Neurofibromatosis Type 1 (NF1) is a genetic disorder that affects about 1 in 3,000 people worldwide. This condition has an impact on the nervous system and causes tumors to grow on nerves throughout the body. NF1 can lead to a wide range of symptoms and complications, making it a complex and challenging disorder to manage for both patients and healthcare providers.
Understanding NF1 is crucial to improve the lives of those affected by this condition. This article aims to explore the key aspects of Neurofibromatosis Type 1, including its common symptoms, diagnostic methods, and available treatment options. By shedding light on these topics, we hope to provide valuable information to patients, families, and healthcare professionals dealing with NF1.
Understanding Neurofibromatosis Type 1
What is NF1?
Neurofibromatosis type 1 (NF1) is a genetic disorder that has an influence on the nervous system. It is caused by a mutation in the NF1 gene, which provides instructions to make a protein called neurofibromin. This protein acts as a tumor suppressor and is produced in many cells, including nerve cells and specialized cells surrounding nerves. When the NF1 gene is altered, it leads to the production of a nonfunctional version of neurofibromin that cannot regulate cell growth and division properly. As a result, tumors such as neurofibromas can form along nerves throughout the body.
Genetic Causes
NF1 follows an autosomal dominant pattern of inheritance, meaning that only one copy of the altered gene is needed to cause the disorder. In about half of the cases, the mutated gene is inherited from an affected parent. The remaining cases result from new mutations in the NF1 gene, occurring in people with no history of the disorder in their family. The NF1 gene is located on the long arm of chromosome 17 (17q11.2), and over 1000 pathogenic variants have been identified. These mutations can include stop mutations, amino acid substitutions, insertions, deletions, and gross chromosomal rearrangements.
RELATED: Black Mold Safety: Symptoms, Risks, and How to Manage
Inheritance Patterns
Since neurofibromatosis type 1 (NF1) is an autosomal dominant condition, an affected individual has a 50% chance of passing the altered gene to their offspring. The disorder is highly penetrant, meaning that almost all individuals with an NF1 gene mutation will present with some phenotypic traits of the syndrome. However, the expression of NF1 can vary widely, even within the same family, leading to different degrees of clinical severity. Genetic testing is available to confirm the presence of the NF1 gene mutation with 95% sensitivity and may be appropriate in some cases, especially for prenatal testing when there is an increased risk.
Common Symptoms and Signs of NF1
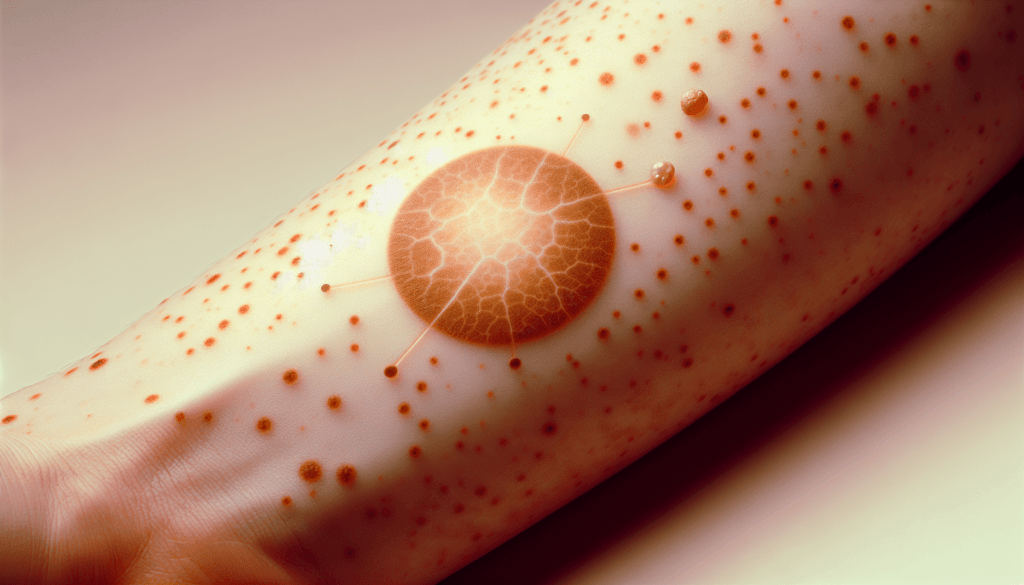
Café-au-lait spots are one of the most common signs of neurofibromatosis type 1 (NF1). These pigmented birthmarks appear as light to dark brown patches on the skin and are present in 99% of patients at birth or develop within the first two years of life. Multiple café-au-lait spots, especially more than six, are highly suggestive of NF1. The spots tend to darken with sun exposure and lighten with age, and they have a non-malignant potential.
Neurofibromas, benign tumors composed of neoplastic Schwann cells, mast cells, endothelial cells, and macrophages, are another hallmark of NF1. They are located along the nerves and can be cutaneous (superficial), subcutaneous (deeper), nodular plexiform, or diffuse plexiform. Neurofibromas usually become apparent after puberty and continue to increase in size and number throughout adulthood.
Lisch nodules, which are melanocytic hamartomas that appear as well-defined, dome-shaped elevations projecting from the surface of the iris, are clear to yellow or brown in color. Multiple Lisch nodules are found almost exclusively in patients with NF1 and are the most consistent feature of the condition in adults. A slit-lamp examination is required to distinguish them from other iris lesions.
