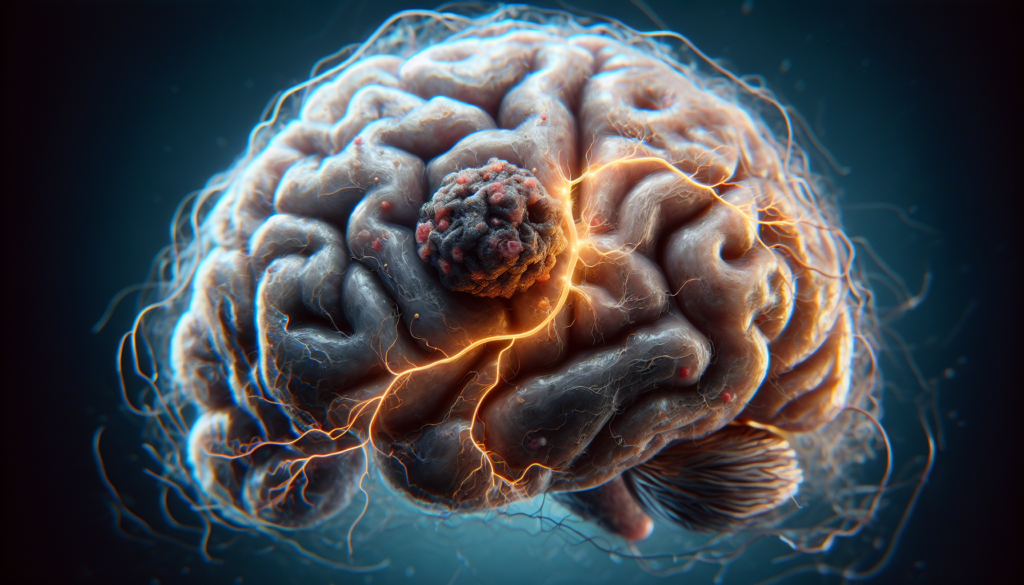
Glioblastoma (GBM) is a devastating form of brain cancer that strikes fear into the hearts of patients and their families. This aggressive tumor grows rapidly in the brain, causing a range of severe symptoms and posing significant challenges for treatment. Despite advances in medical science, glioblastoma remains one of the most difficult cancers to treat, with a poor prognosis for most patients.
Understanding glioblastoma is crucial for patients, caregivers, and healthcare professionals alike. This article delves into the biology of this complex disease, explores the current multimodal treatment approaches, and discusses strategies to manage complications and side effects. By shedding light on the latest research and treatment options, we aim to provide a comprehensive overview of glioblastoma and offer hope for those affected by this formidable condition.
The Biology of Glioblastoma
Glioblastoma (GBM) is a highly aggressive and infiltrative primary brain tumor that arises from glial cells. The biology of GBM is complex, involving various genetic and molecular alterations that contribute to its malignant behavior and therapeutic resistance.
Cell Origin and Tumor Microenvironment
GBM can originate from different cell types, including neural stem cells, glial progenitors, and astrocytes. The tumor microenvironment plays a crucial role in GBM progression and consists of various non-neoplastic cells, such as immune cells, endothelial cells, and reactive astrocytes. These cells interact with tumor cells through complex signaling networks, promoting tumor growth, invasion, and immunosuppression.
Genetic and Molecular Alterations
GBM is characterized by a wide range of genetic and molecular alterations that drive its malignant behavior. Some of the most common alterations include:
- Loss of heterozygosity (LOH) on chromosome 10q
- Amplification of the epidermal growth factor receptor (EGFR) gene
- Mutations in the tumor suppressor genes TP53 and PTEN
- Overexpression of the vascular endothelial growth factor (VEGF)
- Alterations in the PI3K/Akt/mTOR and Ras/MAPK signaling pathways
These genetic and molecular changes contribute to the uncontrolled proliferation, survival, and invasive properties of GBM cells.
RELATED: Cushing Syndrome: A Detailed Look at Causes and Treatment
Tumor Growth and Invasion
GBM exhibits rapid growth and extensive infiltration into the surrounding brain parenchyma, making complete surgical resection challenging. The invasive nature of GBM cells is facilitated by several factors, including:
- Extracellular matrix remodeling: GBM cells secrete matrix metalloproteinases (MMPs) that degrade the extracellular matrix, enabling tumor cell migration and invasion.
- Angiogenesis: GBM is highly vascularized, with tumor cells secreting pro-angiogenic factors such as VEGF to promote the formation of new blood vessels, which support tumor growth and provide routes for invasion.
- Interactions with the tumor microenvironment: GBM cells communicate with various non-neoplastic cells in the tumor microenvironment, such as immune cells and reactive astrocytes, through complex signaling networks that promote tumor growth and invasion.
The biology of GBM is a complex interplay of genetic and molecular alterations, cell-cell interactions, and the influence of the tumor microenvironment. Understanding these factors is crucial for developing effective therapeutic strategies targeting the various aspects of GBM biology.
