Placental abruption is a serious pregnancy complication that demands immediate attention and proper treatment. This condition occurs when the placenta partially or completely separates from the uterus before delivery, potentially jeopardizing the health of both mother and baby. Understanding placental abruption treatments is crucial for pregnant women to ensure timely intervention and optimal outcomes.
Expectant mothers and healthcare providers must be aware of the various approaches to manage placental abruption. These include emergency response protocols, stabilization techniques, and treatment strategies based on gestational age. The article will explore the different types of placental abruption, long-term implications for affected women and babies, and the importance of prompt medical care. By delving into these aspects, readers will gain valuable insights to navigate this challenging situation effectively.
Types of Placental Abruption
Revealed vs. Concealed Abruption
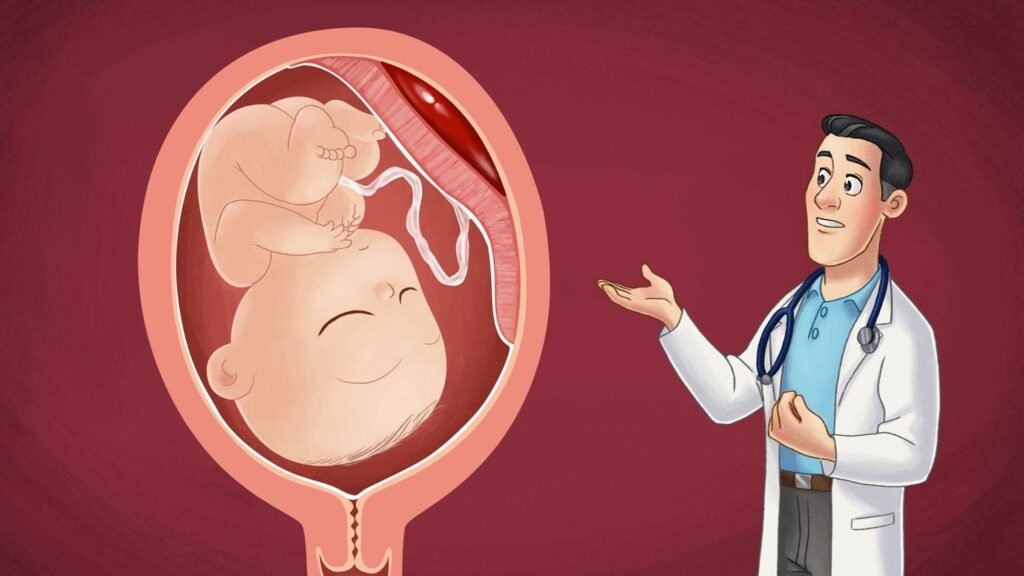
Placental abruption can be classified as revealed or concealed based on the presence or absence of visible vaginal bleeding. In a revealed abruption, blood from the separation of the placenta escapes through the cervix, resulting in noticeable vaginal bleeding. The amount of bleeding may vary from light to heavy, depending on the severity of the abruption. On the other hand, a concealed abruption occurs when the blood remains trapped between the placenta and the uterine wall. In this case, there may be no visible vaginal bleeding, making the diagnosis more challenging. However, the patient may still experience abdominal pain, uterine tenderness, and contractions. Concealed abruptions can be particularly dangerous as the accumulating blood can lead to significant maternal blood loss and fetal distress without obvious external signs.
RELATED: Bone Cancer: A Detailed Look at Diagnosis and Treatment
Partial vs. Complete Abruption
Placental abruptions can also be categorized as partial or complete based on the extent of placental separation from the uterine wall. In a partial abruption, only a portion of the placenta detaches from the uterus. The severity of symptoms and potential complications depend on the size and location of the separated area. Partial abruptions may cause intermittent or light bleeding, abdominal pain, and uterine tenderness. Fetal distress may occur if the separation disrupts a significant portion of the placental blood supply. In contrast, a complete abruption involves the entire placenta separating from the uterine wall. This is a medical emergency that can lead to severe maternal hemorrhage, disseminated intravascular coagulation (DIC), and fetal demise. Patients with a complete abruption often experience intense, sustained abdominal pain, uterine rigidity, and severe fetal distress. Prompt delivery, often by emergency cesarean section, is necessary to prevent life-threatening complications for both mother and baby. Recognizing the different types of placental abruption is crucial for appropriate management and timely intervention to optimize maternal and fetal outcomes.
Emergency Response and Stabilization
Initial Assessment
When a patient presents with symptoms suggestive of placental abruption, a rapid initial assessment is crucial. This includes evaluating the patient’s vital signs, assessing the severity of vaginal bleeding, and monitoring the fetal heart rate. A thorough physical examination should be performed, focusing on abdominal tenderness, uterine contractions, and signs of hypovolemic shock. Obtaining intravenous access with two large-bore lines is essential for fluid resuscitation and potential blood transfusion. Blood samples should be sent for a complete blood count, coagulation studies, and type and cross-match in anticipation of the need for blood products. Continuous external fetal monitoring is initiated to detect any signs of fetal distress, such as prolonged bradycardia or repetitive late decelerations. The optimal duration of monitoring after trauma has not been established; however, most placental abruptions occur within 6-9 hours of the event.
