Pinguecula is a common eye condition that affects many people worldwide. This small, yellowish bump on the surface of the eye can cause discomfort and concern for those who develop it. While often harmless, pinguecula has the potential to impact vision and eye health, making it essential to understand its causes, symptoms, and available treatments.
Eye care professionals frequently encounter patients with pinguecula, highlighting the importance of awareness and proper management. This article delves into the nature of pinguecula, explores its risk factors and prevalence, discusses how it’s diagnosed, and examines various treatment options. By shedding light on this eye condition, readers can gain valuable insights to help them make informed decisions about their eye health.
The Nature of Pinguecula



Pathophysiology
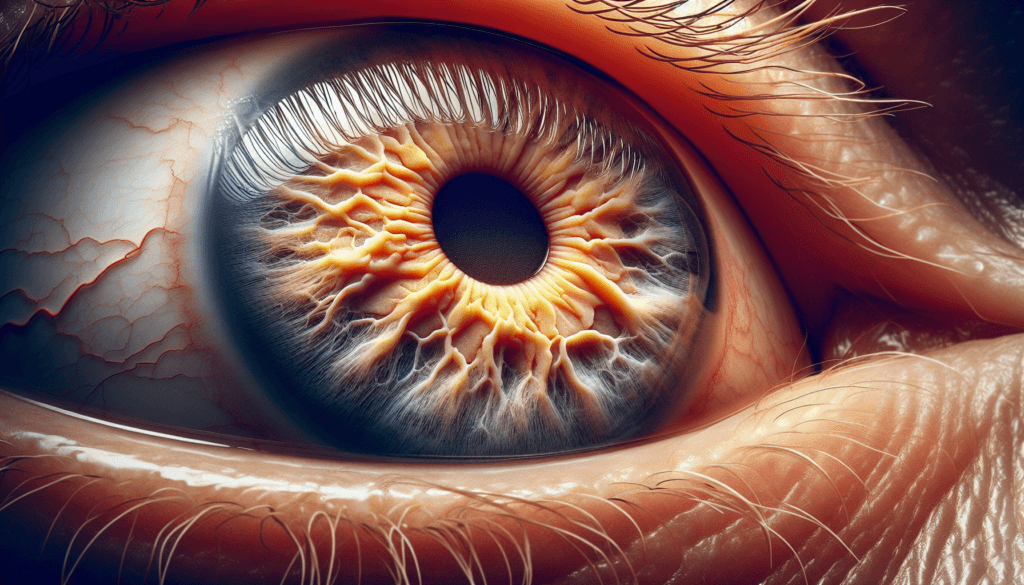
Pinguecula is characterized by elastotic degeneration of the conjunctival tissue. Histologically, the epithelium may be normal, thinned, hyperkeratotic or hyperplastic. The substantia propria exhibits basophilic staining, termed elastotic degeneration, which consists of material that stains for elastin but is not degraded by elastase. This elastotic degeneration is nodular in pinguecula. Fat or calcified globules are sometimes associated with the elastotic material.
Histological Changes
In patients with brown or black skin, epithelial racial melanosis is evident in the pinguecula. The subepithelial tissue shows senile elastosis and irregular, dense subepithelial concretions. These concretions stain positively for lysozyme. The elastotic material is positive for elastin, microfibrillar protein, and amyloid P, components that do not normally co-localize. This indicates that the control of elastogenesis is seriously defective, resulting in abnormal biochemical organization of the elastic fibers rather than overproduction. A marked reduction of elastic microfibrils appears to prevent normal assembly of elastic fibers.
RELATED: Myelofibrosis Symptoms and Treatment: What You Need to Know
Growth Patterns
Pingueculae are usually well-defined nodular lesions that occur within the interpalpebral conjunctiva, most commonly on the nasal side. They have a predilection for the nasal part of the bulbar conjunctiva. Pingueculae are bilateral in most cases but can be unilateral. The lesions almost always occur at the 3 o’clock or 9 o’clock positions of the limbus. Pingueculae appear as a grey white-yellow elevated round mass on the bulbar conjunctiva. The lesions are more frequent nasally, possibly due to increased ultraviolet light exposure from reflection off the side of the nose.
Risk Assessment and Epidemiology
Occupational Hazards
Individuals who spend a significant amount of time outdoors, particularly those exposed to wind, dust, and ultraviolet (UV) light, are at a higher risk of developing pinguecula. Occupations that involve prolonged exposure to these environmental factors, such as farmers, construction workers, and fishermen, have an increased likelihood of experiencing this condition. The constant irritation and damage caused by these elements can lead to the formation and progression of pinguecula over time.
Geographic Distribution
The prevalence of pinguecula varies across different regions of the world, with a higher incidence observed in areas closer to the equator. This geographic distribution is primarily attributed to the increased intensity of UV radiation in these regions. Studies have shown that populations living in tropical and subtropical climates, where sunlight exposure is more intense and prolonged, have a higher prevalence of pinguecula compared to those in temperate regions. This highlights the significant role of UV light in the development of this condition.
Genetic Factors
While environmental factors play a crucial role in the development of pinguecula, genetic predisposition may also contribute to an individual’s susceptibility. Some studies suggest that certain genetic variations may increase the likelihood of developing pinguecula, particularly in combination with environmental risk factors. However, more research is needed to fully understand the specific genetic mechanisms involved and their interaction with environmental triggers in the pathogenesis of pinguecula.
