Genital warts are a common sexually transmitted infection that affects millions of people worldwide. Caused by certain strains of the human papillomavirus (HPV), these small, flesh-colored growths can appear on the genitals, anus, and surrounding areas. While often harmless, genital warts can cause discomfort, embarrassment, and concerns about sexual health and relationships.
Understanding genital warts is crucial for prevention, early detection, and effective management. This article delves into the causes, symptoms, and diagnosis of genital warts, as well as exploring treatment options and prevention strategies. By shedding light on this prevalent condition, we aim to empower readers with knowledge to protect their health and make informed decisions about their sexual well-being.
Understanding HPV and Genital Warts


Human papillomavirus (HPV) is a highly common sexually transmitted infection that affects millions worldwide. There are over 100 different known types of HPV viruses, with certain strains causing genital warts. HPV types 6 and 11 are responsible for approximately 90% of genital wart cases. These warts typically appear in clusters or as separate growths on the genital or anal area.
Types of HPV
HPV strains can be categorized into two main groups:
- Low-risk HPV: These strains, such as types 6 and 11, cause genital warts but are not associated with cancer.
- High-risk HPV: Strains like types 16 and 18 are linked to various cancers, including cervical, anal, penile, vaginal, vulvar, and oropharyngeal cancers. However, most people infected with these strains do not develop cancer.
It is possible to be infected with multiple HPV strains simultaneously.
Transmission
Genital HPV infections are primarily spread through penetrative sex, although transmission can also occur through non-penetrative sexual activity, albeit less commonly. The virus is transmitted through direct skin-to-skin contact with an infected individual, usually during sexual intercourse. Factors that influence transmission include:
- Number of sexual partners
- Frequency of sexual contact with an infected partner
- Use of condoms (which may reduce but not eliminate risk)
- Presence of other sexually transmitted infections
- Smoking status
Approximately three out of four unaffected partners of patients with genital warts develop them within eight months of contact.
RELATED: Sundowning Explained: Symptoms, Causes, and How to Manage
Risk factors
Several factors can increase the likelihood of contracting genital HPV:
- Being sexually active at a young age
- Having multiple sexual partners
- Engaging in unprotected sex
- Having a weakened immune system due to conditions like HIV or immunosuppressive medications
- Smoking
Although most HPV infections are cleared by the body’s immune system within two years, the virus can remain latent and cause recurrences months or even years later. Latent HPV is still transmissible, and unprotected sex with an infected partner carries a 70% chance of infection.
Understanding the types, transmission, and risk factors associated with HPV is crucial for preventing the spread of genital warts and other HPV-related complications. Regular screening, vaccination, and practicing safe sex are essential steps in reducing the impact of this prevalent virus.
Recognizing Genital Warts
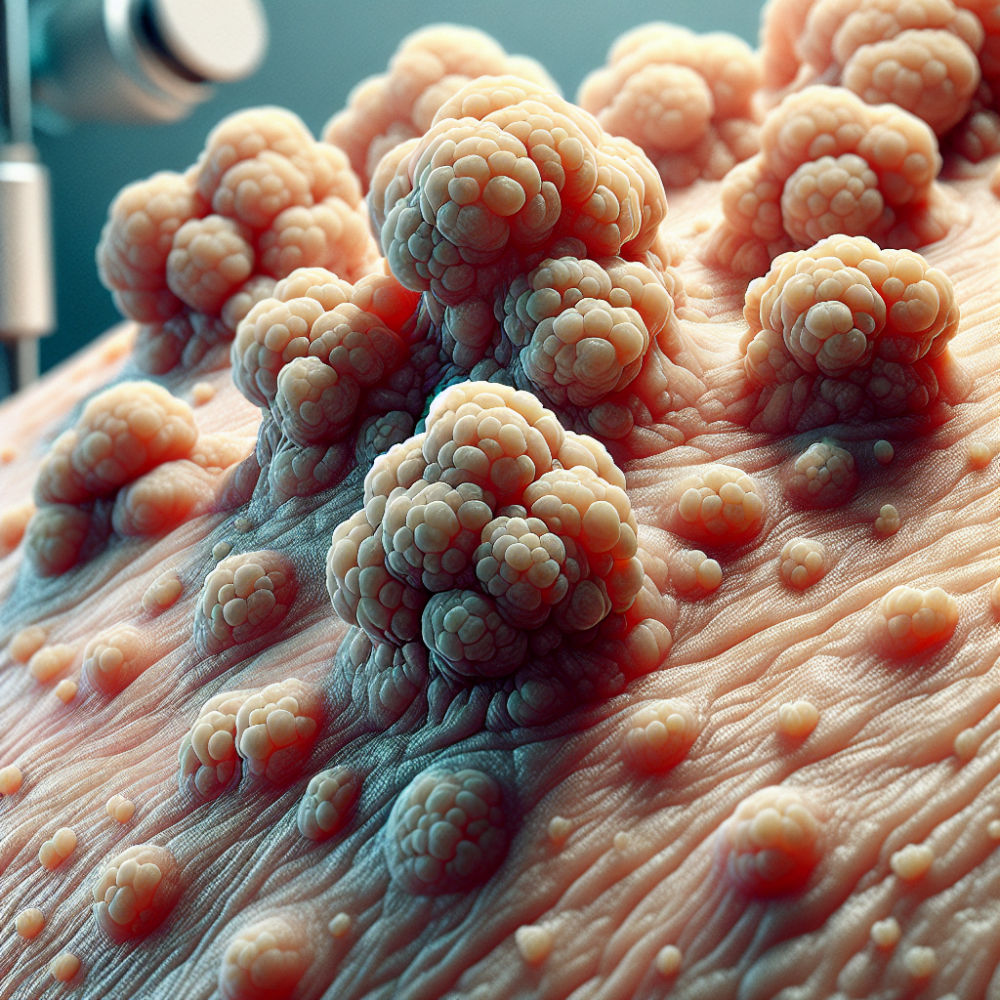
Genital warts appear as small, flesh-colored or whitish bumps in the genital area. They often resemble tiny pieces of cauliflower and can be found on the vulva, vagina, cervix, penis, scrotum, or anus. The warts may be itchy but are usually not painful. It is important to note that not all bumps in the genital area are warts, as there are other infections and normal skin conditions that may look similar.
