enables the identification of the specific pathotype (e.g., STEC, EPEC, ETEC) responsible for the infection, aiding in the selection of appropriate treatment and infection control measures.
- DNA Microarrays: DNA microarrays are high-throughput platforms that allow for the simultaneous detection of multiple e. coli virulence genes. These assays use DNA probes immobilized on a solid surface to hybridize with complementary sequences in the clinical sample. Microarrays provide a comprehensive profile of the virulence factors present, facilitating the identification of the pathogenic e. coli strain.
Imaging Studies
Imaging studies play a role in the diagnosis of e. coli infections, particularly in cases of extraintestinal manifestations or complications. The choice of imaging modality depends on the suspected site of infection and the patient’s clinical presentation.
- Abdominal Imaging: In patients with severe abdominal pain or suspected complications, such as peritonitis or intra-abdominal abscesses, imaging studies are essential. Computed tomography (CT) scans or ultrasound examinations can reveal the presence of inflammation, fluid collections, or abscesses in the abdominal cavity.
- Urinary Tract Imaging: For patients with e. coli urinary tract infections (UTIs), imaging studies may be necessary to assess the extent of the infection and detect any structural abnormalities or complications. Renal ultrasound can evaluate for the presence of kidney stones, hydronephrosis, or renal abscesses. In complicated cases, CT or magnetic resonance imaging (MRI) may be used to visualize the urinary tract and surrounding structures.
- Neuroimaging: In rare cases of e. coli meningitis, neuroimaging studies, such as CT or MRI of the brain, may be performed to assess for the presence of intracranial complications, such as brain abscesses or ventriculitis.
The integration of clinical findings, laboratory tests, and imaging studies allows for a comprehensive diagnostic approach to e. coli infections. Prompt and accurate diagnosis is crucial for initiating appropriate treatment, preventing complications, and implementing necessary infection control measures.
Treatment and Management
Treatment for e. coli infections focuses on managing symptoms and preventing complications. The specific approach depends on the severity and location of the infection.
Supportive Care
In most cases of mild to moderate e. coli gastroenteritis, treatment primarily involves supportive care measures:
- Rehydration: Replacing fluids and electrolytes lost through diarrhea is crucial. Oral rehydration solutions are recommended for mild to moderate dehydration, while intravenous fluids may be necessary for severe cases.
- Rest: Allowing the body to rest and recover is important during the acute phase of the illness.
- Dietary modifications: Temporarily avoiding dairy products, fatty foods, and high-fiber foods can help reduce gastrointestinal distress. Gradually reintroducing these foods as symptoms improve is recommended.
Medication Options
Antibiotics are not routinely used to treat e. coli gastroenteritis, as they may prolong the duration of diarrhea and increase the risk of complications, particularly in infections caused by Shiga toxin-producing e. coli (STEC). However, antibiotics may be prescribed in certain situations:
- Severe infections: In cases of severe gastroenteritis or when the infection spreads beyond the intestines (such as in urinary tract infections or sepsis), antibiotics like fluoroquinolones, or cephalosporins may be used.
- Traveler’s diarrhea: Antibiotics such as azithromycin, fluoroquinolones may be prescribed to shorten the duration of traveler’s diarrhea caused by e. coli.
- Other extraintestinal infections: Treatment for e. coli infections outside the gastrointestinal tract, such as pneumonia or meningitis, typically involves targeted antibiotic therapy based on the specific location and severity of the infection.
Antimotility agents, such as loperamide, should be avoided in children and in cases of bloody diarrhea, as they may increase the risk of complications.
RELATED: Understanding Chlamydia: Symptoms, Causes, and Effective Treatments
Hospitalization Criteria
While most e. coli infections can be managed at home, hospitalization may be necessary in certain situations:
- Severe dehydration: Patients with signs of severe dehydration, such as decreased urine output, dizziness, or rapid heartbeat, may require intravenous fluid replacement and close monitoring.
- Hemolytic uremic syndrome (HUS): Patients with STEC infections who develop HUS, a serious complication affecting the kidneys and blood clotting system, require immediate hospitalization and specialized care.
- Invasive infections: Patients with e. coli infections that have spread to other parts of the body, such as the bloodstream or central nervous system, often require hospitalization for intensive treatment and monitoring.
- High-risk individuals: Infants, older adults, and those with weakened immune systems may be more likely to require hospitalization due to an increased risk of complications.
Close communication with healthcare providers is essential for determining the most appropriate treatment approach based on the individual’s specific circumstances and the severity of the infection.
Conclusion
E. coli infections pose a significant health challenge, ranging from mild discomfort to life-threatening complications. This guide sheds light on the key aspects of E. coli infections, including their sources, symptoms, and diagnostic methods. By understanding these factors, individuals can take steps to prevent infection and seek timely medical care when needed.
Proper diagnosis and treatment play a crucial role in managing E. coli infections effectively. While most cases resolve with supportive care, severe infections may require hospitalization and specialized treatment. Staying informed about E. coli infections empowers individuals to make smart health choices and helps healthcare providers offer the best possible care to patients.