Prurigo nodularis is a chronic skin condition that can cause intense itching and discomfort. This challenging disorder affects people of all ages and backgrounds, leading to the formation of hard, itchy bumps on the skin that can significantly impact quality of life. Understanding prurigo nodularis is crucial for those affected and their caregivers, as proper management can help alleviate symptoms and improve overall well-being.
This article aims to shed light on the key aspects of prurigo nodularis. It will explore the nature of the condition, its typical symptoms and appearance, and the factors that may contribute to its development. Additionally, the piece will discuss diagnostic approaches and available treatment options, providing readers with valuable insights to better understand and address this persistent skin disorder.
What is Prurigo Nodularis?



Definition
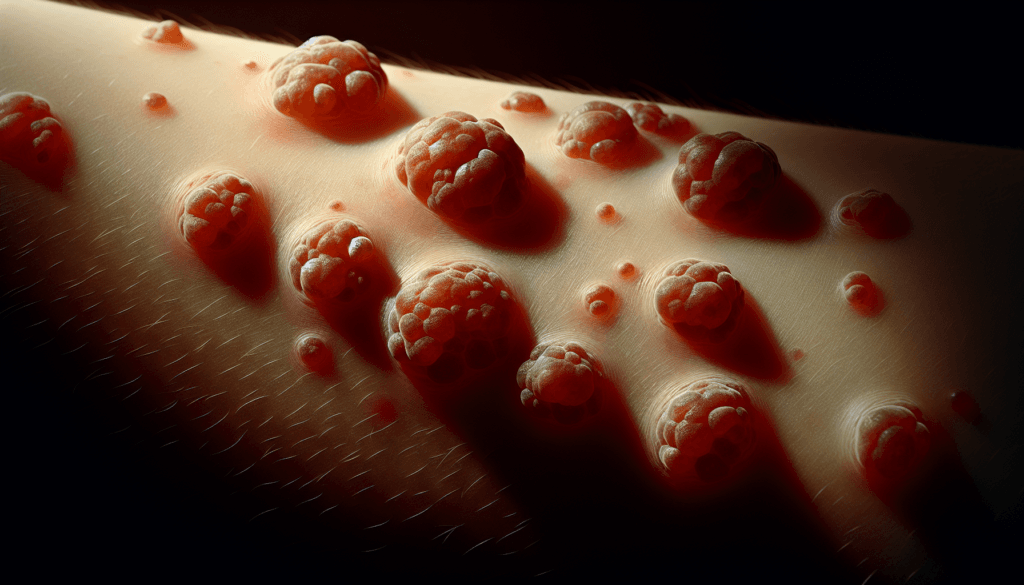
Prurigo nodularis (PN) is a chronic skin condition characterized by the presence of intensely itchy, firm bumps or nodules on the skin. These nodules are often symmetrically distributed and typically appear on the arms, legs, and trunk. The persistent itching associated with prurigo nodularis can significantly impact a person’s quality of life.
Characteristics
The nodules in prurigo nodularis are usually hard and dome-shaped, ranging in size from a few millimeters to several centimeters in diameter. They may be skin-colored, pink, or darkly pigmented. The skin surrounding the nodules is often thickened and rough due to repeated scratching. The intense itching sensation leads to a vicious cycle of scratching, which further exacerbates the formation of new nodules and perpetuates the condition.
RELATED: Living with Obsessive-Compulsive Personality Disorder (OCPD)
Prevalence
While the exact prevalence of prurigo nodularis is not well-established, recent studies suggest that it affects approximately 72 out of every 100,000 people in the United States. However, this figure may be an underestimation, as prurigo nodularis is often underdiagnosed or misdiagnosed. The condition tends to be more common in middle-aged and older adults, with a slightly higher prevalence in women compared to men. Certain underlying health conditions, such as atopic dermatitis, chronic kidney disease, and psychiatric disorders, may increase the risk of developing prurigo nodularis.
Symptoms and Appearance
Itchy bumps
Prurigo nodularis causes intensely itchy bumps or nodules that can appear anywhere on the body where the skin can be scratched, picked, or rubbed. These nodules are usually firm and dome-shaped, varying in size from a few millimeters to several centimeters in diameter. The itching sensation associated with these bumps is often severe and can lead to a vicious cycle of scratching, which further exacerbates the formation of new nodules.
Distribution on the body
While prurigo nodularis can develop anywhere on the skin, it most commonly affects the arms, legs, upper back, lower back, buttocks, and abdomen. The distribution of the nodules is often symmetrical, meaning they appear on both sides of the body in similar locations. The intense itching can be localized to a few areas or cover a large portion of the skin, depending on the individual.
Skin changes
As a result of the persistent scratching and rubbing, the skin surrounding the nodules often becomes thickened, rough, and discolored. The nodules themselves may be skin-colored, pink, or darkly pigmented, depending on the individual’s skin tone and the duration of the condition. In some cases, the itching can be so severe that it causes the nodules to break open and bleed, increasing the risk of infection. Over time, the repeated scratching can lead to further skin changes, such as the development of dark spots or scars where the nodules once were.
Causes and Risk Factors
Underlying conditions
Several underlying conditions have been associated with the development of prurigo nodularis. These include atopic dermatitis, chronic kidney disease, liver disease, HIV infection, and certain malignancies. Prurigo nodularis may also occur in conjunction with other inflammatory skin conditions such as psoriasis, lichen planus, and bullous pemphigoid. In some cases, the intense itching and scratching associated with these conditions can lead to the formation of the characteristic nodules seen in prurigo nodularis.