Location on the body
In women, genital warts can grow on the vulva, walls of the vagina, area between the outer genitals and anus, anal canal, and cervix. In men, they may appear on the tip or shaft of the penis, scrotum, or anus. Genital warts can also form in the mouth or throat of a person who has had oral sex with an infected individual.
Physical characteristics
Genital warts caused by HPV can be flesh-colored or slightly darker than the surrounding skin. They may appear as a single bump or in clusters, and their size can vary from small to large. The surface of genital warts is often described as bumpy or rough, resembling a cauliflower. In some cases, the warts may cause itching or discomfort, and they might bleed during sexual intercourse.
RELATED: 16 Low Carb Vegetables That Will Transform Your Diet
Differentiating from other conditions
It is crucial to differentiate genital warts from other skin conditions, such as skin tags. While skin tags are soft, flesh-colored growths that often develop in areas where the skin folds, they are not caused by HPV and are not contagious. Skin tags typically have a smooth surface and a thin stalk connecting them to the skin, whereas genital warts have a rough, cauliflower-like appearance and a broader base.
If you suspect that you have genital warts or have been exposed to HPV, it is essential to consult with a healthcare professional for an accurate diagnosis. They can perform a physical examination and, if necessary, take a biopsy of the affected area to confirm the presence of genital warts. Early detection and treatment can help prevent the spread of HPV and reduce the risk of potential complications.
Diagnostic Procedures
Diagnosing genital warts involves a combination of physical examination, Pap smear, and HPV DNA testing. Healthcare professionals often can identify genital warts during a physical exam. They may use a colposcope, a special magnifying instrument, to examine the genital area more closely and spot warts that are not visible to the naked eye. In some cases, a small tissue sample (biopsy) may be taken for laboratory analysis to confirm the diagnosis.
For women, regular Pap smears are crucial in detecting abnormal changes in the cervical cells caused by HPV. During a Pap test, a healthcare provider collects cells from the cervix using a soft brush and a flat scraping device called a spatula. The collected cells are then examined under a microscope for any irregularities. Pap tests can help identify precancerous changes in the cervix, allowing for early intervention and treatment.
In addition to Pap smears, HPV DNA testing can be performed to determine the presence of high-risk HPV strains that are known to cause cervical cancer. This test is often done in conjunction with a Pap smear for women aged 30 and above. HPV DNA testing involves analyzing cervical cells for the presence of HPV genetic material. If high-risk HPV strains are detected, further evaluation and monitoring may be necessary.
It is important to note that while genital warts are a visible sign of HPV infection, not all HPV infections cause warts. Many people with HPV do not develop any symptoms, which is why regular screening through Pap smears and HPV testing is essential for early detection and prevention of HPV-related complications.
If you suspect that you have genital warts or have been exposed to HPV, it is crucial to consult with a healthcare professional for an accurate diagnosis. They will perform a thorough examination and recommend the appropriate tests based on your individual circumstances. Early diagnosis and treatment can help prevent the spread of HPV and reduce the risk of potential health problems associated with the virus.
Treatment Approaches
There are several treatment options available for genital warts, depending on the location, size, and number of warts present. The goal of treatment is to remove visible warts and reduce the risk of transmission to sexual partners. However, it is important to note that while treatments can remove the warts, they do not eliminate the underlying HPV infection.
Prescription creams and ointments are often the first line of treatment for genital warts. These topical medications work by stimulating the immune system to fight the virus or by directly destroying the wart tissue. Some common prescription creams include:
- Podophyllin (Podocon-25) and podofilox (Condylox): These solutions destroy genital wart tissue. Podophyllin is applied by a healthcare professional, while podofilox can be self-applied at home. These medications should never be used inside the body and are not recommended during pregnancy.
