Bursitis is a common yet often misunderstood condition that affects millions of people worldwide. This painful inflammation of the small, fluid-filled sacs called bursae can occur in various joints throughout the body, causing discomfort and limiting mobility. As these cushioning structures play a key role in reducing friction between bones, tendons, and muscles, their inflammation can have a significant impact on daily activities and quality of life.
Understanding bursitis is crucial for early detection, effective treatment, and prevention of recurrence. This article aims to shed light on the different types of bursitis, their symptoms, and how to tell them apart from other conditions. It will also explore various treatment approaches, from conservative methods to medical interventions, and provide insights on long-term management strategies to help individuals cope with and minimize the effects of this bothersome condition.
Types of Bursitis and Their Symptoms




Bursitis can develop in various joints throughout the body, with each type presenting its own set of symptoms. The most common types of bursitis include:
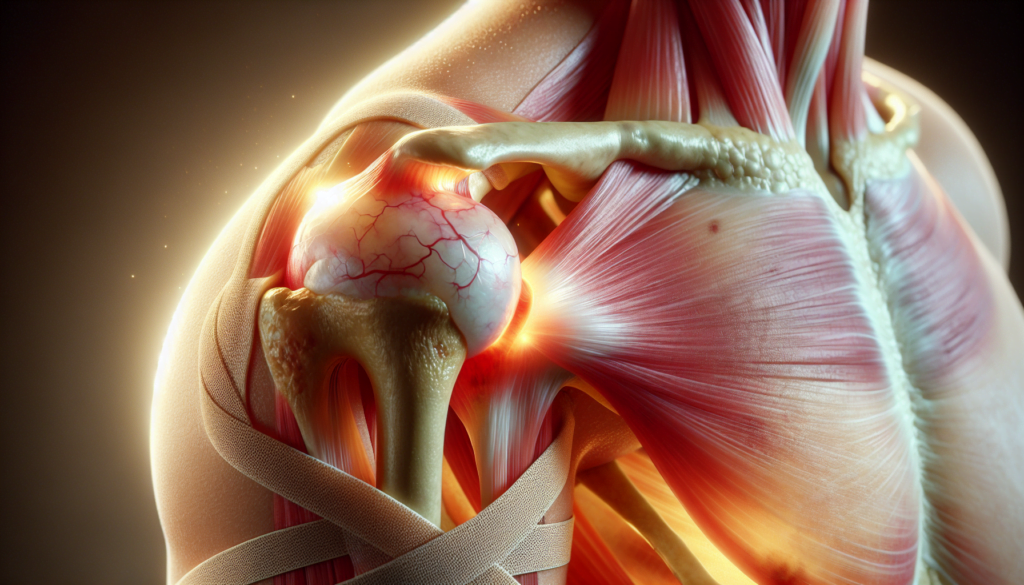
Shoulder Bursitis
Shoulder bursitis, also known as subacromial bursitis, affects the bursa located between the rotator cuff tendons and the acromion (the highest point of the shoulder blade). Symptoms of shoulder bursitis include:
- Pain and swelling in the shoulder
- Stiffness or limited range of motion
- Nighttime pain when lying on the affected side
- Sharp or pinching pain with overhead shoulder motions
RELATED: Irritable Bowel Syndrome (IBS): Causes, Symptoms, and Treatment Options
Hip Bursitis
Hip bursitis can occur in two main bursae: the trochanteric bursa, located on the outside of the hip, and the iliopsoas bursa, situated on the inside (groin side) of the hip. Trochanteric bursitis is more common and causes pain on the outside of the hip and outer thigh. Iliopsoas bursitis, although less common, results in pain in the groin or upper buttock area.
Knee Bursitis
Knee bursitis, particularly prepatellar bursitis, affects the bursa located in front of the kneecap (patella). This condition is often referred to as “housemaid’s knee,” “carpet layer’s knee,” or “coal miner’s knee” due to its association with frequent kneeling. Symptoms include:
- Swelling at the front of the knee
- Pain or tenderness when kneeling or bending the knee
- Redness and warmth in the affected area (if caused by an infection)
Elbow Bursitis
Elbow bursitis, or olecranon bursitis, involves inflammation of the bursa at the bony tip of the elbow (olecranon). Symptoms of elbow bursitis include:
- Swelling at the back of the elbow
- Pain and tenderness, especially when bending the elbow or applying pressure
- Redness and warmth (if caused by an infection)
Heel Bursitis
Heel bursitis, also known as retrocalcaneal bursitis, affects the bursa located between the Achilles tendon and the heel bone (calcaneus). Symptoms of heel bursitis include:
- Pain and swelling at the back of the heel
- Tenderness when touching the affected area
- Increased pain when standing on toes or wearing shoes that put pressure on the heel
In some cases, bursitis can be caused by an infection (septic bursitis), leading to additional symptoms such as fever, chills, and general feelings of being unwell. Septic bursitis requires prompt medical attention and treatment with antibiotics to prevent the spread of infection.
