Parasites are unwelcome guests that can take up residence in the human body, causing a range of health issues. These microscopic organisms survive by feeding off their hosts, often leading to various symptoms and complications. From intestinal worms to blood-dwelling protozoa, parasites pose a significant threat to human health worldwide, affecting millions of people each year.
This article delves into the world of human parasites, exploring their causes, symptoms, and available treatment options. It sheds light on common types of parasites that infect humans, discusses risk factors for parasitic infections, and outlines the diagnostic methods used to identify these invaders. Additionally, it examines various treatment approaches to combat parasitic infections, empowering readers with knowledge to protect themselves and seek appropriate medical care when needed.
Common Types of Human Parasites



Human parasites can be classified into three main categories: protozoa, helminths, and ectoparasites. Each type has its unique characteristics and can cause various health issues.
Protozoa
Protozoa are single-celled organisms that can multiply within the human body. They can spread through contaminated food and water, person-to-person contact, and insect bites. Some common examples of protozoan parasites include:
- Plasmodium malariae: This parasite causes malaria infection.
- Cryptosporidium: This parasite is ingestible and can cause cryptosporidiosis.
RELATED: Molluscum Contagiosum: A Detailed Look at Symptoms and Solutions
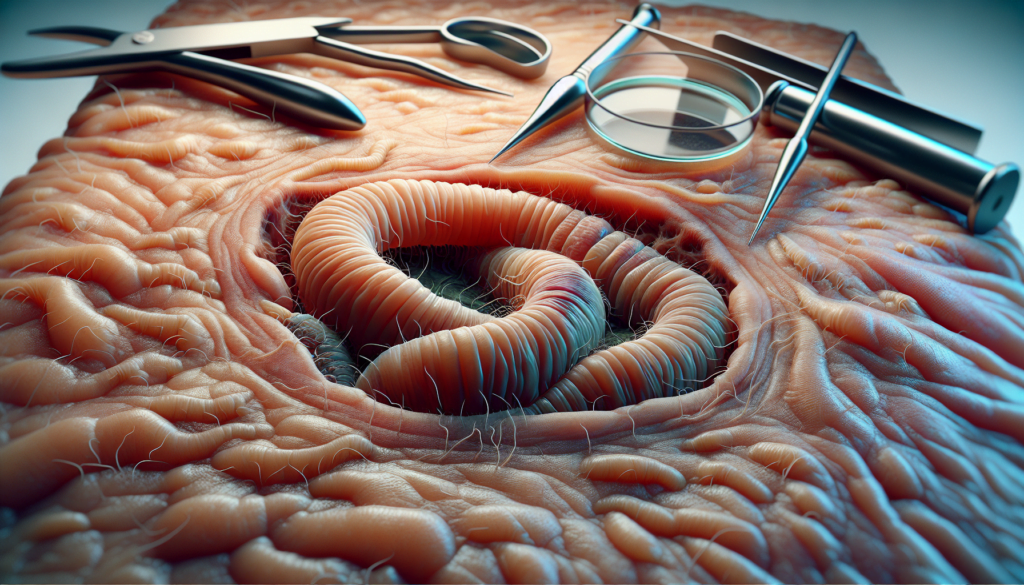
Helminths
Helminths are parasitic worms that often take up residence in a person’s digestive tract. Unlike protozoa, these parasites cannot multiply or divide within the human body and eventually pass through a person’s stool. Some common types of helminths include:
- Ascaris lumbricoides: This is a common roundworm that can infect the human intestines.
- Hookworm: These parasitic worms can cause hookworm infection, which can lead to anemia and other health issues.
Ectoparasites
Ectoparasites are small organisms that live on the outside of the human body. They can cause various skin irritations and allergic reactions. Some common examples of ectoparasites include:
- Ticks: These blood-sucking arachnids can transmit diseases like Lyme disease and Rocky Mountain spotted fever.
- Fleas: These small, wingless insects can cause itching and skin irritation, and can also transmit diseases like the plague.
- Lice: These tiny insects can infest the hair and skin, causing itching and irritation.
It’s important to note that the symptoms of parasitic infections can vary widely depending on the type of parasite involved. Some common symptoms may include skin rashes, weight loss, increased appetite, abdominal pain, diarrhea, vomiting, and general feelings of weakness and fatigue. However, in some cases, there may be no symptoms at all, making it difficult to detect the presence of a parasite without proper testing.
Causes and Risk Factors
Parasitic infections can be caused by a variety of factors, including contaminated food and water, poor hygiene practices, travel to endemic areas, and a weakened immune system.
Contaminated Food and Water
One of the primary causes of parasitic infections is consuming food or water contaminated with parasitic eggs or cysts. This can occur when:
- Eating raw or undercooked meat, fish, or aquatic plants
- Drinking water from contaminated sources, such as lakes or streams
- Consuming unwashed fruits and vegetables
- Ingesting unpasteurized milk or juices
Parasites can survive in contaminated food and water, and when consumed, they can establish an infection in the human body.
Poor Hygiene
Poor personal and environmental hygiene practices can also contribute to the spread of parasitic infections. Risk factors include:
- Not washing hands before eating or after using the bathroom
- Infrequent bathing or showering
- Lack of access to clean water and sanitation facilities
- Exposure to contaminated soil, especially when walking barefoot
Parasites can be transmitted from person to person through contaminated hands, surfaces, or objects.
