In the realm of tick-borne illnesses, Lyme disease emerges as a formidable adversary, affecting thousands of individuals annually with a spectrum of symptoms that can significantly impair one’s quality of life. The significance of understanding Lyme disease, from its early detection to effective treatment strategies, cannot be overstated in public health discussions. Given its capacity to mimic other conditions and the potential for long-term health complications, Lyme disease represents a critical area of concern for both healthcare providers and those at risk.
This article endeavors to equip readers with comprehensive insights into Lyme disease, including an examination of its symptoms, causes, and risk factors. Furthermore, it delicates to navigating the complexities of diagnosis and testing, followed by an overview of current treatment options available. A pivotal section on preventing Lyme disease offers practical advice for minimizing exposure to this insidious disease, highlighting the indispensable role of preventive measures in combating its spread. Ultimately, this guide aims to serve as an essential resource for those seeking to understand and mitigate the impacts of Lyme disease on individuals and communities alike.
Understanding Lyme Disease
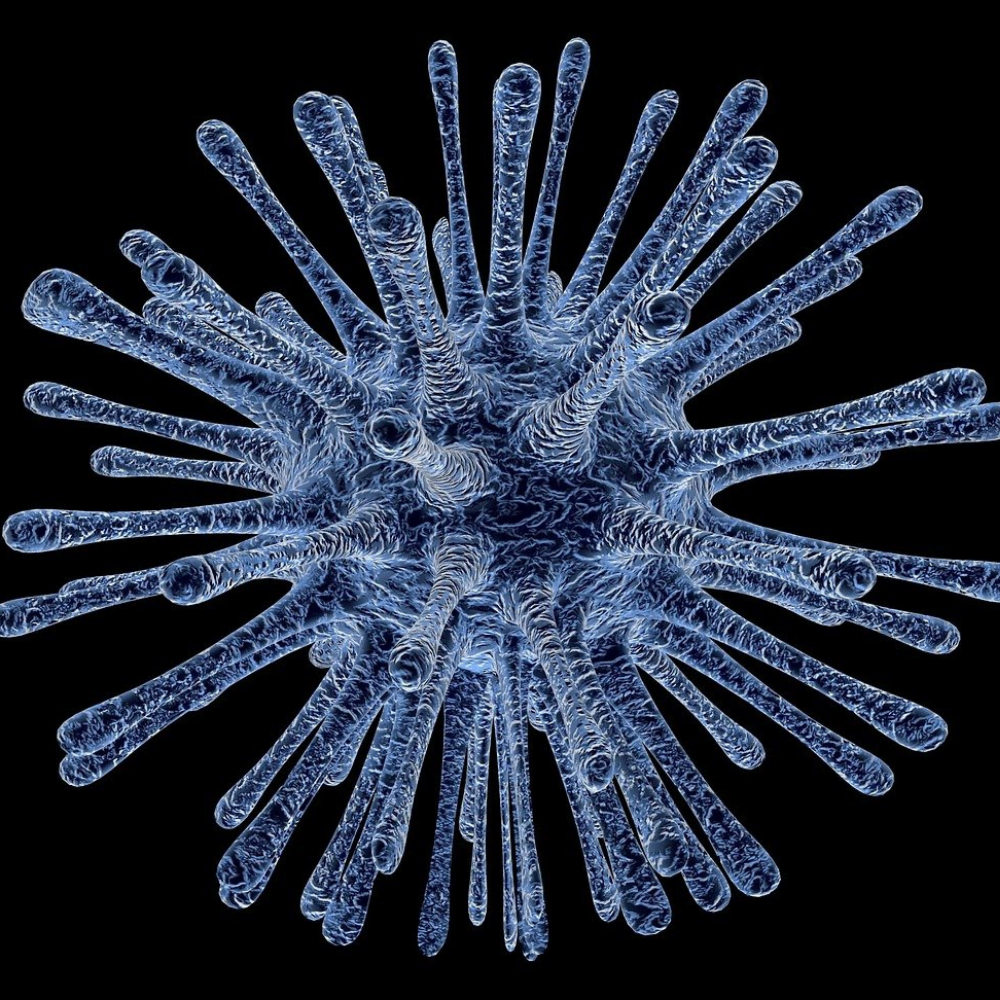
Lyme disease is a potentially serious illness caused by the bacteria Borrelia burgdorferi and, rarely, B. mayonii. These bacteria are transmitted to humans through the bite of infected blacklegged ticks, also known as deer ticks. The disease can affect people of any age and is most prevalent in the northeastern, north-central, and mid-Atlantic states of the United States.