Clinical Presentation and Diagnosis
Physical Examination
Pinguecula is a benign lesion that appears as a small, yellowish bump on the bulbar conjunctiva. It usually occurs within the interpalpebral conjunctiva, typically at the 3 o’clock or 9 o’clock position near the limbus. While pinguecula has a predilection for the nasal side of the conjunctiva, it can appear on the temporal side as well. Though usually asymptomatic, an inflamed pinguecula (pingueculitis) may cause mild ocular irritation, foreign body sensation, and dryness. The presence of a pinguecula can interfere with the normal spreading of the tear film, leading to reduced tear break-up time and dry eye symptoms. During a slit-lamp examination, the eye care provider can closely assess the morphology and location of the pinguecula to distinguish it from other conjunctival lesions.
Differential Diagnosis
The differential diagnosis of pinguecula includes several other conjunctival conditions. Pterygium, a fleshy growth with numerous blood vessels, can be differentiated from pinguecula by its tendency to cross the limbus and encroach onto the cornea. Other conditions to consider include conjunctival intraepithelial neoplasia, which may resemble a keratinized pinguecula, as well as dermoid cysts, epithelial retention cysts, and inflammatory conditions such as episcleritis, angular conjunctivitis, and phlytenulosis. Careful examination and evaluation of the lesion’s characteristics are essential for accurate diagnosis.
RELATED: Leg Cramps: Why They Happen and How to Stop Them
Diagnostic Tools
While pinguecula can typically be diagnosed through a comprehensive eye examination, recent advancements in imaging technology have provided additional tools for assessing these lesions. Anterior segment optical coherence tomography (AS-OCT) allows for detailed visualization of the morphological patterns of pinguecula, revealing wedge-shaped masses that stop at the limbal region without elevating the corneal epithelium. This imaging modality can also help determine the thickness of the pinguecula. Additionally, optical coherence tomography angiography (OCTA) has been used to evaluate the vascularization of pinguecula, although studies have shown no significant difference in blood vessel density between normal conjunctiva and pinguecula. In rare cases where the appearance of the pinguecula is atypical, a conjunctival biopsy may be performed to rule out malignancy and confirm the diagnosis.
Treatment Strategies and Outcomes
Conservative Treatments
Treatment for pinguecula is rarely required. Artificial tears may be useful in mild cases of dryness or foreign body sensation. If inflammation is more severe, a short course of topical steroids or topical antibiotic–steroid in tapering dose may be indicated. Topical non-steroidal anti-inflammatory drugs are also effective in treating pingueculitis. Cold compresses may help patients with inflamed pinguecula.
Surgical Interventions
Surgical excision is considered only for cosmetic reasons. It is a final resort either in cases of chronic persistent irritation when conservative treatment has failed, and when interference with contact lens wear occurs. Excision should be followed by histological evaluation to exclude malignancy when the pinguecula is atypical in either location or appearance.
Argon laser photocoagulation is an alternative to standard surgical excision for pinguecula. It is a safe method for removing a pinguecula for cosmetic purposes. It provides control of the extent and depth of removal of tissue, thus reducing conjunctival defects and complications. Argon laser photocoagulation involves the use of argon green laser. A topical anesthetic drop is instilled into the conjunctival sac before the procedure. High power laser is used for thick pinguecula, whereas low power laser is appropriate for thinner pinguecula.
There were no significant differences between surgical excision and argon laser photocoagulation in cosmetic outcomes. Surgical excision of symptomatic pinguecula with conjunctival autograft with fibrin glue may improve cosmesis. It also improved dry eye symptoms.
RELATED: Understanding Laryngomalacia: Symptoms, Causes, and Treatments
Post-treatment Care
Following argon laser photocoagulation, the conjunctival defects are allowed to re-epithelialize. During the post-operative period, patients should receive a topical antibiotic steroid eye drop.
Patients are advised to take a day off on surgery date. Downtime is minimal and patients can expect to return to their normal routines a day after the procedure. To protect the eye, it is recommended that the patient wears an eyepatch for up to two days following the surgery. During the recovery period, patients generally use special drops to promote the healing process and reduce any inflammation associated with the procedure.
To decrease the possibility of recurrence, patients should routinely and adequately protect the eyes against UV light and dust, as well keep the eyes well lubricated when in dry environments. Wraparound sunglasses can be worn for protection and artificial tears can be used to add moisture to the eyes.
Conclusion
Pinguecula, a common eye condition, has a significant impact on eye health and comfort for many individuals worldwide. This article has explored its causes, symptoms, and treatment options, shedding light on the importance of understanding and managing this condition. From occupational hazards to geographic distribution, various factors contribute to the development of pinguecula, highlighting the need for preventive measures and early detection.
The diagnosis and treatment of pinguecula involve a range of approaches, from conservative management to surgical interventions when necessary. While often asymptomatic, pinguecula can cause discomfort and visual disturbances in some cases, making proper care and attention crucial. By staying informed about this condition and taking steps to protect the eyes from environmental stressors, individuals can play an active role in maintaining their ocular health and preventing the progression of pinguecula.