Epididymitis is a condition that affects men’s reproductive health, causing inflammation of the epididymis, a coiled tube at the back of the testicle. This painful condition can have a significant impact on a man’s quality of life and fertility. Understanding the causes, symptoms, and available treatments is crucial for anyone experiencing or concerned about epididymitis.
This article delves into the intricacies of epididymitis, exploring its underlying causes and common symptoms. It also examines the diagnostic process and discusses various treatment options available to manage and resolve the condition. By providing comprehensive information, this guide aims to help readers better understand epididymitis and make informed decisions about their health care.
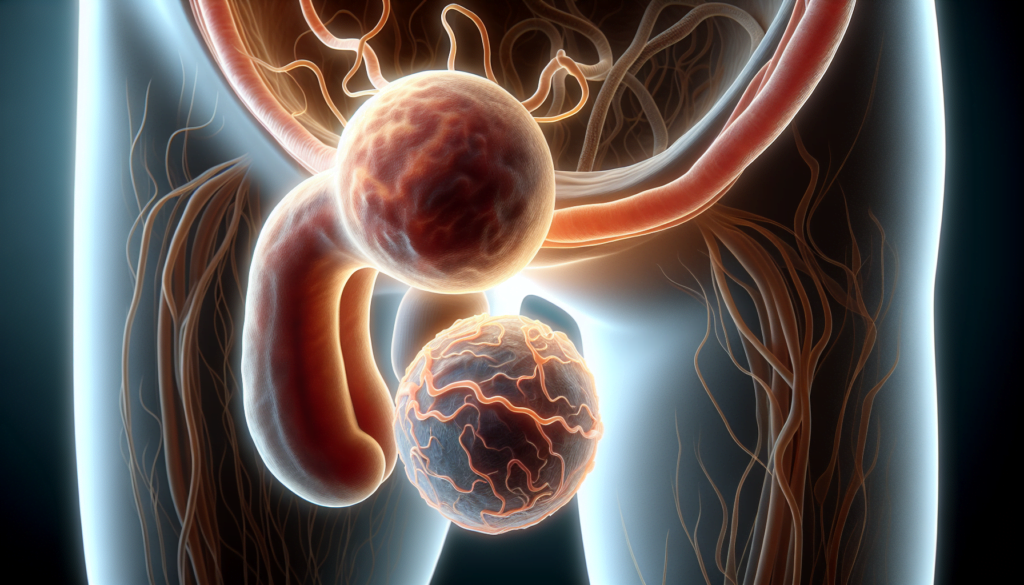
Understanding Epididymitis: Definition and Anatomy
The epididymis is a coiled tube located at the back of each testicle that stores and carries sperm. Epididymitis refers to the inflammation of this tube, which can cause pain, swelling, and discomfort in the scrotum. The condition can be acute (sudden onset) or chronic (long-term) and is typically caused by a bacterial infection.
What is the epididymis?
The epididymis is a series of small tubes that collects and stores sperm. It is attached to the back of each testicle and plays a crucial role in the male reproductive system. Sperm start growing in the testes and gain movement and maturity while moving through the epididymis. The epididymis is linked to the ejaculatory duct by the vas deferens, a tube that runs from the lower part of the scrotum into the pelvis.
RELATED: Understanding Atherosclerosis: Symptoms, Causes, and Treatments
Types of epididymitis
There are two main types of epididymitis:
- Acute epididymitis: This type is characterized by sudden onset of symptoms, such as redness, pain, and swelling in the scrotum. It is usually caused by a bacterial infection and can be treated with antibiotics.
- Chronic epididymitis: This type develops slowly and is a longer-term problem. The pain is typically duller compared to acute epididymitis, and symptoms may come and go. Chronic epididymitis can be more challenging to treat and may require a combination of antibiotics and anti-inflammatory medications.
Who is at risk?
Epididymitis can occur at any age, but it is most common in men between the ages of 14 and 35. Several factors can increase the risk of developing epididymitis, including:
- Urinary tract infections (UTIs)
- Sexually transmitted infections (STIs), such as chlamydia and gonorrhea
- Prostate enlargement or infection (prostatitis)
- Recent catheter use or genito-urinary surgery
- Congenital kidney and bladder problems
Understanding the anatomy of the epididymis and the types of epididymitis is essential for recognizing symptoms and seeking appropriate treatment. By identifying risk factors and taking preventive measures, such as practicing safe sex and maintaining good hygiene, individuals can reduce their likelihood of developing this painful condition.
Common Causes of Epididymitis
Epididymitis can have an impact on a man’s reproductive health and quality of life. Understanding the common causes of this condition is crucial for prevention, early diagnosis, and effective treatment. The most frequent causes of epididymitis include bacterial infections, sexually transmitted infections (STIs), and non-infectious factors.
Bacterial infections are a leading cause of epididymitis, particularly in older men. These infections often occur due to the retrograde flow of urine from the bladder or urethra into the epididymis. The most common bacterial pathogens responsible for epididymitis include Escherichia coli and other enteric organisms.
