Understanding the signs your body sends when something is amiss is crucial, especially when it pertains to high blood sugar symptoms. Elevated blood sugar levels, or hyperglycemia, can lead to a host of complications if left unmanaged, directly impacting those with diabetes or at risk of developing type 2 diabetes. Recognizing these high blood sugar symptoms early on can be a significant step in preventing the adverse effects they may herald, underscoring the importance of being informed about how one’s body reacts to such conditions.
This article delves into the various manifestations of high blood sugar, starting from the early signs and symptoms to look out for, progressing through more advanced indicators. It will also explore the risk factors that increase the likelihood of experiencing high blood sugar, along with the underlying causes of these rises in glucose levels. Understanding the potential complications arising from persistent high blood sugar is pivotal in appreciating the importance of its management. Finally, the text will provide insight into preventive measures and how to manage high blood sugar effectively, emphasizing the role of lifestyle choices such as weight loss and dietary adjustments in maintaining healthy blood sugar levels.
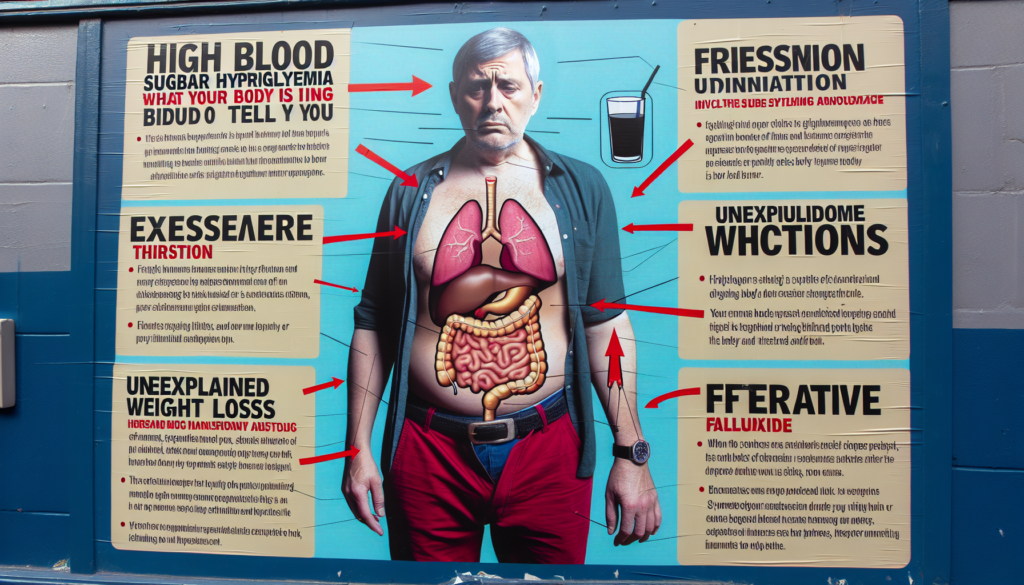
Early Signs and Symptoms of High Blood Sugar
Increased Thirst
One of the most common early indicators of high blood sugar is an increased sense of thirst. Individuals often experience a persistent dryness that is not easily quenched by drinking water. This symptom arises because the body attempts to dilute the high glucose levels in the blood, prompting an increased intake of fluids.
Frequent Urination
Closely linked to the increased thirst is the symptom of frequent urination. As individuals consume more liquids to satisfy their thirst, the kidneys are forced to work harder to filter and absorb the excess glucose. When they are unable to keep up, the surplus sugar is excreted through urine, leading to a higher frequency of urination.
Blurred Vision
Blurred vision is another early warning sign of elevated blood sugar levels. High glucose concentrations can cause the lens inside the eye to swell, altering its ability to focus. Initially, this symptom may be mild, but it can worsen if blood sugar levels remain uncontrolled. It’s important for individuals experiencing this symptom to monitor their blood sugar and consult with a healthcare provider to adjust their management plan if necessary.
Fatigue and Weakness
Experiencing an unusual degree of fatigue or weakness is a common symptom among those with high blood sugar. This occurs because the body is inefficient in using glucose for energy due to insulin resistance or lack of insulin production. Additionally, the frequent urination associated with high blood sugar can lead to dehydration, compounding feelings of tiredness.