What Lyme Disease Is
Lyme disease is an infectious disease that can cause a variety of symptoms, ranging from mild to severe. The most common early symptom is a circular bull’s eye rash called erythema migrans, which appears around the site of the tick bite in 60-80% of cases. Other early symptoms may include chills, fever, headache, fatigue, stiff neck, muscle and joint pain, and swollen glands. If left untreated, Lyme disease can lead to more severe complications involving the joints, heart, and nervous system.
RELATED: Asherman’s Syndrome: Diagnosis, Management, and Treatment Options
How Lyme Disease Spreads
Lyme disease is primarily spread through the bite of infected blacklegged ticks. These ticks have a two-to-three-year life cycle and can become infected with the Lyme disease bacteria when feeding on infected wildlife hosts, usually rodents. The bacteria are then passed on to the next life stage of the tick and can be transmitted to humans during the tick’s next blood meal.
For the bacteria to be transmitted, the infected tick must be attached to the skin for more than 24 hours. Prompt removal of the tick within this timeframe can greatly reduce the chances of contracting Lyme disease. It is important to note that Lyme disease cannot be spread through touching, kissing, or sexual contact, and there is no evidence of transmission from infected pets to humans.
Areas with High Prevalence
Lyme disease is most commonly reported in the northeastern, north-central, and mid-Atlantic states of the United States. The blacklegged tick, which transmits the disease in these regions, is found primarily in forested areas. In the Pacific Coast states, the western blacklegged tick is responsible for spreading the infection, although in smaller geographic areas.
The percentage of infected ticks varies depending on the area and life stage of the tick, ranging from none to over 50%. It is crucial for individuals living in or visiting these high-risk areas to take preventive measures, such as wearing protective clothing, using insect repellents, and performing thorough tick checks after spending time outdoors.
Symptoms of Lyme Disease





The symptoms of Lyme disease can vary depending on the stage of the infection. In the early stages, symptoms may be mild and easily overlooked, while advanced stages can lead to more severe complications if left untreated.
Early Symptoms
The most common early symptom of Lyme disease is a distinctive skin rash called erythema migrans (EM). This rash:
- Appears at the site of the tick bite, usually within 3 to 30 days after the bite
- Gradually expands over several days, reaching up to 12 inches or more across
- May resemble a bull’s-eye with a central red spot surrounded by a clear area and a red outer ring
- Can appear on any area of the body and may be warm to the touch but is rarely painful or itchy
Other early symptoms, which may occur with or without the rash, include:
- Fever and chills
- Fatigue
- Headache
- Muscle and joint pain
- Swollen lymph nodes
Advanced Symptoms
If Lyme disease is not treated promptly, the infection can spread to other parts of the body, leading to more serious symptoms weeks to months after the initial tick bite. These symptoms may include:
- Joint pain and swelling, particularly in the knees
- Neurological problems, such as numbness, weakness, tingling sensations, facial palsy, and meningitis
- Intermittent pain in tendons, muscles, joints, and bones
- Heart palpitations or an irregular heartbeat (Lyme carditis)
- Dizziness or shortness of breath
- Inflammation of the eyes or liver
- Severe fatigue
Symptoms in Children
Children with Lyme disease generally present with symptoms similar to those in adults. However, some key differences include:
- Rash may appear in a different shape, such as a solid red rash instead of the classic bull’s-eye
- Neurologic symptoms may be more pronounced, including facial palsy and meningitis
- Arthritis is less common in children than in adults
It is essential to note that the symptoms of Lyme disease can mimic other conditions, making diagnosis challenging. If you suspect that you or your child may have Lyme disease, consult a healthcare professional promptly for proper diagnosis and treatment to prevent potential complications.
Causes and Risk Factors
Lyme disease is caused by the bacterium Borrelia burgdorferi and rarely, Borrelia mayonii. These bacteria are transmitted to humans through the bite of infected black-legged ticks, commonly known as deer ticks.
Bacteria Involved
In the United States, Lyme disease is primarily caused by the bacteria Borrelia burgdorferi and Borrelia mayonii. These bacteria are carried by black-legged or deer ticks, which become infected when feeding on small animals that harbor the bacteria, such as mice and other rodents.
Tick Exposure
Ticks can attach to any part of the human body but are often found in hard-to-see areas such as the groin, armpits, and scalp. In most cases, the tick must be attached for 36 to 48 hours or more before the Lyme disease bacterium can be transmitted.