Multimodal Treatment Approach
The treatment of glioblastoma (GBM) involves a multimodal approach that combines maximal safe resection, radiation therapy, and chemotherapy. This comprehensive strategy aims to maximize tumor control while preserving the patient’s neurological function and quality of life.
Maximal safe resection is the cornerstone of GBM treatment. Advanced intraoperative imaging techniques, such as (5-ALA) fluorescence, have improved the extent of resection while minimizing the risk of neurological deficits. Intraoperative MRI (IoMRI) and ultrasound (IoUS) provide real-time guidance during surgery, enabling surgeons to achieve a more complete resection. Neuronavigation and diffusion tensor imaging (DTI) tractography help identify and preserve critical white matter tracts.
Following surgery, radiation therapy is typically administered to eradicate residual tumor cells and prevent recurrence. Intensity-modulated radiation therapy (IMRT) and stereotactic radiosurgery (SRS) deliver precise, high-dose radiation to the tumor while sparing healthy brain tissue. These advanced techniques have improved local tumor control and reduced radiation-related side effects.
Concurrent with radiation therapy, patients receive chemotherapy, usually with (TMZ). TMZ is an alkylating agent that crosses the blood-brain barrier and has demonstrated significant survival benefits when combined with radiation. Other chemotherapeutic agents, may be used as second-line treatments, an anti-angiogenic agent, for recurrent GBM.
RELATED: Understanding Costochondritis: Causes and Treatment Options
Novel therapies and clinical trials are continuously being developed to improve outcomes for GBM patients. Immunotherapies, such as checkpoint inhibitors and vaccines, harness the patient’s immune system to fight the tumor. Targeted therapies, like EGFR inhibitors, aim to disrupt specific molecular pathways involved in tumor growth and invasion. Gene therapy and oncolytic viruses are also being investigated as potential treatment options.
In conclusion, the multimodal treatment approach for GBM combines maximal safe resection, advanced radiation therapy techniques, and chemotherapy to improve survival and quality of life. Ongoing research and clinical trials continue to explore novel therapies to further enhance outcomes for patients with this devastating disease.
Managing Complications and Side Effects
The management of complications and side effects is a critical aspect of glioblastoma (GBM) treatment. Patients with GBM often experience neurological deficits, seizures, and adverse effects from steroid use, which can significantly impact their quality of life.
Neurological Deficits
GBM can cause a range of neurological deficits, including motor weakness, sensory changes, and cognitive impairment. These deficits are often related to the location and extent of the tumor. Rehabilitation therapies, such as physical therapy, occupational therapy, and speech therapy, can help patients manage these deficits and maintain their functional independence.
Seizure Management
Seizures are a common complication of GBM, occurring in up to 60% of patients. Antiepileptic drugs (AEDs) are the mainstay of seizure management in GBM patients. Other AEDs, may be used as add-on therapy for uncontrolled seizures. In the end-of-life phase, when oral intake is hampered, benzodiazepines via nonoral routes can be used for seizure control.
RELATED: Constipation: How to Diagnose and Treat It Effectively
Steroid Use and Side Effects
Corticosteroids, are frequently used to manage cerebral edema and reduce intracranial pressure in GBM patients. However, long-term steroid use can lead to significant side effects, including:
- Cushing’s syndrome
- Hyperglycemia
- Osteoporosis
- Immunosuppression
- Psychiatric disturbances
To minimize these side effects, steroids should be used at the lowest effective dose for the shortest duration possible. Patients should be closely monitored for adverse effects, and prophylactic measures, such as gastric protection and bone density monitoring, should be implemented as needed.
Quality of Life Considerations
GBM and its treatment can have a profound impact on a patient’s quality of life. Fatigue, cognitive deficits, depression, and changes in personality and behavior are common issues that patients and their caregivers face. Supportive care interventions, such as psychosocial support, cognitive rehabilitation, and exercise programs, can help improve quality of life. Palliative care should be integrated early in the disease course to address symptoms, provide emotional support, and assist with advance care planning.
Conclusion
Glioblastoma presents a formidable challenge in the realm of brain cancer treatment. The complex biology of this aggressive tumor, coupled with its rapid growth and invasive nature, makes it particularly difficult to manage. Despite these hurdles, advancements in surgical techniques, radiation therapy, and chemotherapy have led to improvements in patient outcomes. The multimodal approach to treatment aims to maximize tumor control while preserving neurological function and quality of life.
Managing complications and side effects is crucial to ensure the best possible quality of life for GBM patients. From dealing with neurological deficits and seizures to managing the side effects of steroid use, a comprehensive approach is essential. Ongoing research and clinical trials continue to explore new therapies and treatment strategies, offering hope for enhanced outcomes in the future. While GBM remains a devastating diagnosis, the combined efforts of medical professionals, researchers, and supportive care teams provide a beacon of hope for patients and their families.