Travel to Endemic Areas
Traveling to regions where parasitic infections are common can increase the risk of exposure. Some high-risk areas include:
- Rural or developing regions with poor sanitation
- Tropical and subtropical countries
- Areas with inadequate water treatment facilities
Travelers may be exposed to parasites through contaminated food, water, or insect bites.
RELATED: All About Moles: From Causes to Treatment Options
Weakened Immune System
Individuals with compromised immune systems are more susceptible to parasitic infections. This includes people who:
- Have HIV/AIDS
- Are undergoing cancer treatment
- Have received an organ transplant
- Take immunosuppressive medications
A weakened immune system may not be able to effectively fight off parasitic infections, leading to more severe symptoms and complications.
Symptoms of Parasitic Infections
The symptoms of parasitic infections can vary widely depending on the type of parasite involved. Some common symptoms may include gastrointestinal issues, systemic symptoms, and skin-related problems.
Gastrointestinal symptoms are often the most prominent signs of a parasitic infection. These may include:
- Diarrhea
- Abdominal pain and cramping
- Nausea and vomiting
- Gas and bloating
- Loss of appetite
In some cases, parasites can cause more severe gastrointestinal symptoms, such as dysentery (loose stools containing blood and mucus) or rectal prolapse.
Systemic symptoms refer to those that affect the body as a whole. These may include:
- Fatigue and weakness
- Unexplained weight loss
- Fever and chills
- Muscle aches
- Headache
- Dizziness or fainting
Some parasites, such as those that cause malaria or sleeping sickness, can have a significant impact on the body’s overall functioning, leading to more severe systemic symptoms.
Skin-related symptoms are another common sign of parasitic infections. These may include:
- Itching and rash, particularly around the rectum or vulva
- Hives or welts
- Swelling and inflammation
- Sores or lesions
Certain parasites, such as scabies mites or lice, can cause intense itching and skin irritation as they burrow into the skin or feed on the host’s blood.
It’s important to note that some parasitic infections may not cause any symptoms at all, making it difficult to detect their presence without proper testing. In other cases, symptoms may develop gradually over time as the parasite population grows within the host’s body.
If you suspect that you may have a parasitic infection, it’s crucial to consult with a healthcare provider for an accurate diagnosis and appropriate treatment. Left untreated, parasitic infections can lead to more serious complications and long-term health problems.
Diagnosis and Treatment Options
Diagnosing parasitic infections involves a combination of stool tests, blood tests, and imaging studies to identify the specific parasite causing the infection. Treatment typically includes antiparasitic medications and supportive care to manage symptoms and prevent complications.
Stool tests are the most common method for diagnosing intestinal parasites. Patients provide multiple stool samples over several days, which are examined under a microscope for the presence of parasite eggs or larvae. Special staining techniques may be used to enhance visualization of certain parasites.
Blood tests can detect antibodies produced by the immune system in response to parasitic infections. Serology tests look for specific antibodies, while blood smears allow direct visualization of parasites in the blood. These tests are particularly useful for diagnosing parasites that invade tissues or cause systemic infections.
Imaging studies, such as X-rays, ultrasounds, or CT scans, may be used to assess the extent of organ damage caused by parasitic infections. For example, imaging can reveal cysts or lesions in the liver, lungs, or brain resulting from certain parasitic diseases.
Once the specific parasite has been identified, treatment with antiparasitic medications can begin. The choice of medication depends on the type of parasite and the severity of the infection. Common antiparasitic drugs include:
- Mebendazole for roundworm and hookworm infections
- Nitazoxanide for cryptosporidiosis
Supportive care is essential for managing symptoms and preventing complications associated with parasitic infections. This may include:
- Fluid and electrolyte replacement to prevent dehydration
- Nutritional support to address malnutrition
- Pain management and anti-inflammatory medications
- Treatment of secondary bacterial infections
In some cases, surgery may be necessary to remove cysts or repair organ damage caused by parasitic infections.
RELATED: Myalgic Encephalomyelitis: Symptoms, Causes, and Treatments
Successful treatment of parasitic infections requires a comprehensive approach that includes accurate diagnosis, appropriate antiparasitic therapy, and supportive care. Follow-up stool tests may be performed to confirm eradication of the parasite and monitor for potential reinfection.
Conclusion
Parasitic infections pose a significant health challenge, affecting millions worldwide. From protozoa to helminths and ectoparasites, these unwelcome guests can cause a range of symptoms and complications. Understanding the causes, risk factors, and common types of parasites has an impact on our ability to prevent and address these infections effectively. Accurate diagnosis and proper treatment are crucial to tackle parasitic infections and prevent long-term health issues.
To wrap up, managing parasitic infections requires a comprehensive approach. This includes maintaining good hygiene practices, being cautious while traveling to high-risk areas, and seeking prompt medical attention when symptoms arise. By staying informed and taking preventive measures, we can reduce the risk of parasitic infections and promote better health outcomes. Remember, early detection and appropriate treatment are key to overcoming these microscopic invaders and maintaining overall well-being.