The chances of being bitten by a deer tick are greater during times of the year when ticks are most active. Young deer ticks, called nymphs, are active from mid-May to mid-August and are about the size of poppy seeds. Adult ticks, which are approximately the size of sesame seeds, are most active from March to mid-May and from mid-August to November. Both nymphs and adults can transmit Lyme disease.
RELATED: Ascites Explained: Key Causes, Symptoms, and Treatment Options
High-Risk Activities
Several factors can increase the risk of getting Lyme disease, including:
- Spending time in wooded or grassy areas where ticks carrying Lyme disease thrive, particularly in the Northeast and Midwest regions of the United States.
- Having exposed skin when in tick-infested areas, as ticks can attach more easily.
- Failing to remove ticks promptly or properly, allowing them to remain attached for 36 to 48 hours or longer, which increases the risk of infection.
Individuals who live or spend time in wooded areas or have pets that visit these areas are at an increased risk of exposure to ticks. Outdoor occupations such as landscaping, forestry, and wildlife management can also elevate the risk. Taking precautions such as wearing protective clothing, using insect repellents, and performing thorough tick checks can help reduce the likelihood of tick bites and Lyme disease transmission.
Diagnosis and Testing
Diagnosing Lyme disease can be challenging, as the symptoms often mimic other illnesses. Healthcare providers consider multiple factors when evaluating a patient for Lyme disease, including the signs and symptoms, likelihood of exposure to infected ticks, and the possibility of other illnesses causing similar symptoms. Laboratory testing is also an important component of the diagnostic process.
When to See a Doctor
If an individual suspects they may have Lyme disease, it is crucial to seek medical attention promptly. Early diagnosis and treatment can help prevent the development of more severe symptoms and long-term complications. Patients should consult a healthcare provider if they:
- Live in or have recently visited an area where Lyme disease is common
- Have a rash that resembles a bull’s-eye or have other symptoms of Lyme disease
- Have been bitten by a tick and are experiencing symptoms
Diagnostic Tests Available
The primary diagnostic tool for Lyme disease is a blood test that detects antibodies to the Lyme bacteria. However, it is important to note that it can take several weeks after infection for the immune system to produce enough antibodies to be detected by the test. The Centers for Disease Control and Prevention (CDC) recommends using FDA-cleared antibody tests that follow a two-step process:
- Enzyme immunoassay (EIA) or immunofluorescence assay (IFA): These tests measure the level of antibodies in the blood. If the result is negative, no further testing is necessary. If the result is positive or inconclusive, the second step is performed.
- Western blot test: This test is used to confirm the results of the first test. It detects antibodies to specific proteins of the Lyme bacteria.
In some cases, healthcare providers may also use other diagnostic methods, such as a polymerase chain reaction (PCR) test to detect the DNA of the Lyme bacteria in joint fluid or cerebrospinal fluid.
At-Home Testing Kits
While some laboratories offer at-home testing kits for Lyme disease, it is essential to exercise caution when using these products. Many at-home tests are not cleared or approved by the FDA and may provide inaccurate results. Additionally, interpreting the results of these tests can be challenging without the guidance of a healthcare professional.
If an individual chooses to use an at-home testing kit, they should follow up with a healthcare provider to confirm the results and discuss appropriate treatment options. It is crucial to remember that a positive test result does not necessarily mean an individual has Lyme disease, as false positives can occur.
In conclusion, diagnosing Lyme disease involves a combination of clinical evaluation and laboratory testing. Patients who suspect they may have Lyme disease should seek medical attention promptly and work closely with their healthcare provider to ensure an accurate diagnosis and appropriate treatment plan.
Treatment Options
The primary treatment for Lyme disease is antibiotics, which are most effective when administered in the early stages of the infection. The choice of antibiotic, dosage, and duration of treatment depends on factors such as the patient’s age, symptoms, and the presence of any complications.
Antibiotic Treatment
The most commonly prescribed antibiotics for Lyme disease include:
- Amoxicillin: This antibiotic is often prescribed for adults, younger children, and pregnant or breastfeeding women. The usual dosage is 500 mg orally three times a day.
In cases of neurological or cardiac complications, intravenous (IV) antibiotics may be necessary.
Duration and Effectiveness
The duration of antibiotic treatment varies depending on the stage and severity of the disease:
- Early Lyme disease: Treatment usually lasts 10-14 days.