Differentiating Bursitis from Other Conditions
Bursitis shares similarities with other joint conditions, making it challenging to distinguish without medical expertise. The primary difference between bursitis and arthritis is that bursitis affects the bursae, while arthritis impacts the bones and cartilage of the joints. Bursitis is typically acute and resolves within a few weeks, whereas arthritis is a chronic, progressive condition.
Arthritis vs. bursitis
Although both conditions cause joint pain, stiffness, and swelling, they affect different structures. Arthritis attacks the cartilage and bones, while bursitis involves inflammation of the bursae. Arthritis appears gradually and worsens over time, while bursitis may appear suddenly after an injury or intense activity.
To diagnose the cause of joint pain, a doctor will evaluate the location, severity, and duration of symptoms. X-rays or MRIs may be ordered to confirm arthritis, while an ultrasonogram or injection can help identify bursitis.
Tendinitis vs. bursitis
Tendinitis, another condition causing joint pain, affects the tendons that connect muscles to bones. Like bursitis, tendinitis is often caused by repetitive motions or overuse. However, tendinitis pain is typically more localized to the affected tendon, while bursitis pain may be more diffuse around the joint.
RELATED: Ingrown Toenails: Common Symptoms and How to Address Them
Other joint-related conditions
Other conditions that can cause joint pain include gout, a type of arthritis caused by uric acid buildup, and septic arthritis, which results from a joint infection. A thorough medical evaluation is essential to accurately diagnose the cause of joint pain and develop an appropriate treatment plan.
Bursitis Treatment Approaches
The treatment of bursitis aims to reduce inflammation, alleviate pain, and restore joint function. A combination of non-surgical and surgical options may be considered, depending on the severity and persistence of symptoms.
Non-surgical treatments are often the first line of defense against bursitis. These include rest, ice application, and compression to reduce swelling and discomfort. Modifying activities that aggravate the condition and using assistive devices like crutches or braces can help minimize stress on the affected joint.
Medications and injections play a crucial role in managing bursitis symptoms. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and pain. In more severe cases, corticosteroid injections directly into the bursa may be recommended to provide rapid relief. However, repeated injections should be avoided, as they can weaken tendons and increase the risk of complications.
Physical therapy is an essential component of bursitis treatment. A physical therapist can develop a personalized exercise program to strengthen the muscles surrounding the affected joint, improve flexibility, and promote proper body mechanics. Techniques such as ultrasound therapy, electrical stimulation, and manual therapy may also be employed to enhance healing and reduce pain.
Surgical options are typically reserved for cases where conservative treatments have failed to provide adequate relief or when the bursa is severely damaged. Surgical procedures may involve draining excess fluid from the bursa or removing the inflamed bursa altogether. In rare instances, tendon repair surgery may be necessary if the condition has led to a torn or ruptured tendon. Postoperative rehabilitation is crucial to ensure a successful recovery and prevent future recurrences of bursitis.
Long-term Management of Bursitis
Long-term management of bursitis involves a combination of lifestyle adjustments, ongoing exercises and stretches, regular check-ups, and strategies to prevent recurrence. Individuals with bursitis should modify their daily activities to avoid or reduce repetitive motions and prolonged pressure on the affected joint. This may involve using ergonomic equipment, taking frequent breaks, and maintaining proper posture.
Incorporating a regular exercise routine that focuses on stretching and strengthening the muscles surrounding the affected joint can help improve flexibility, reduce stiffness, and prevent future flare-ups. Low-impact activities such as swimming, cycling, and yoga are often recommended for individuals with bursitis. Physical therapists can develop personalized exercise programs tailored to the individual’s specific needs and goals.
RELATED: High Blood Pressure: Complete Guide to Prevention and Care
Scheduling regular check-ups with a healthcare provider is essential for monitoring the condition and making necessary adjustments to the treatment plan. During these visits, the provider may assess the individual’s range of motion, pain levels, and overall progress. They may also recommend additional therapies, such as massage or acupuncture, to complement the existing treatment regimen.
To prevent recurrence of bursitis, individuals should maintain a healthy weight, as excess weight can put additional stress on the joints. Wearing appropriate footwear and using protective gear, such as knee pads or elbow pads, can help reduce the risk of developing bursitis in vulnerable areas. Additionally, gradually increasing the intensity and duration of physical activities, rather than suddenly engaging in strenuous exercises, can help prevent overuse injuries that may lead to bursitis.
Conclusion
Bursitis is a challenging condition that has a significant impact on joint health and overall well-being. Understanding its symptoms, causes, and treatment options is key to managing this painful inflammation effectively. By adopting a multifaceted approach that includes rest, medication, physical therapy, and lifestyle changes, individuals can alleviate discomfort and improve their quality of life. Regular check-ups and personalized care plans are crucial to monitor progress and make necessary adjustments.
Looking ahead, preventing bursitis recurrence is just as important as treating its immediate symptoms. This involves making smart choices in daily activities, maintaining a healthy weight, and sticking to a regular exercise routine that strengthens the muscles around vulnerable joints. By staying proactive and informed, those dealing with bursitis can take control of their joint health and minimize the condition’s impact on their lives. Remember, with the right approach and support, managing bursitis is not just possible but can lead to long-term relief and improved joint fun