Skeletal abnormalities are also relatively common in individuals with NF1, with up to 50% experiencing significant musculoskeletal manifestations. Scoliosis is the most frequent skeletal complication, affecting approximately 21% of NF1 patients. Other skeletal issues include bowing and pseudarthrosis, which are related to mesodermal dysplasia and commonly affect the tibia. These bone abnormalities can lead to fractures, deformities, and functional impairments.
Diagnosis and Testing for NF1
Clinical Criteria
The diagnosis of neurofibromatosis type 1 (NF1) is usually made based on clinical findings. The revised diagnostic criteria for NF1 incorporate new clinical features and genetic testing. An individual who does not have a parent diagnosed with NF1 meets the diagnostic criteria if they have two or more of the following: six or more café-au-lait macules, freckling in the axillary or inguinal regions, two or more neurofibromas or one plexiform neurofibroma, optic pathway glioma, two or more iris Lisch nodules or choroidal abnormalities, a distinctive osseous lesion, or a heterozygous pathogenic NF1 variant with a 50% variant allele fraction in normal tissue. A child of a parent who meets these criteria merits an NF1 diagnosis if they have one or more of the listed features.
RELATED: Adenomyosis: Identifying Symptoms and Exploring Treatment Plans
Genetic Testing
While NF1 is usually diagnosed clinically, genetic testing can be helpful in certain situations. Sequencing of the NF1 gene has a high detection rate, approaching 95% in clinically affected individuals. Molecular testing is particularly useful for younger patients with limited clinical findings who lack a positive family history. It can also help differentiate NF1 from conditions with overlapping features, such as Legius syndrome. Prenatal genetic diagnosis is possible through linkage analysis or direct sequencing if a specific familial mutation is known.
Imaging Studies
Imaging studies have a role in the diagnosis and management of NF1-related complications. MRI of the brain can detect optic pathway gliomas and T2 hyperintensities, which are common in NF1. It is also valuable for evaluating other internal lesions. CT or MRI is indicated when pheochromocytoma is suspected based on biochemical screening. Other imaging modalities, such as PET and scintigraphy, may be used in specific situations.
Treatment Options and Management
Monitoring and Surveillance
Neurofibromatosis type 1 (NF1) requires regular monitoring to detect potential complications early. Annual examinations should include blood pressure measurement, skin assessment for typical lesions, visual acuity check, eye examination for proptosis or strabismus, and spine and extremity evaluation for abnormalities. Neurologic evaluation should involve a careful history of headaches or motor/sensory symptoms and a comprehensive motor/sensory examination. Annual ophthalmologic exams are crucial for detecting optic nerve pallor, visual acuity changes, visual field defects, and Lisch nodules. Children with NF1 should undergo yearly neurologic exams and ophthalmologic evaluations up to age 10 to screen for optic gliomas. MRI of the brain may be recommended if concerns arise regarding vision or early puberty.
Surgical Interventions
Surgical management is the most effective method to control or even cure neurofibromas. For cutaneous neurofibromas, recent advances in laser technology have allowed nonsurgical removal of small lesions. However, careful surgical resection may leave a smaller, less prominent scar. Plexiform neurofibromas can be more challenging to remove due to their invasive growth and proximity to important structures. Preoperative embolization of the tumor’s nutrient arteries can effectively reduce intraoperative bleeding. Other surgical interventions may be necessary for skeletal abnormalities such as scoliosis and pseudarthrosis.
RELATED: Angioedema: What You Need to Know About Symptoms and Treatments
Medication Therapies
In 2020, the FDA approved selumetinib (Koselugo) for the treatment of symptomatic, inoperable plexiform neurofibromas in patients 2 years and older with NF1. This oral kinase inhibitor can result in durable tumor shrinkage with clinical benefit. Chemotherapy, especially with carboplatin and vincristine, has shown effectiveness in controlling the progression of optic nerve gliomas. Hypertension associated with NF1 should be promptly treated with medication. Epilepsy can be managed with anti-seizure medications to reduce the frequency of seizures.
Multidisciplinary Care
A multidisciplinary approach to care is essential for individuals with NF1, involving a dedicated team of specialists throughout the patient’s lifetime. This team may include neurologists, ophthalmologists, dermatologists, orthopedic surgeons, oncologists, and geneticists. Patients should be referred to specialized neurofibromatosis centers for comprehensive care and access to clinical trials. Psychological support, pain management, and educational interventions are also important aspects of multidisciplinary care for NF1 patients and their families.
Conclusion
Neurofibromatosis Type 1 (NF1) has a significant impact on the lives of those affected, presenting a range of challenges from physical symptoms to emotional and social hurdles. The complexity of this genetic disorder necessitates a comprehensive approach to care, involving regular monitoring, surgical interventions when needed, and emerging medication therapies. What’s more, the role of multidisciplinary teams in managing NF1 can’t be overstated, as they provide crucial support to patients throughout their lives.
Looking ahead, ongoing research and clinical trials offer hope for improved treatments and quality of life for individuals with NF1. As our understanding of the condition grows, so does the potential for more targeted therapies and better management strategies. To wrap up, while NF1 presents significant challenges, the combined efforts of medical professionals, researchers, and support networks continue to make strides in improving outcomes for those living with this complex disorder.