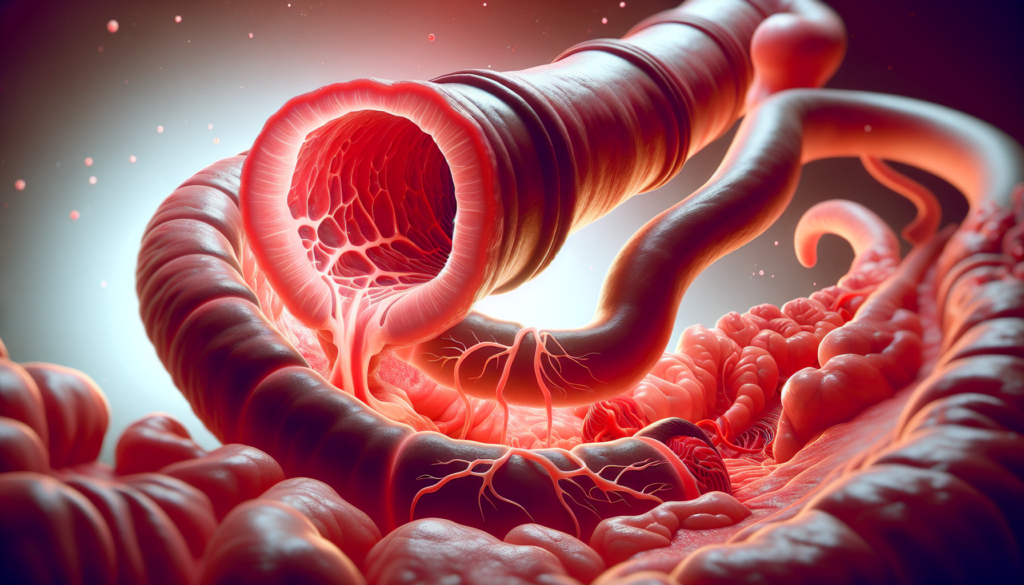
Esophagitis is a condition that causes inflammation and irritation of the esophagus, the tube connecting the throat to the stomach. This uncomfortable and potentially serious condition can have a significant impact on a person’s quality of life, affecting their ability to eat and drink comfortably. Understanding esophagitis is crucial for those experiencing symptoms or at risk of developing this condition.
This guide aims to provide a comprehensive overview of esophagitis, covering its various types, causes, and symptoms. It will explore the steps involved in diagnosing the condition, from initial symptoms to medical tests. The article will also delve into different treatment approaches, depending on the underlying cause of esophagitis. Finally, it will offer practical advice on prevention strategies to help reduce the risk of developing this condition.
The Impact of Esophagitis on Health
Esophagitis can have a significant impact on an individual’s health, affecting their quality of life in both the short and long term. The inflammation and irritation of the esophageal lining caused by esophagitis can lead to a range of symptoms that disrupt daily activities and cause discomfort.
In the short term, esophagitis can cause chest pain, difficulty swallowing, and painful swallowing. These symptoms can make it challenging for individuals to eat and drink comfortably, leading to reduced food intake and potential nutritional deficiencies. The constant discomfort and pain associated with esophagitis can also interfere with sleep, leading to fatigue and decreased overall well-being.
RELATED: Cytomegalovirus (CMV) Explained: What You Need to Know
If left untreated, esophagitis can lead to long-term complications that further impact health. Chronic inflammation of the esophagus can result in the formation of strictures, which are narrowed areas of the esophagus that make swallowing difficult. In some cases, ulcers may develop in the esophagus, causing bleeding and increasing the risk of infection. Scarring of the esophageal tissue can also occur, leading to a condition called Barrett’s esophagus, which is a precursor to esophageal cancer.
The impact of esophagitis extends beyond physical symptoms, affecting an individual’s quality of life. The discomfort and pain associated with the condition can lead to anxiety and depression, as individuals may feel limited in their ability to enjoy meals and social gatherings. The need for long-term management and lifestyle changes can also be stressful, impacting mental health and overall well-being.
In conclusion, esophagitis has a significant impact on an individual’s health, both in the short and long term. By understanding the potential consequences of the condition and seeking appropriate treatment, individuals can manage their symptoms, prevent complications, and maintain a better quality of life.
Diagnosing Esophagitis: A Step-by-Step Guide
Diagnosing esophagitis involves a combination of clinical assessment, endoscopic evaluation, and histopathologic analysis. Because no single symptom, endoscopic finding, or histologic feature is pathognomonic for esophagitis, the entire clinical picture must be considered to make an accurate diagnosis.
The diagnostic process begins with an initial assessment of the patient’s symptoms and medical history. Common symptoms that may suggest esophagitis include dysphagia, chest pain, heartburn, and regurgitation. The presence of concomitant atopic diseases, such as asthma or allergic rhinitis, can also provide clues to the underlying cause of esophagitis.
If esophagitis is suspected based on the initial assessment, the next step is to perform diagnostic tests. Esophagogastroduodenoscopy (EGD) is the gold standard for visualizing the esophagus and obtaining biopsies. During EGD, the endoscopist looks for characteristic findings such as esophageal rings, furrows, white plaques, and mucosal fragility. However, these endoscopic features are not specific to esophagitis and can be seen in other conditions as well.
Esophageal biopsies are essential for confirming the diagnosis of esophagitis and determining the underlying cause. Current guidelines recommend obtaining at least 2-4 biopsies from both the distal and proximal esophagus to maximize diagnostic sensitivity. The biopsies are then examined microscopically for the presence of eosinophils, which are the hallmark of eosinophilic esophagitis (EoE). A peak count of ≥15 eosinophils per high-power field is considered diagnostic for EoE, with few exceptions.
