Neurofibromatosis is a complex genetic disorder that affects the nervous system, causing tumors to grow on nerves throughout the body. This condition can lead to a wide range of symptoms and complications, impacting the lives of those affected in various ways. While relatively rare, neurofibromatosis has gained increased attention in recent years due to advancements in genetic research and improved diagnostic techniques.
This article delves into the intricate world of neurofibromatosis, exploring its genetic foundations and the process of tumor development. It examines the different diagnostic approaches used to identify the condition and discusses current treatment strategies available to manage symptoms and improve quality of life. By shedding light on this often misunderstood disorder, we aim to provide a comprehensive overview of neurofibromatosis, its implications, and the ongoing efforts to enhance patient care.
Genetic Foundations of Neurofibromatosis


Neurofibromatosis has a strong genetic basis, with mutations in specific genes leading to the development of the disorder. The two main types of neurofibromatosis, NF1 and NF2, are caused by alterations in different genes.
NF1 Gene Mutation
NF1 results from mutations in the NF1 gene located on chromosome 17q11.2. This gene encodes a protein called neurofibromin, which acts as a tumor suppressor by regulating cell growth and division. Mutations in the NF1 gene lead to the production of non-functional neurofibromin, allowing cells to grow and divide uncontrollably, forming tumors such as neurofibromas.
Over 1,000 different pathogenic variants of the NF1 gene have been identified, including stop mutations, amino acid substitutions, insertions, deletions, and gross chromosomal rearrangements. Most variants involve sizable truncation of neurofibromin, often due to alteration of messenger ribonucleic acid (mRNA) splicing.
NF2 Gene Mutation
NF2 is caused by mutations in the NF2 gene located on chromosome 22q12.2. This gene codes for a protein called merlin (moesin-ezrin-radixin-like protein) or schwannomin, which is essential for regulating contact-dependent inhibition of cellular proliferation. Merlin functions at the cell-cell adhesion interface, in transmembrane signaling, and in the actin cytoskeleton.
About 90% of NF2 gene mutations result in a compromised protein product, leading to non-functional merlin that cannot prevent tumor growth, particularly in Schwann cells. This results in the development of vestibular schwannomas, the most common benign tumors diagnosed in individuals with NF2.
RELATED: Effective Treatments for Insomnia: What You Need to Know
Inheritance Patterns
Both NF1 and NF2 follow an autosomal dominant inheritance pattern, meaning that only one copy of the mutated gene is required for an individual to be affected. Descendants of an affected individual have a 50% risk of inheriting the altered gene. However, the phenotype of individuals with NF1 or NF2 can be highly variable, even among genetically related family members.
In approximately 50% of cases, NF1 and NF2 result from de novo mutations, occurring for the first time in an individual with no family history of the disorder. The NF1 gene locus has a higher spontaneous mutation rate compared to most other gene loci, which may account for the observed de novo cases.
Understanding the genetic foundations of neurofibromatosis is crucial for developing targeted therapies and personalized healthcare approaches for affected individuals. As research continues to unravel the complexities of these genetic alterations, new avenues for diagnosis, prognosis, and treatment may emerge.
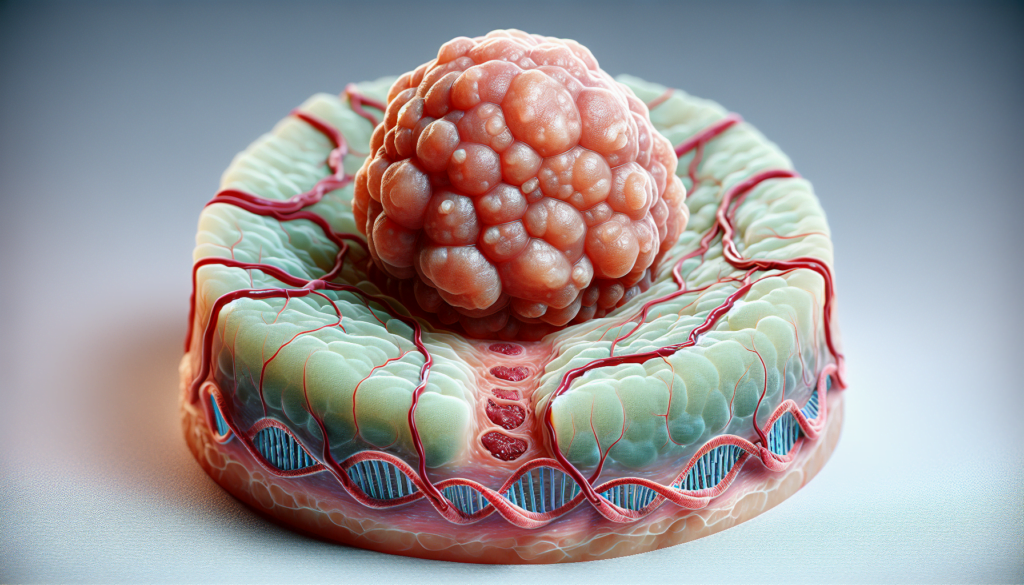
Tumor Development in Neurofibromatosis
Neurofibromatosis has a strong influence on tumor development in the nervous system. Individuals with neurofibromatosis type 1 (NF1) are prone to developing neurofibromas, while those with neurofibromatosis type 2 (NF2) are more likely to develop schwannomas. The tumor suppressor genes NF1 and NF2 play crucial roles in regulating cell growth and differentiation, and mutations in these genes lead to uncontrolled cell proliferation and tumor formation.