By recognizing these early signs and symptoms, individuals can take swift action to manage their blood sugar levels, potentially preventing the progression to more severe health issues.
Advanced Symptoms of High Blood Sugar
Fruity-smelling Breath
One alarming sign of advanced high blood sugar is a fruity-smelling breath, often compared to the scent of nail polish remover. This symptom indicates the presence of ketones, which are toxic acids produced when the body begins to break down fat for energy due to insufficient insulin.
Dry Mouth
Individuals with high blood sugar levels may also experience a persistent dry mouth. This condition is not only uncomfortable but can also exacerbate other oral health issues, as saliva is essential for neutralizing acids and washing away food particles.
Abdominal Pain
Abdominal pain is another severe symptom associated with high blood sugar levels, particularly when it progresses to ketoacidosis. This discomfort can be sharp, dull, or cramping and is often accompanied by other gastrointestinal symptoms like nausea and vomiting.
Nausea and Vomiting
Nausea and vomiting are common when blood sugar levels become dangerously high. These symptoms are particularly concerning as they can lead to dehydration, further complicating the individual’s health status.
Shortness of Breath
Shortness of breath, or a feeling of being unable to catch one’s breath, is a critical symptom that requires immediate attention. This can occur when ketone levels are high, indicating that the body’s chemistry is severely imbalanced.
Confusion and Loss of Consciousness
High blood sugar can affect mental clarity, leading to confusion and, in severe cases, loss of consciousness. These symptoms are signs of diabetic ketoacidosis (DKA), a life-threatening condition that demands urgent medical intervention.
Recognizing these advanced symptoms is crucial for managing high blood sugar effectively and preventing the progression to more severe health complications. Prompt medical treatment is essential to address these dangerous symptoms and stabilize blood sugar levels.
Risk Factors for High Blood Sugar
Obesity
Obesity is a significant risk factor for high blood sugar and type 2 diabetes. Excess body fat, especially when concentrated around the abdomen, increases the body’s resistance to insulin. This resistance makes it difficult for the body to manage glucose levels effectively. Maintaining a healthy weight through diet and exercise can significantly reduce the risk of developing high blood sugar.
Physical Inactivity
A sedentary lifestyle is another critical risk factor for high blood sugar. Physical activity helps the body use glucose as energy and makes insulin more effective. Regular exercise, such as brisk walking or cycling, can improve insulin sensitivity and help manage or prevent high blood sugar levels.
Poor Dietary Choices
Consuming foods high in calories, fats, sugars, and processed carbohydrates can increase the risk of high blood sugar. These foods cause rapid spikes in glucose levels, which can be difficult to manage, especially in individuals with insulin resistance. A balanced diet rich in fiber, vitamins, and minerals is essential for maintaining stable blood sugar levels.
Medications Like Steroids
Certain medications, such as steroids, can raise blood sugar levels as a side effect. These drugs can interfere with the body’s ability to use insulin effectively, leading to temporary or prolonged increases in glucose levels. Individuals taking such medications should monitor their blood sugar levels closely and discuss potential alternatives with their healthcare provider if necessary.
Chronic Stress
Chronic stress triggers the body’s fight-or-flight response, releasing hormones that can raise blood sugar levels. Over time, persistent stress can make it difficult for the body to manage glucose effectively, contributing to higher blood sugar levels. Techniques such as mindfulness, meditation, and regular physical activity can help manage stress and its effects on blood sugar.
Pregnancy and Other Hormonal Changes
Pregnancy introduces hormonal changes that can affect insulin sensitivity, leading to gestational diabetes in some women. This condition usually resolves after childbirth but may increase the mother’s risk of developing type 2 diabetes later in life. Monitoring and managing blood sugar during pregnancy is crucial for the health of both the mother and the baby.
Causes of High Blood Sugar
Insufficient Insulin Production
Insufficient insulin production primarily occurs due to damage or diseases affecting the pancreas, the organ responsible for producing insulin. Conditions such as autoimmune diseases, chronic pancreatitis, pancreatic cancer, and cystic fibrosis can severely impair the pancreas’s ability to function normally. In these cases, the reduced production of insulin leads to inadequate control of blood glucose levels, resulting in hyperglycemia.
