Primary ciliary dyskinesia is a rare genetic disorder that affects the tiny hair-like structures called cilia in various organs of the body. This condition has an impact on the normal functioning of cilia, leading to a range of health issues primarily affecting the respiratory system. Understanding what primary ciliary dyskinesia is and its implications is crucial for patients newly diagnosed with this condition, as well as for their families and caregivers.
This article aims to provide a comprehensive overview of primary ciliary dyskinesia to help patients navigate their diagnosis and treatment. It will explore the underlying causes of the disorder, common symptoms, and diagnostic procedures. Additionally, the article will discuss available treatment options and management strategies to improve quality of life for those living with primary ciliary dyskinesia. By the end, readers will have a clearer understanding of this complex condition and the steps they can take to manage it effectively.
What is Primary Ciliary Dyskinesia?
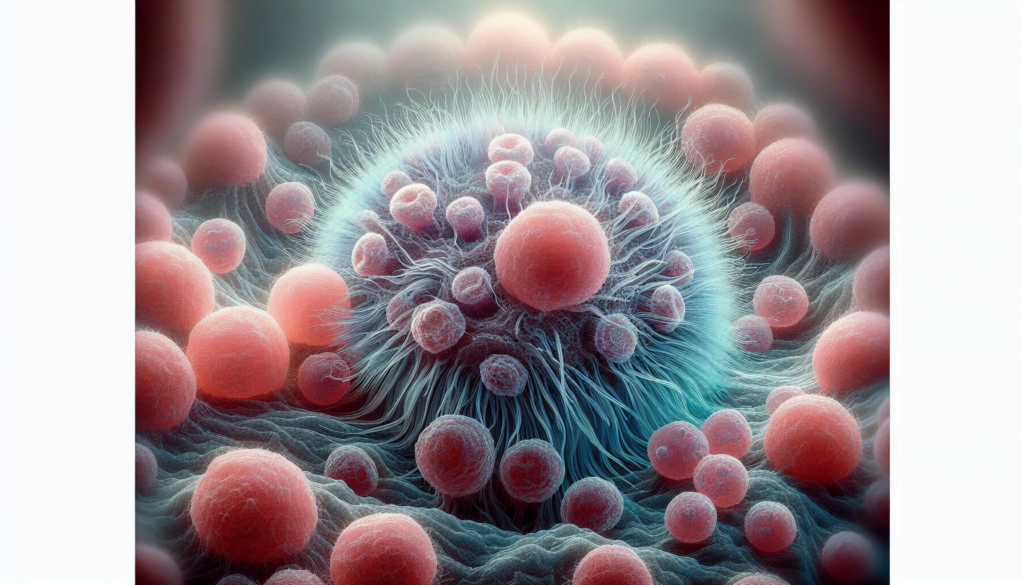
Primary ciliary dyskinesia is a rare genetic disorder that affects the structure and function of motile cilia, which are hair-like structures present on the surface of cells in various organs of the body. These cilia play a crucial role in the normal functioning of the respiratory system by clearing mucus and other particles from the airways. In individuals with primary ciliary dyskinesia, the cilia are either immotile or have an abnormal beating pattern, leading to impaired mucociliary clearance.
The prevalence of primary ciliary dyskinesia is estimated to be around 1 in 10,000 to 20,000 individuals. It is caused by mutations in genes that encode proteins essential for the assembly, structure, and function of motile cilia. To date, over 50 genes have been associated with primary ciliary dyskinesia, with the majority following an autosomal recessive inheritance pattern. This means that an individual must inherit one copy of the mutated gene from each parent to develop the disorder.
RELATED: Fungal Infections Explained: Types, Causes, and Effective Treatments
The motile cilia are composed of hundreds of proteins that form a complex structure called the axoneme. The axoneme consists of nine peripheral microtubule doublets surrounding a central pair of microtubules, creating a “9+2” arrangement. Emanating from the peripheral doublets are the outer and inner dynein arms, which contain enzymes that hydrolyze ATP to generate the force necessary for ciliary beating. Mutations in genes encoding these structural components or proteins involved in their assembly can lead to various ultrastructural defects in the cilia, such as the absence of outer or inner dynein arms, central pair abnormalities, or disorganization of the microtubules.
These ultrastructural defects result in the characteristic clinical features of primary ciliary dyskinesia, which primarily affect the respiratory system. The impaired mucociliary clearance leads to the accumulation of mucus and bacteria in the airways, causing chronic respiratory infections, sinusitis, and otitis media. Over time, this can result in the development of bronchiectasis, a condition characterized by the irreversible dilation of the bronchi due to repeated infections and inflammation.
Symptoms and Diagnosis
Common symptoms
Primary ciliary dyskinesia (PCD) is characterized by a range of symptoms that primarily affect the respiratory system. The most common manifestations include chronic wet cough, which is present in nearly all infants with PCD, and year-round nasal congestion starting from early childhood. Recurrent lower respiratory tract infections, such as pneumonia, are also frequently observed, affecting up to 80% of PCD patients by preschool age.