Neurofibromas
Neurofibromas are the hallmark tumors of NF1. They are benign tumors that arise from the cells and tissues surrounding nerves, including Schwann cells, fibroblasts, and other cell types. Neurofibromas can grow in various locations, such as the skin, under the skin, or deeper in the body. Plexiform neurofibromas are a specific subtype that involves multiple nerve branches and can cause significant morbidity due to their size and location. Although most neurofibromas are benign, they have the potential to transform into malignant peripheral nerve sheath tumors (MPNSTs) in a small percentage of cases.
Schwannomas
Schwannomas are the characteristic tumors associated with NF2. These benign tumors originate from Schwann cells, which are the cells that provide insulation for nerves. In NF2, schwannomas commonly develop on the vestibular nerve, leading to hearing loss and balance problems. However, schwannomas can also occur on other cranial and peripheral nerves throughout the body. Unlike neurofibromas, schwannomas in NF2 rarely undergo malignant transformation.
RELATED: Hidradenitis Suppurativa: Complete Overview and Treatment Options
Other Associated Tumors
In addition to neurofibromas and schwannomas, individuals with neurofibromatosis are at an increased risk of developing other types of tumors. These include:
- Optic pathway gliomas: Low-grade gliomas that affect the optic nerve and can cause visual impairment.
- Meningiomas: Tumors that arise from the meninges, the protective membranes covering the brain and spinal cord.
- Ependymomas: Tumors that develop from the ependymal cells lining the ventricles of the brain and the central canal of the spinal cord.
- Malignant peripheral nerve sheath tumors (MPNSTs): Aggressive sarcomas that can arise from pre-existing plexiform neurofibromas in NF1.
Understanding the mechanisms of tumor development in neurofibromatosis is crucial for developing targeted therapies and improving patient outcomes. Ongoing research aims to elucidate the complex interplay between genetic mutations, cellular signaling pathways, and the tumor microenvironment in the pathogenesis of neurofibromatosis-associated tumors.
Diagnostic Approaches
Diagnosing neurofibromatosis involves a combination of clinical evaluation, imaging techniques, and genetic testing. The National Institutes of Health (NIH) have established diagnostic criteria for neurofibromatosis type 1 (NF1) based on the presence of specific clinical features. These criteria include six or more café-au-lait macules, two or more neurofibromas or one plexiform neurofibroma, freckling in the axillary or inguinal regions, optic pathway glioma, two or more Lisch nodules, a distinctive osseous lesion, and a first-degree relative with NF1.
Imaging techniques play a crucial role in identifying tumors associated with neurofibromatosis. Magnetic resonance imaging (MRI) is the preferred modality for detecting brain and spinal tumors, as it provides excellent contrast and multiplanar capabilities. MRI can visualize vestibular schwannomas, meningiomas, ependymomas, and spinal neurofibromas. Computed tomography (CT) scans may be used when MRI is contraindicated, and CT myelography can depict spinal tumors.
Genetic testing has become an essential tool in confirming the diagnosis of neurofibromatosis. Molecular testing for pathogenic variants in the NF1 gene is available, with a high detection rate of around 95% when using a comprehensive approach that includes dosage analysis and RNA-based sequencing. Identifying an NF1 pathogenic variant in an individual with clinical features of NF1 confirms the diagnosis. Genetic testing is also valuable for distinguishing NF1 from similar conditions, such as Legius syndrome, which is caused by pathogenic variants in the SPRED1 gene.
Treatment Strategies
The management of neurofibromatosis focuses on alleviating symptoms, enhancing mobility, and addressing aesthetic concerns. Medications play a crucial role in symptom management, primarily for pain relief, and can help control tumor growth, sometimes in combination with radiation therapy.
Surgical interventions are vital for managing neurofibromatosis, particularly in complex cases like plexiform neurofibromas and peripheral nerve sheath tumors. Surgical excision is often used to treat these tumors, especially if they cause chronic pain, show rapid growth, or are on peripheral nerves.
To manage neurofibromatosis-related skin conditions, treatments such as laser therapy can lessen the visibility of café-au-lait spots. Topical creams and ointments provide relief from skin discomfort. Routine skin care with gentle cleansers and moisturizers maintains skin health, while sun protection is crucial to prevent symptom aggravation.
RELATED: Fetal Alcohol Syndrome: A Complete Overview of Symptoms and Diagnosis
Pain management strategies for plexiform neurofibromas include medications for nerve pain. Non-surgical methods like radiation therapy are alternative options to reduce tumor size and ease symptoms, but they come with risks and side effects that should be thoroughly discussed with the healthcare provider.
Physical therapy can be pivotal in symptom management for neurofibromatosis. It helps improve muscle strength, coordination, and flexibility, which are often compromised by tumor growth on nerves. Physical therapy also offers pain relief and can lift the patient’s mood.
Selumetinib, an oral kinase inhibitor, has shown promising results in treating symptomatic, inoperable plexiform neurofibromas in patients with neurofibromatosis type 1 (NF1). It can result in durable tumor shrinkage and clinical benefit, making it a significant advancement in targeted therapies for NF1.
Conclusion
Neurofibromatosis has a significant impact on the lives of those affected, with its complex genetic foundations leading to tumor development and a range of symptoms. The advances in diagnostic approaches, including clinical evaluation, imaging techniques, and genetic testing, have improved our ability to identify and understand this condition. These developments have paved the way for more targeted treatment strategies, offering hope to patients and their families.
The ongoing research into neurofibromatosis continues to shed light on its mechanisms and potential therapies. From surgical interventions and pain management to promising new medications like selumetinib, the field is evolving to better address the needs of patients. As we move forward, the focus remains on improving quality of life, managing symptoms, and working towards more effective treatments for this challenging disorder.