RELATED: Nocturia Explained: What Causes Frequent Nighttime Urination?
Immune system involvement
The immune system plays a significant role in the pathogenesis of prurigo nodularis. Studies have shown that the skin lesions in prurigo nodularis exhibit an increased number of immune cells, including T cells, eosinophils, and mast cells. These cells release various inflammatory mediators, such as interleukins and cytokines, which contribute to the itching and inflammation associated with the condition. Additionally, recent research has identified a potential role for Th22 cells and their associated cytokine, IL-22, in the development of prurigo nodularis.
Neural factors
Neuronal dysregulation is another key factor in the development of prurigo nodularis. The skin lesions in prurigo nodularis have been found to have an increased density of nerve fibers in the dermis, along with a decreased density of nerve fibers in the epidermis. This altered distribution of nerve fibers may contribute to the intense itching experienced by patients with prurigo nodularis. Furthermore, the release of neuropeptides such as substance P and calcitonin gene-related peptide (CGRP) from these nerve fibers can further exacerbate the itching and inflammation in the affected skin.
Diagnosis and Treatment Options
Clinical examination
Prurigo nodularis is primarily a clinical diagnosis based on the presence of characteristic itchy, firm papules or nodules. A thorough physical examination is essential to assess the distribution, size, and appearance of the lesions. Particular attention should be paid to the extensor surfaces of the arms and legs, as these are the most commonly affected areas. The skin surrounding the nodules may appear thickened, rough, or discolored due to chronic scratching. In some cases, the lesions may be excoriated or crusted, indicating the intense pruritus experienced by the patient.
Biopsy
Although the diagnosis of prurigo nodularis is typically made based on clinical findings, a skin biopsy may be performed in certain situations. If the lesions are not responding to initial treatments or if there are concerns about secondary complications such as infection or malignancy, a biopsy can provide valuable information. Histologically, prurigo nodularis exhibits characteristic features such as compact orthohyperkeratosis, irregular epidermal hyperplasia, hypergranulosis, and fibrosis of the papillary dermis. The presence of increased fibroblasts and capillaries in the dermis is also a common finding. Direct immunofluorescence may be utilized to differentiate prurigo nodularis from autoimmune disorders that can present with similar clinical features.
Topical treatments
Topical therapies play a crucial role in the management of prurigo nodularis. High-potency topical corticosteroids are often the first-line treatment, as they have anti-inflammatory and antipruritic effects. These medications can be applied directly to the lesions or used under occlusion to enhance their penetration and efficacy. Topical calcineurin inhibitors, such as tacrolimus and pimecrolimus, have also shown promise in reducing pruritus and inflammation associated with prurigo nodularis. These agents are particularly useful for patients who cannot tolerate or have contraindications to topical corticosteroids. Other topical options include menthol, phenol, pramoxine, and capsaicin creams, which work by providing a cooling or numbing sensation to alleviate itching.
RELATED: Night Terrors: Causes, Symptoms, and Treatment Options
Systemic medications
In cases of severe or refractory prurigo nodularis, systemic medications may be necessary to control symptoms and promote healing. Antihistamines, particularly those with sedative properties, can be helpful in reducing nighttime pruritus and improving sleep quality. Oral corticosteroids, such as prednisone, may be prescribed for short courses to rapidly control inflammation and itching. However, long-term use of systemic corticosteroids should be avoided due to potential side effects. Other immunosuppressive agents, including methotrexate, cyclosporine, and azathioprine, have been used off-label for the treatment of prurigo nodularis with varying degrees of success. More recently, targeted therapies like dupilumab and nemolizumab have shown promise in managing prurigo nodularis by inhibiting specific inflammatory pathways involved in the pathogenesis of the condition.
Phototherapy
Phototherapy, which involves exposing the affected skin to controlled doses of ultraviolet light, can be an effective treatment modality for prurigo nodularis. Narrowband UVB phototherapy has been shown to reduce pruritus and improve the appearance of prurigo nodules. This treatment is typically administered two to three times per week in a dermatologist’s office or a phototherapy center. Psoralen plus UVA (PUVA) therapy, which combines the use of an oral or topical photosensitizing agent with UVA light exposure, has also been used to treat prurigo nodularis. The excimer laser, a type of targeted phototherapy, can be employed to treat individual, recalcitrant nodules that have not responded to other therapies. While phototherapy can be beneficial, it is important to consider the potential long-term risks associated with UV exposure, such as premature skin aging and increased risk of skin cancer.
Conclusion
Prurigo nodularis is a complex skin condition that has a significant impact on those affected. This article has shed light on its key aspects, from its defining features and symptoms to the various factors that contribute to its development. Understanding the condition’s characteristics, potential causes, and available treatment options is crucial to manage it effectively. With a range of therapies available, from topical treatments to systemic medications and phototherapy, there’s hope for those struggling with this persistent disorder.
While prurigo nodularis can be challenging to treat, ongoing research and new therapeutic approaches are paving the way for better management strategies. By working closely with healthcare providers and exploring different treatment options, individuals with prurigo nodularis can find relief from their symptoms and improve their quality of life. As our understanding of this condition grows, so does the potential to develop more targeted and effective treatments in the future.