Insulin Resistance
Insulin resistance is a condition where muscle, fat, and liver cells do not respond effectively to insulin, preventing glucose from entering these cells and causing elevated blood glucose levels. Several factors contribute to insulin resistance, including genetic predisposition, obesity—particularly excess fat around the abdomen—and physical inactivity. Hormonal disorders like Cushing’s syndrome, acromegaly, and hypothyroidism can also induce insulin resistance, as can certain medications and inherited genetic conditions such as myotonic dystrophy and inherited lipodystrophy.
Pancreatic Diseases
Pancreatic diseases disrupt the pancreas’s ability to produce sufficient insulin, crucial for regulating blood sugar. Autoimmune disorders can attack and destroy pancreatic cells, while chronic pancreatitis leads to a gradual deterioration of pancreatic function. Additionally, pancreatic cancer and cystic fibrosis can damage the insulin-producing cells, further contributing to high blood sugar levels. It is noteworthy that individuals with type 2 diabetes have an increased risk of developing pancreatic cancer, potentially creating a reciprocal relationship between these two conditions.
Acute Physical or Emotional Stress
Acute stress, whether physical or emotional, can temporarily raise blood glucose levels. This response involves the release of stress hormones like cortisol and epinephrine, which promote glucose production by the liver and reduce the effectiveness of insulin. Situations such as illness, surgery, injury, or severe emotional distress can trigger this response, leading to transient episodes of hyperglycemia. In the long term, chronic stress can lead to sustained high blood sugar levels, contributing to the development of insulin resistance and type 2 diabetes.
By understanding these causes of high blood sugar, individuals can better manage their conditions through targeted treatments and lifestyle adjustments, aiming to maintain stable blood glucose levels and prevent the complications associated with hyperglycemia.
Complications from High Blood Sugar
Cardiovascular Diseases
High blood sugar is a significant risk factor for cardiovascular diseases, including heart attacks and strokes. It can lead to the narrowing of blood vessels and increase in cholesterol levels, which heightens the risk of coronary artery disease and peripheral arterial disease. These conditions can significantly accelerate in individuals with diabetes, leading to severe cardiovascular issues.
Neuropathy
Neuropathy, or nerve damage, is commonly induced by elevated blood sugar levels, affecting various nerves in the body. This includes peripheral neuropathy which impacts the extremities, causing symptoms like pain, tingling, and numbness. Cardiac autonomic neuropathy is another serious complication, increasing the risk of cardiovascular mortality and manifesting symptoms such as resting tachycardia and silent myocardial infarctions.
Kidney Damage
Chronic high blood sugar can lead to kidney damage, also known as diabetic nephropathy, which is one of the leading causes of kidney disease. This condition results from the damage to the blood vessels in the kidneys, making it difficult for them to filter waste effectively. Over time, this can progress to kidney failure, necessitating dialysis or a kidney transplant.
Retinopathy
Diabetic retinopathy occurs when high blood sugar levels damage the blood vessels in the retina. Initially, this may cause mild vision problems, but can escalate to severe vision loss or blindness. The condition often progresses silently and can suddenly manifest with significant symptoms, underscoring the importance of regular eye checks.
Foot Problems
High blood sugar levels can lead to severe foot complications, including ulcers and infections, which may result in amputation if not properly managed. This is due to a combination of neuropathy, which reduces sensation in the feet, and poor blood circulation that impedes healing.
Bone and Joint Issues
Individuals with high blood sugar are at an increased risk for bone and joint problems, such as osteoporosis. The metabolic imbalances caused by high glucose levels can lead to decreased bone density and joint deterioration, complicating mobility and quality of life.
Dental Issues
Dental health is significantly impacted by high blood sugar, which increases the risk of periodontal gum disease, cavities, and other oral health issues. Elevated glucose levels in saliva promote the growth of harmful bacteria, leading to plaque formation and gum disease, which can advance to tooth loss if not addressed.
Managing blood sugar levels is crucial in preventing these complications and requires a comprehensive approach including regular monitoring, lifestyle changes, and medical intervention.