- Sinecatechins: This ointment, made from green tea extract, is used to treat genital warts on the body and around the anus. It is applied three times a day for up to 16 weeks.
Cryotherapy, also known as cryosurgery, is another common treatment for genital warts. This procedure involves freezing the warts with liquid nitrogen, causing them to blister and eventually fall off. The recovery time depends on the location and number of warts removed, but healing usually occurs within 1 to 3 weeks. After treatment, patients may experience irritation, soreness, swelling, and the shedding of dead tissue.
Cryotherapy is often used when genital warts are visible, growing in a small area, or causing discomfort. It is usually not recommended for widespread warts. While cryotherapy can be effective in removing genital warts, they may grow back, requiring multiple treatments. Risks associated with cryotherapy include pain during and after treatment, skin color changes, blisters, and skin irritation.
Electrocautery is a procedure that uses a low-voltage electrified probe to burn off genital warts. It is typically performed in a doctor’s office or clinic, and a local anesthetic is used for pain control. In some cases, general anesthesia may be necessary, depending on the number and location of the warts being treated.
The recovery time for electrocautery varies based on the extent of the treatment. Patients may experience pain, swelling, and redness following the procedure. Healing usually takes 2 to 4 weeks, and the treated area may be more sensitive during this time. Electrocautery can leave scars and may require multiple sessions to completely remove the warts.
Electrocautery is an effective treatment option for genital warts, as it removes them with minimal blood loss. However, as with other treatments, there is a risk of the warts recurring. Other potential risks include bleeding, infection, and pain following the procedure.
Living with Genital Warts
Living with genital warts can be challenging, both physically and emotionally. However, understanding how to manage outbreaks, cope with the emotional impact, and communicate with partners can help individuals navigate this condition effectively.
Managing Outbreaks
Genital warts are caused by certain strains of the human papillomavirus (HPV) and can recur even after successful treatment. To manage outbreaks, individuals can:
- Practice good hygiene: Keeping the affected area clean and dry can help prevent the spread of HPV and reduce the risk of secondary infections.
- Use barrier protection: Condoms and dental dams can help reduce the risk of transmitting HPV to sexual partners, although they do not provide complete protection.
- Avoid irritants: Tight clothing, fragranced products, and excessive friction can irritate the skin and exacerbate symptoms.
- Seek prompt treatment: If warts reappear, consulting with a healthcare provider can help ensure timely and effective treatment.
Emotional Impact
An HPV diagnosis can take a toll emotionally, leading to feelings of shame, guilt, and anxiety. Some individuals may withdraw socially or experience symptoms of depression. It is essential to remember that having a sexually transmitted infection does not define a person’s worth and that with proper management, individuals can lead fulfilling lives.
Coping strategies may include:
- Educating oneself about HPV to dispel myths and misconceptions
- Joining a support group or seeking counseling to process emotions
- Engaging in self-care activities to promote overall well-being
- Communicating openly with trusted friends, family members, or partners
RELATED: Top 10 Foods to Avoid with Diabetes for Better Health
Talking to Partners
Disclosing an HPV diagnosis to sexual partners can be daunting, but it is an important step in maintaining honest and healthy relationships. When discussing HPV with a partner, individuals should:
- Choose an appropriate time and place for the conversation, ensuring privacy and minimal distractions.
- Provide accurate information about HPV, its transmission, and potential health implications.
- Emphasize that HPV is common and that having the virus does not indicate infidelity or promiscuity.
- Discuss prevention strategies, such as vaccination and regular screenings, to protect both partners’ health.
- Allow the partner time to process the information and ask questions, offering resources for further education if needed.
While some partners may react with fear or judgment, others may be understanding and supportive. If a partner becomes emotionally or physically abusive, individuals should prioritize their safety and seek help from a trusted friend, family member, or professional organization.
Living with genital warts requires patience, self-compassion, and open communication. By taking proactive steps to manage outbreaks, address emotional challenges, and maintain healthy relationships, individuals can successfully navigate the impact of HPV on their lives.
Conclusion
Genital warts, caused by certain strains of HPV, have a significant impact on millions worldwide. This article has explored the causes, symptoms, diagnosis, and treatment options for this common sexually transmitted infection. Understanding the nature of genital warts and HPV is crucial to prevent transmission and manage the condition effectively. From recognizing the physical characteristics of warts to exploring various treatment approaches, individuals can take proactive steps to protect their sexual health.
Living with genital warts involves more than just managing outbreaks. It requires addressing the emotional impact and maintaining open communication with partners. By educating themselves, seeking appropriate medical care, and adopting prevention strategies, individuals can navigate the challenges posed by genital warts. In the end, a combination of awareness, proper treatment, and emotional support can help people lead healthy, fulfilling lives while managing this condition.