Immediate Interventions
Once placental abruption is suspected, immediate interventions are necessary to stabilize the mother and fetus. Crystalloid fluid resuscitation should be initiated to maintain adequate perfusion and prevent hypovolemic shock. If the patient remains hemodynamically unstable despite fluid resuscitation, blood transfusion should be started promptly. Correcting coagulopathy is crucial, as disseminated intravascular coagulation (DIC) can occur in severe cases of placental abruption.
Treatment Strategies Based on Gestational Age
Before 34 Weeks
When placental abruption occurs before 34 weeks of gestation, the primary goal is to prolong the pregnancy as much as possible to allow for fetal lung maturity. If the abruption is mild and both mother and fetus are stable, conservative management may be appropriate. This involves close monitoring of maternal and fetal well-being, including regular assessment of vital signs, fetal heart rate, and uterine activity. Corticosteroids may be administered to accelerate fetal lung development in anticipation of preterm delivery. However, if the abruption worsens or there are signs of maternal or fetal distress, immediate delivery is necessary to prevent further complications.
34-36 Weeks
Between 34 and 36 weeks of gestation, the decision to deliver or continue the pregnancy depends on the severity of the abruption and the condition of the mother and fetus. If the abruption is mild and both are stable, expectant management may be considered with close observation. This allows the fetus to gain additional maturity and reduces the risks associated with late preterm birth. However, if the placental abruption is moderate to severe or there are indications of maternal or fetal compromise, prompt delivery is essential. The mode of delivery, vaginal or cesarean, will depend on the clinical situation and the likelihood of achieving a safe vaginal birth.
RELATED: Understanding Blood Blisters: Causes and Effective Treatments
After 36 Weeks
When placental abruption occurs after 36 weeks of gestation, immediate delivery is usually recommended regardless of the severity of the abruption. At this stage of pregnancy, the risks associated with continuing the pregnancy often outweigh the benefits of allowing further fetal maturity. Prompt intervention is crucial to minimize the potential for maternal hemorrhage, disseminated intravascular coagulation, and fetal distress or demise. The decision between vaginal delivery and cesarean section will be based on factors such as the extent of the abruption, maternal and fetal status, and the likelihood of a successful vaginal birth. In cases of severe abruption or fetal distress, an emergency cesarean section may be necessary to ensure the best possible outcomes for both mother and baby.
Long-term Implications
Impact on Future Pregnancies
Women who have experienced placental abruption are at an increased risk of recurrence in subsequent pregnancies. The risk of recurrence ranges from 4% to 12%, depending on the severity of the initial abruption and the presence of other risk factors. Careful monitoring and management of future pregnancies are essential to minimize the risk of adverse outcomes. Women with a history of placental abruption should receive early prenatal care and be closely monitored for signs of abruption, such as vaginal bleeding, abdominal pain, and uterine tenderness. Ultrasound examinations may be performed more frequently to assess placental location and to detect any signs of separation. In some cases, prophylactic measures, such as bed rest or hospitalization, may be recommended to reduce the risk of recurrent abruption. Additionally, women with a history of placental abruption are at an increased risk of other pregnancy complications, such as preterm labor, intrauterine growth restriction, and stillbirth. Therefore, these pregnancies require a multidisciplinary approach with input from maternal-fetal medicine specialists, neonatologists, and other healthcare professionals to ensure optimal outcomes for both mother and baby.
RELATED: How to Recognize Bladder Cancer Symptoms Early
Psychological Effects
The experience of placental abruption can have significant psychological effects on the mother and her family. The sudden onset of symptoms, the potential for life-threatening complications, and the uncertainty surrounding the outcome of the pregnancy can be extremely stressful and traumatic. Women who have experienced placental abruption may develop post-traumatic stress disorder (PTSD), anxiety, or depression. These psychological effects can persist long after the physical recovery from the abruption and may impact the mother’s ability to bond with her baby and adjust to motherhood. It is important for healthcare providers to recognize the psychological impact of placental abruption and to provide appropriate support and referrals to mental health professionals. Counseling, support groups, and other resources can help women and their families cope with the emotional aftermath of this serious complication. Additionally, healthcare providers should be sensitive to the mother’s emotional needs during subsequent pregnancies, as the fear of recurrence can be a significant source of anxiety. Providing reassurance, education, and a supportive environment can help alleviate some of these concerns and promote a positive pregnancy experience.
Conclusion
To wrap up, placental abruption is a serious pregnancy complication that has a significant impact on both maternal and fetal health. Prompt recognition and appropriate management are crucial to optimize outcomes. The treatment approach depends on various factors, including the severity of the abruption, gestational age, and the condition of the mother and baby. Healthcare providers must be prepared to implement emergency protocols and make quick decisions to ensure the best possible care.
Women who have experienced placental abruption may face challenges in future pregnancies and might need extra support to deal with the psychological effects. Close monitoring and early intervention are key to managing subsequent pregnancies. By understanding the types, treatments, and long-term implications of placental abruption, expectant mothers and healthcare professionals can work together to navigate this condition effectively, aiming to protect the health and well-being of both mother and baby.