- Lyme arthritis: Treatment may extend to 28 days.
- Neurological or cardiac complications: Treatment typically lasts 14-21 days.
It is crucial to complete the full course of antibiotics as prescribed, even if symptoms improve before the end of the treatment period. Most patients who receive prompt treatment in the early stages of Lyme disease recover rapidly and completely.
Handling Complications
In some cases, patients may experience persistent symptoms or develop complications despite receiving appropriate antibiotic treatment. These situations may require additional or prolonged antibiotic therapy, as determined by a healthcare provider.
| Complication | Treatment |
|---|---|
| Lyme arthritis | Oral antibiotics for 28 days or IV antibiotics if oral treatment is ineffective |
| Neurological manifestations | IV antibiotics for 14-21 days |
| Cardiac manifestations | IV antibiotics for 14-21 days; oral antibiotics may be sufficient for mild carditis |
It is important to note that the term “chronic Lyme disease” is not well-defined, and ongoing symptoms after treatment are not necessarily indicative of persistent infection. In such cases, healthcare providers should work with patients to identify the cause of their symptoms and determine the most appropriate treatment plan.
Preventing Lyme Disease
Preventing Lyme disease involves taking precautions to reduce the risk of tick bites and promptly removing any attached ticks. The following strategies can help minimize the chances of contracting Lyme disease:
Avoiding Tick Bites
One of the most effective ways to prevent Lyme disease is to avoid areas where ticks are prevalent, such as tall grass, brushy areas, and leaf litter. When hiking or walking in the woods, stay in the center of trails and avoid contact with vegetation. Wearing light-colored clothing can make it easier to spot ticks on your body.
To further protect yourself from tick bites, follow these steps:
- Wear long-sleeved shirts and long pants tucked into socks or boots.
- Use permethrin-treated clothing and gear for added protection.
- Check your clothing, gear, and pets for ticks after spending time outdoors.
- Shower soon after coming indoors to wash off any unattached ticks.
- Conduct a full-body tick check, paying close attention to areas such as the scalp, behind the ears, armpits, groin, and behind the knees.
Using Repellents
Insect repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus (OLE), para-menthane-diol (PMD), or 2-undecanone can help repel ticks. Always follow the product instructions carefully and reapply as directed. When using repellents on children, avoid applying them to the hands, eyes, or mouth.
Permethrin is another effective tick repellent that can be applied to clothing and gear. Treat items such as boots, pants, socks, and tents with permethrin before heading outdoors. Pre-treated clothing is also available and can provide long-lasting protection against ticks.
RELATED: Ascending Aortic Aneurysm: Early Signs, Risks, and Treatments
Checking for Ticks
After spending time in tick-infested areas, thoroughly inspect yourself, your children, and your pets for ticks. Use a hand-held or full-length mirror to view all parts of your body, including hard-to-see areas. If you find an attached tick, remove it promptly using fine-tipped tweezers.
To remove a tick:
- Grasp the tick as close to the skin’s surface as possible.
- Pull upward with steady, even pressure to avoid crushing the tick’s body.
- After removal, clean the bite area and your hands with rubbing alcohol or soap and water.
- Dispose of the tick by flushing it down the toilet or sealing it in a container.
If you develop a rash or fever within several weeks of removing a tick, consult your healthcare provider and mention your recent tick bite. Early diagnosis and treatment of Lyme disease can help prevent more serious complications.
By following these prevention strategies and remaining vigilant about tick exposure, you can significantly reduce your risk of contracting Lyme disease and enjoy outdoor activities with greater peace of mind.
Conclusion
Through a detailed exploration of Lyme disease’s symptoms, causes, and preventative measures, this guide has aimed to arm individuals and communities with the knowledge necessary to combat this tick-borne illness effectively. By spotlighting the importance of early detection, appropriate medical intervention, and diligent preventative practices, it underscores the critical nature of awareness and proactive behavior in mitigating the risks associated with Lyme disease. The collective effort to understand and address this condition not only signifies a step forward in personal health management but also enhances our collective resilience against such diseases.
The implications of Lyme disease, from its potential to cause long-term health issues to its impact on quality of life, extend far beyond the individual, touching upon broader public health strategies and the importance of environmental awareness. As we continue to navigate these challenges, the call to action for ongoing research, community education, and individual precaution becomes ever more poignant. Embracing the insights shared within this article can empower us to lead safer, healthier lives while contributing to a broader culture of awareness and prevention against Lyme disease.