Sexually transmitted infections, such as chlamydia and gonorrhea, are significant causes of epididymitis in sexually active men, especially those between the ages of 14 and 35. These infections are transmitted through sexual contact and can ascend from the urethra to the epididymis, causing inflammation and pain.
- Chlamydia trachomatis
- Neisseria gonorrhoeae
- Mycoplasma genitalium
Non-infectious causes of epididymitis, while less common, can still contribute to the development of this condition. These factors include:
- Trauma or injury to the scrotum
- Urinary tract abnormalities, such as bladder outlet obstruction
- Autoimmune disorders
- Certain medications
Recognizing the risk factors and understanding the common causes of epididymitis can help individuals take preventive measures, such as practicing safe sex and maintaining good hygiene, to reduce their likelihood of developing this painful condition. Early diagnosis and appropriate treatment are essential to prevent complications and promote recovery.
Recognizing Symptoms and Seeking Diagnosis
Epididymitis often presents with a gradual onset of scrotal pain and swelling, usually affecting one testicle. The pain may begin in the flank and migrate to the scrotum. Urinary symptoms such as dysuria, frequency, urgency, or incontinence may also be present. A urethral discharge might be observed in some cases.
Key symptoms
- Scrotal pain and swelling, usually unilateral
- Tenderness upon palpation of the epididymis
- Warm, erythematous, and indurated skin overlying the scrotum
- Tender inguinal adenopathy
- Urethral discharge
Diagnostic procedures
Evaluation of epididymitis begins with urinalysis, which may reveal red and white blood cells, indicating an acute infectious or inflammatory condition. Urine culture helps determine the causative agent in cases associated with urinary tract infection. A urethral swab is indicated when a sexually transmitted disease is suspected.
Radiographic evaluation includes ultrasonography to assess anatomic structure and vascular flow to the testis. Ultrasonography can demonstrate inflammation of the epididymis and testis in cases of epididymitis and epididymo-orchitis. Computerized tomography may be useful when the patient has flank pain and urinary symptoms associated with an acute genitourinary problem such as ureterolithiasis.
RELATED: Atelophobia(Fear of Imperfection): Causes, Symptoms, and How to Overcome It
Differential diagnosis
Ruling out testicular torsion is of utmost importance, as it is a surgical emergency. While epididymitis tends to occur gradually, the pain associated with testicular torsion often occurs abruptly. Other conditions to consider in the differential diagnosis include:
- Scrotal hernia
- Inguinal hernia
- Idiopathic scrotal edema
- Reactive hydrocele
- Pyocele
- Henoch-Schönlein purpura
- Behçet disease
- Polyarteritis nodosa
- Vasculitis
- Referred or radicular pain
- Epididymal cyst
- Epididymal congestion following vasectomy
- Spermatocele
- Testicular tumor (hemorrhage into tumor)
- Tunica vaginalis tumors: Mesothelioma
- Varicocele
- Urinary tract infection
Prompt recognition of symptoms and appropriate diagnostic evaluation are essential for the effective management of epididymitis and the prevention of complications.
Treatment Options and Recovery
The primary goal of treating epididymitis is to alleviate symptoms, eliminate the underlying infection, and prevent complications. Treatment typically involves a combination of antibiotic therapy, pain management, and lifestyle modifications.
Pain management
Pain and discomfort associated with epididymitis can be managed with the following measures:
- Rest and scrotal elevation
- Application of cold packs to the affected area
- Over-the-counter pain relievers, such as ibuprofen or acetaminophen
- Wearing supportive underwear or an athletic supporter
RELATED: Articulation Disorder: Symptoms, Diagnosis, and Therapy Options
Lifestyle modifications
In addition to medical treatment, certain lifestyle changes can aid in the recovery process and prevent future episodes of epididymitis:
- Abstaining from sexual activity until the infection has cleared
- Practicing safe sex, including using condoms, to reduce the risk of sexually transmitted infections
- Maintaining good genital hygiene
- Avoiding heavy lifting or strenuous activities during recovery
Potential complications
While most cases of epididymitis resolve with appropriate treatment, complications can occur if the condition is left untreated or if the infection spreads. Potential complications include:
- Chronic epididymitis
- Abscess formation
- Testicular infarction (loss of blood supply to the testicle)
- Infertility
Prompt diagnosis and treatment are essential to minimize the risk of complications and ensure a full recovery. Follow-up with a healthcare provider is recommended to monitor progress and adjust treatment if necessary.
Conclusion
Epididymitis has a significant impact on men’s reproductive health and overall well-being. This article has delved into the causes, symptoms, and treatments of this condition to provide a comprehensive understanding. By exploring the anatomy of the epididymis, common risk factors, and diagnostic procedures, readers are now better equipped to recognize the signs of epididymitis and seek timely medical attention.
To wrap up, proper management of epididymitis involves a combination of antibiotic therapy, pain relief, and lifestyle changes. Early diagnosis and appropriate treatment are crucial to prevent complications and ensure a full recovery. By staying informed and taking preventive measures, individuals can protect their reproductive health and maintain a good quality of life.