Preventing and Managing High Blood Sugar
Consistent Medication Use
Managing high blood sugar effectively often requires the use of medications, especially for individuals with type 2 diabetes. It is crucial for patients to adhere to their prescribed medication schedules to maintain optimal blood glucose levels. Suboptimal adherence can lead to poor glycemic control, increasing the risk of diabetes complications and associated healthcare costs. Patients should consult with healthcare providers to ensure that the timing and dosage of their medications are appropriately aligned with their daily routines and meal plans.
Following a Diabetes Meal Plan
Diet plays a pivotal role in managing high blood sugar. A diabetes meal plan typically focuses on balancing nutrient intake, particularly carbohydrates, to prevent spikes in blood sugar levels. Techniques such as carbohydrate counting and using the plate method can help individuals make informed choices about their meals. Incorporating a variety of fiber-rich foods, such as fruits, vegetables, and whole grains, is recommended as these help slow down the digestion of carbohydrates and stabilize blood sugar levels.
Regular Physical Activity
Physical activity is essential for blood sugar management. Regular exercise helps increase insulin sensitivity, which means the body can use the available sugar in the bloodstream more effectively. For most adults, it is advisable to engage in at least 150 minutes of moderate aerobic activity per week, along with strength-building exercises a few times a week. Activities such as brisk walking, swimming, and cycling are beneficial. It is important for individuals to monitor their blood sugar levels before, during, and after exercise to prevent hypoglycemia, especially if they are on insulin therapy.
Blood Sugar Monitoring
Regular monitoring of blood glucose levels is a cornerstone of diabetes management. It allows individuals to understand how their lifestyle choices and medications affect their blood sugar levels. For people using insulin, frequent monitoring is crucial and can guide adjustments in dosage. Even for those not on insulin, occasional monitoring can provide valuable insights, especially when paired with diabetes education and support.
Healthy Lifestyle Choices
In addition to specific diabetes management strategies, general healthy lifestyle choices play a significant role in controlling high blood sugar. These include maintaining a moderate weight, staying hydrated, managing stress through relaxation techniques, and ensuring adequate sleep. Each of these factors has a direct impact on blood sugar levels and overall health. For instance, adequate hydration helps the kidneys flush out excess sugar through urine, and managing stress can prevent the blood sugar spikes that stress hormones often cause.
By integrating these strategies into daily life, individuals can effectively manage their high blood sugar levels and reduce the risk of developing the serious health complications associated with diabetes.
Conclusion
Through a comprehensive exploration of hyperglycemia, this article has highlighted the crucial signs and symptoms that signal elevated blood sugar levels, shedding light on the potential risks and underlying causes. Understanding these indicators is vital for early intervention, which can significantly reduce the risk of progressing to more severe complications. By recognizing both the early and advanced symptoms, individuals can take proactive steps towards managing their condition, underscoring the importance of being attuned to one’s body and its signals related to high blood sugar.
The discussion further extended into actionable strategies for preventing and managing high blood sugar, emphasizing the role of lifestyle choices, regular monitoring, and medication adherence. This holistic approach not only aids in stabilizing blood sugar levels but also contributes to a broader understanding of managing diabetes effectively. In essence, the journey towards managing hyperglycemia underscores a commitment to informed health choices, regular medical consultation, and an active lifestyle, offering a pathway to improved health outcomes and a better quality of life.
FAQs
1. How does the body manage elevated blood sugar levels? When blood sugar levels increase, the body’s pancreas releases insulin. This hormone helps open up cells to allow glucose to enter, providing them with the necessary energy to function. Any excess glucose is then stored in the liver and muscles for future use.
2. What are common symptoms of high blood sugar (hyperglycemia)? Individuals with hyperglycemia may experience several symptoms, including increased thirst, dry mouth, frequent urination, fatigue, blurred vision, unintentional weight loss, and recurrent infections such as thrush, bladder infections (cystitis), and skin infections.
3. What happens in the body when glucose levels are too high? In response to high glucose levels, the pancreas secretes insulin. This hormone encourages cells to take in glucose for energy or storage, which helps lower glucose levels in the blood.
4. What blood sugar level is considered harmful? Blood sugar levels exceeding 140 mg/dL in hospitalized patients are considered hyperglycemic and can cause complications like nosocomial infections and cardiovascular events. However, guidelines generally advise keeping blood glucose levels between 140-180 mg/dL to manage these risks effectively.