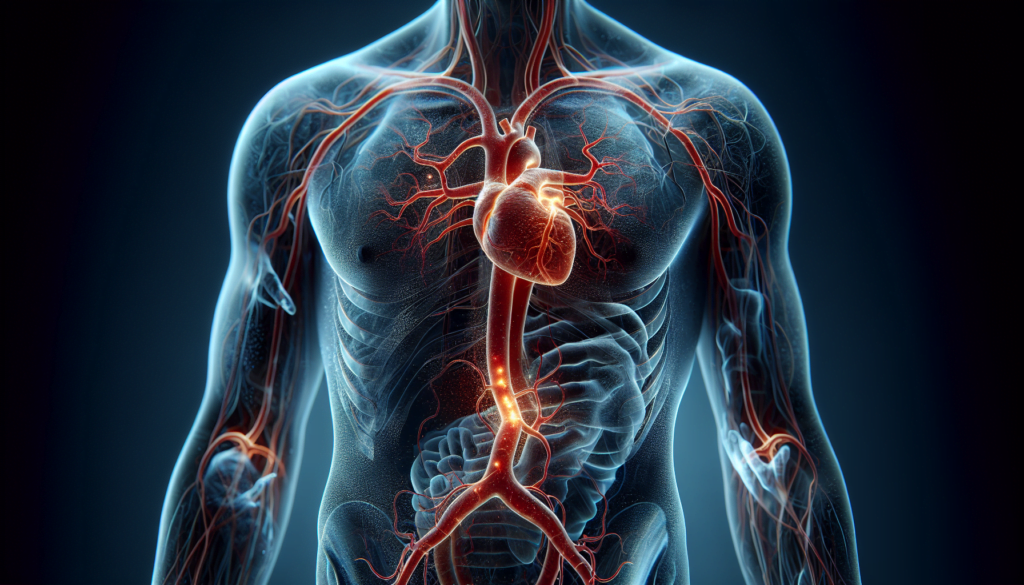
An aortic aneurysm is a life-threatening condition that demands immediate attention. This bulge in the wall of the aorta, the main artery carrying blood from the heart to the rest of the body, can lead to severe complications if left untreated. Understanding the nature of aortic aneurysms is crucial for early detection and effective management, potentially saving lives.
This comprehensive guide delves into the various aspects of aortic aneurysms. It explores different types, examines causes and risk factors, and discusses diagnosis and screening methods. The article also looks at treatment approaches, ranging from watchful waiting to surgical interventions. By shedding light on this serious condition, readers can gain valuable insights to protect their health or support loved ones facing this challenge.
Types of Aortic Aneurysms
Aortic aneurysms can develop in different regions of the aorta, each with its own characteristics and potential complications. The three main types of aortic aneurysms are thoracic aortic aneurysms, abdominal aortic aneurysms, and thoracoabdominal aortic aneurysms.
Thoracic aortic aneurysms occur in the part of the aorta that runs through the chest. They are most often located in the ascending aorta, which is the section closest to the heart. Risk factors for thoracic aortic aneurysms include genetic disorders like Marfan syndrome, Loeys-Dietz syndrome, and vascular Ehlers-Danlos syndrome, as well as bicuspid aortic valve and a family history of aneurysms.
Abdominal aortic aneurysms (AAAs) are the most common type of aortic aneurysm, occurring in the part of the aorta that passes through the abdomen. AAAs are more prevalent in older men, especially those with risk factors such as smoking, high blood pressure, and a family history of the condition. Women with AAAs generally suffer ruptures more often and with smaller aneurysm sizes compared to men.
RELATED: The Complete Guide to Arrhythmia: Symptoms, Causes, and Treatments
Thoracoabdominal aortic aneurysms are complex aneurysms that extend from the chest to the abdomen. They are classified according to the Crawford Classification system, which categorizes them based on their location and extent:
- Extent I: Involves the majority of the descending thoracic aorta and the upper abdominal aorta
- Extent II: Involves the majority of the descending thoracic aorta and the majority of the abdominal aorta
- Extent III: Involves the lower descending thoracic aorta and the majority of the abdominal aorta
- Extent IV: Involves most or all of the abdominal aorta
- Extent V: Involves the lower descending thoracic aorta and the upper abdominal aorta
The most common cause of thoracoabdominal aortic aneurysms is atherosclerosis, which is a hardening of the arteries caused by plaque buildup. Other risk factors include smoking, high blood pressure, high cholesterol, being overweight, a family history of cardiovascular disease, older age, and genetic disorders affecting connective tissue.
Causes and Risk Factors
Several factors can contribute to the development of an aortic aneurysm. These include genetic factors, lifestyle choices, and certain medical conditions.
Genetic factors play a significant role in the development of aortic aneurysms. Certain genetic disorders, such as Marfan syndrome, Loeys-Dietz syndrome, and Ehlers-Danlos syndrome, can weaken the aortic wall, making it more susceptible to aneurysm formation. Familial thoracic aortic aneurysms (FTAA) can also occur in families without a known genetic syndrome, suggesting an inherited component.