In addition to respiratory symptoms, approximately 50% of individuals with PCD have situs inversus totalis, a condition where the internal organs are arranged in a mirror image of their normal positions. Other laterality defects, such as situs ambiguus, can also occur in PCD patients.
Chronic otitis media with effusion is another common feature, affecting at least 80% of children with PCD, particularly in the first year of life. This can lead to complications such as hearing loss, speech and language delay, and the need for multiple sets of pressure equalization tubes.
Diagnostic tests
Diagnosing PCD can be challenging, as there is no single definitive test. A combination of clinical history, physical examination, and various diagnostic tests are used to confirm the diagnosis. Nasal nitric oxide (nNO) measurement is a useful screening tool, as PCD patients typically have very low nNO levels compared to healthy individuals. However, other conditions, such as cystic fibrosis, can also result in low nNO levels, so further testing is necessary for a definitive diagnosis.
Electron microscopy of respiratory cilia obtained through nasal scrape or brush biopsy is considered the gold standard for diagnosing PCD. This test can reveal ultrastructural defects in the cilia, such as missing or abnormal dynein arms, which are characteristic of PCD. However, some patients with PCD may have normal ciliary ultrastructure, necessitating additional tests.
Genetic testing is another valuable diagnostic tool, as researchers have identified numerous genes associated with PCD. A positive genetic test can confirm the diagnosis, particularly in cases where ciliary ultrastructure appears normal.
RELATED: Frozen Shoulder: Expert Advice on Symptoms and Treatments
Challenges in diagnosis
Despite advances in diagnostic methods, PCD remains underdiagnosed due to several challenges. The clinical presentation of PCD can overlap with other common respiratory conditions, such as asthma, chronic bronchitis, and recurrent pneumonia, leading to misdiagnosis or delayed diagnosis. Additionally, not all healthcare providers are familiar with the diagnostic tests for PCD, and some tests, such as electron microscopy and genetic testing, may not be readily available in all clinical settings.
Another challenge in diagnosing PCD is the variability in ciliary ultrastructure and function among patients. Some individuals with PCD may have subtle or atypical defects that are not easily detected by standard diagnostic tests. Moreover, secondary ciliary dysfunction caused by infections or environmental factors can mimic the features of PCD, further complicating the diagnostic process.
To overcome these challenges, a multidisciplinary approach involving pediatric pulmonologists, otolaryngologists, and geneticists is essential. Referral to specialized PCD centers with expertise in diagnostic testing and management can facilitate timely and accurate diagnosis. Ongoing research efforts aim to improve diagnostic methods and identify new PCD-associated genes, which will enhance our understanding of this complex disorder and lead to better patient care.
Treatment and Management
Daily care routines
The cornerstone of primary ciliary dyskinesia management involves daily airway clearance techniques, including chest physiotherapy and physical exercise, to improve mucociliary clearance and prevent the accumulation of mucus in the airways. Patients should perform these techniques regularly, even when feeling well, as they are essential to maintaining lung health. Nasal saline irrigation and topical nasal steroids can help alleviate chronic rhinosinusitis symptoms, which are common in individuals with primary ciliary dyskinesia.
RELATED: Understanding Fragile X Syndrome (FXS): A Comprehensive Guide
Medications
Prompt treatment of respiratory tract infections is crucial in primary ciliary dyskinesia. Antibiotics should be initiated at the first sign of a respiratory exacerbation, guided by sputum or cough swab culture results when possible. Chronic macrolide therapy, such as azithromycin, has been shown to reduce exacerbation frequency in primary ciliary dyskinesia patients. Inhaled hypertonic saline may aid in mucus clearance, although its efficacy in this population requires further study. The role of other medications, such as inhaled corticosteroids and bronchodilators, remains unclear and should be evaluated on an individual basis.
Importance of early intervention
Early diagnosis and initiation of appropriate treatment are critical in primary ciliary dyskinesia to prevent irreversible lung damage and maintain lung function. Regular monitoring of lung function, microbial surveillance, and timely intervention can help slow disease progression and improve quality of life. Patients with primary ciliary dyskinesia should be followed closely by a multidisciplinary team experienced in managing this rare disorder to ensure optimal care and outcomes.
Conclusion
Primary ciliary dyskinesia is a complex genetic disorder that has a significant impact on patients’ respiratory health and quality of life. The combination of daily care routines, prompt treatment of infections, and regular monitoring by a multidisciplinary team is key to manage this condition effectively. Early diagnosis and intervention play a crucial role to slow down the progression of lung damage and maintain optimal lung function.
To wrap up, living with primary ciliary dyskinesia presents unique challenges, but with proper understanding and management, patients can lead fulfilling lives. Ongoing research efforts aim to improve diagnostic methods and treatment options, offering hope for better outcomes in the future. As awareness of this rare disorder grows, it’s likely to lead to earlier diagnoses and more targeted therapies to help patients breathe easier.