Interpreting the results of the diagnostic tests requires careful consideration of the clinical context. The finding of esophageal eosinophilia on biopsy does not, in and of itself, establish a diagnosis of EoE. Other possible causes of esophageal eosinophilia, such as gastroesophageal reflux disease (GERD) and proton pump inhibitor-responsive esophageal eosinophilia (PPI-REE), must be excluded. This is typically done by treating the patient with a high-dose proton pump inhibitor (PPI) for 8 weeks and repeating the endoscopy with biopsies. If the symptoms and esophageal eosinophilia persist despite PPI therapy, then the diagnosis of EoE can be confirmed.
In summary, diagnosing esophagitis is a multi-step process that involves integrating clinical, endoscopic, and histopathologic data. A systematic approach, as outlined in the current diagnostic guidelines, is essential for accurately identifying the underlying cause of esophagitis and guiding appropriate management.
Treatment Approaches for Different Types of Esophagitis
The treatment approach for esophagitis varies depending on the underlying cause. Reflux esophagitis is often managed with a combination of lifestyle changes, medications such as proton pump inhibitors (PPIs), and in some cases, surgery. PPIs work by reducing acid secretion in the stomach, allowing the esophageal mucosa to heal.
For eosinophilic esophagitis (EoE), treatment involves dietary modifications, topical corticosteroids, and dilation when strictures develop. Specialized diets, such as the six-food elimination diet (SFED) or elemental diet, can help identify and eliminate food triggers. Topical corticosteroids, like fluticasone or budesonide, reduce esophageal inflammation. Dilation is used as an adjunctive therapy to improve esophageal diameter and reduce dysphagia and food impactions.
RELATED: What You Need to Know About Cyanosis: Symptoms and Solutions
Drug-induced esophagitis management involves discontinuing the culprit medication and providing supportive care. Short-term treatment with PPIs and antacids can help alleviate symptoms and promote healing. Patients should be advised to take medications with an adequate amount of water and avoid lying down immediately after taking pills.
In cases of refractory esophagitis, a thorough review of the diagnosis and treatment adherence is necessary. Novel monoclonal antibody therapies targeting inflammatory mediators are being investigated for refractory EoE, but their role in clinical practice is not yet established.
Regardless of the type of esophagitis, the goal of treatment is to reduce inflammation, alleviate symptoms, and prevent complications such as strictures or Barrett’s esophagus. A multidisciplinary approach involving gastroenterologists, allergists, and nutritionists is often required for optimal management of esophagitis.
Prevention Strategies for Esophagitis
Preventing esophagitis involves a combination of dietary modifications, lifestyle changes, and proper medication management. By adopting these strategies, individuals can reduce their risk of developing esophagitis or prevent the condition from recurring.
Dietary Guidelines
Dietary changes play a crucial role in preventing esophagitis. Individuals should avoid trigger foods that can exacerbate symptoms, such as chocolate, coffee, fried foods, peppermint, spicy foods, and carbonated beverages. Keeping a food diary can help identify personal trigger foods. Eating smaller, more frequent meals throughout the day instead of large meals can promote digestion and prevent heartburn. Additionally, avoiding lying down for at least two hours after a meal or drinking acidic beverages can help prevent stomach contents from flowing back into the esophagus.
Lifestyle Recommendations
Several lifestyle modifications can help prevent esophagitis. Elevating the head while sleeping, using an extra pillow or two, can prevent reflux. Wearing loose-fitting clothes can ease pressure on the stomach, which can worsen heartburn and reflux. Quitting smoking is essential, as smoking can increase stomach acid production, reduce lower esophageal sphincter function, and decrease saliva, which neutralizes acid. Maintaining a healthy weight and reducing excess weight around the midsection can ease pressure on the stomach and prevent stomach contents from backing up into the esophagus.
RELATED: Managing Benign Prostatic Hyperplasia: Key Symptoms and Treatments
Medication Management
Proper medication management is crucial for preventing drug-induced esophagitis. Patients should take medications with an adequate amount of water (at least 200-250 ml) and remain in an upright position for at least 30 minutes after taking the medication. If possible, medications should be taken in liquid form to reduce the risk of pill-induced esophageal injury. Patients should also avoid taking medications just before bedtime. If a medication is known to cause esophageal irritation, patients should discuss alternative options with their healthcare provider.
By following these dietary guidelines, lifestyle recommendations, and medication management strategies, individuals can significantly reduce their risk of developing esophagitis or prevent the condition from recurring. If symptoms persist despite these preventive measures, it is essential to consult a healthcare provider for further evaluation and treatment.
Conclusion
Esophagitis has a significant impact on a person’s well-being, affecting their ability to eat comfortably and enjoy daily activities. This guide has explored the various types of esophagitis, their causes, and symptoms, as well as the steps involved in diagnosing and treating this condition. By understanding the underlying factors and following appropriate treatment approaches, individuals can effectively manage their symptoms and prevent complications.
To wrap up, the key to dealing with esophagitis lies in early detection, proper diagnosis, and tailored treatment plans. By adopting healthy lifestyle habits, making dietary changes, and following medication guidelines, individuals can reduce their risk of developing esophagitis or prevent its recurrence. Remember, if symptoms persist despite preventive measures, it’s crucial to seek medical advice for further evaluation and personalized care.