Lifestyle factors, such as smoking and high blood pressure, can also increase the risk of developing an aortic aneurysm. Smoking weakens the aortic wall and accelerates the growth of existing aneurysms. High blood pressure puts additional stress on the aortic wall, making it more likely to bulge or rupture.
Certain medical conditions can also increase the risk of aortic aneurysms. These include:
- Atherosclerosis: The buildup of plaque in the arteries can weaken the aortic wall.
- Bicuspid aortic valve: A congenital heart defect where the aortic valve has only two leaflets instead of the usual three, increasing the risk of aortic aneurysm.
- Inflammatory conditions: Vasculitis and other inflammatory diseases can damage the aortic wall.
- Infections: Rarely, untreated infections such as syphilis or salmonella can lead to aortic aneurysms.
Age and gender also play a role in aortic aneurysm risk. Abdominal aortic aneurysms are more common in men over 65 years old, while thoracic aortic aneurysms can occur at any age but are more likely to cause complications in older individuals.
Diagnosis and Screening
Abdominal aortic aneurysms (AAAs) are often asymptomatic until they rupture, making early detection crucial. Diagnosis and screening involve various imaging techniques and guidelines to identify individuals at risk.
Imaging Techniques
Ultrasonography is the primary method for AAA screening due to its high sensitivity (94-100%) and specificity (98-100%). It is noninvasive, simple to perform, and does not expose patients to radiation. Computed tomography (CT) is an accurate tool for identifying AAAs but is not recommended as a screening method due to potential radiation exposure risks. Physical examination has low sensitivity (39-68%) and specificity (75%) and is not recommended for screening.
RELATED: Understanding Arithmophobia (Fear of Numbers): Causes, Symptoms, and Solutions
Screening Guidelines
The United States Preventive Services Task Force (USPSTF) recommends one-time screening for AAA with ultrasonography in men aged 65 to 75 years who have ever smoked (at least 100 cigarettes in their lifetime). They also recommend selectively offering screening to men aged 65 to 75 years who have never smoked, considering factors such as medical history, family history, and other risk factors. The USPSTF recommends against routine screening in women who have never smoked and have no family history of AAA. Evidence is insufficient to assess the balance of benefits and harms of screening in women aged 65 to 75 years who have ever smoked or have a family history of AAA.
Genetic Testing
Genetic testing can help identify individuals with a higher risk of developing AAAs due to specific gene mutations. More than 25 genes have been identified in hereditary thoracic aortic diseases (HTADs), with some causing syndromic conditions like Marfan syndrome and others causing familial thoracic aortic aneurysms. Genetic testing is recommended for individuals with a family history of AAAs or those presenting with AAAs at a young age. Identifying the specific gene responsible can guide treatment decisions and help screen family members who may be at risk. However, genetic testing may not always identify a pathogenic variant, and further research is needed to discover new genetic variants that explain aneurysm disease.
Treatment Approaches
The goal of aortic aneurysm treatment is to prevent the aneurysm from growing and rupturing. Treatment approaches depend on the aneurysm’s size, location, and the patient’s overall health. Options include medical management, open surgical repair, and endovascular aneurysm repair (EVAR).
Medical Management
For small aortic aneurysms (less than 5.5 cm in diameter), medical management is often recommended. This approach involves:
- Regular monitoring with imaging tests to track the aneurysm’s growth
- Managing risk factors such as high blood pressure, high cholesterol, and smoking
- Prescribing medications like beta-blockers and angiotensin 2 receptor blockers to reduce stress on the aortic wall
RELATED: Armpit Yeast Infection: Diagnosis, Treatment, and Prevention
Open Surgical Repair
Open surgical repair is typically recommended for larger aneurysms (greater than 5.5 cm) or rapidly growing aneurysms. The procedure involves:
- Making a large incision in the abdomen or chest to access the aorta
- Removing the damaged section of the aorta
- Replacing it with a synthetic graft that is sewn into place
Recovery from open surgery can take several weeks to months.
Endovascular Aneurysm Repair (EVAR)
EVAR is a minimally invasive alternative to open surgery. It is suitable for patients with certain anatomical characteristics and has a faster recovery time. The procedure involves:
- Inserting a catheter through a small incision in the groin
- Guiding the catheter to the aneurysm site using imaging techniques
- Deploying a stent-graft to reinforce the weakened aortic wall and prevent rupture
Regular follow-up imaging is necessary after EVAR to monitor for potential complications, such as endoleaks.
The choice of treatment depends on individual factors, and the patient should discuss the risks and benefits of each approach with their healthcare provider.
Conclusion
Aortic aneurysms are serious health concerns that have a significant impact on many lives. This article has explored the different types, causes, risk factors, diagnosis methods, and treatment options for this condition. Understanding these aspects is crucial to recognize the signs early and get timely medical help. It’s essential to keep in mind that early detection and proper management can greatly improve outcomes for those affected by aortic aneurysms.
While medical advancements have led to better diagnostic tools and treatment options, prevention remains key. Lifestyle changes, regular check-ups, and awareness of family history can play a vital role in reducing the risk of aortic aneurysms. For those diagnosed with this condition, working closely with healthcare providers to create a tailored treatment plan is crucial. As research continues, we can hope for even more effective ways to prevent, detect, and treat aortic aneurysms in the future.