Pulmonary fibrosis is a devastating lung condition that affects thousands of people worldwide. This progressive disease causes scarring in the lungs, making it increasingly difficult for those affected to breathe. As the condition worsens, it has a significant impact on a person’s quality of life and can ultimately lead to respiratory failure.
This article aims to explore the complexities of pulmonary fibrosis in depth. It will delve into the science behind the disease, discussing its causes and how it develops. Additionally, it will examine the various treatment options available to patients, from medications to lifestyle changes. The piece will also shed light on the challenges of living with pulmonary fibrosis and provide insights into managing the condition effectively.
The Science Behind Pulmonary Fibrosis
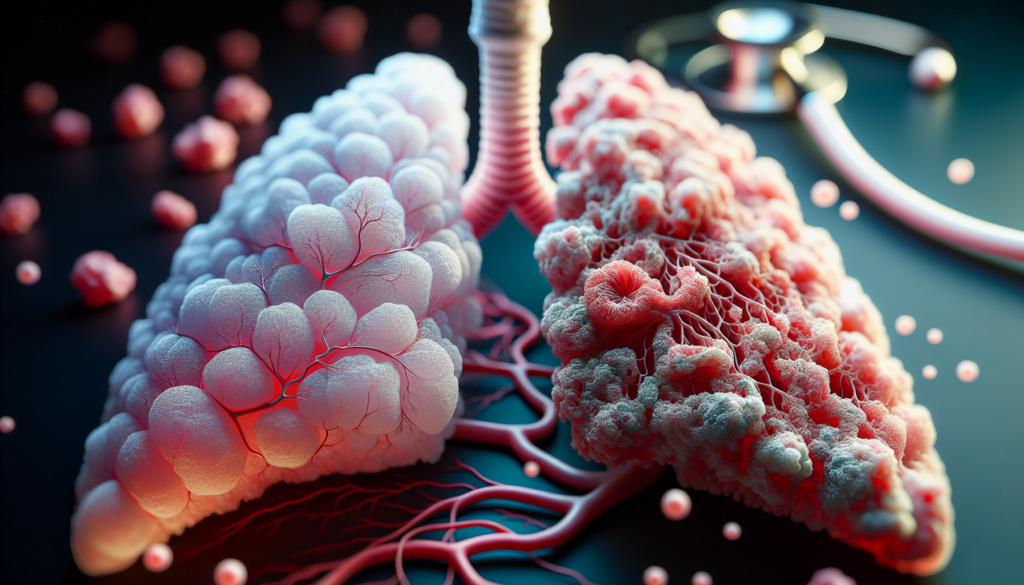
Pulmonary fibrosis occurs when the tissue around the air sacs in the lungs becomes damaged and scarred. This scarring causes the lungs to stiffen, making breathing increasingly difficult. To understand how pulmonary fibrosis develops, it is essential to examine the anatomy of the lungs and the process of fibrosis itself.
Anatomy of the Lungs
The lungs are composed of numerous tiny air sacs called alveoli. These alveoli are surrounded by a network of blood vessels, which facilitate the exchange of oxygen and carbon dioxide between the lungs and the bloodstream. In a healthy lung, the alveoli are elastic and can expand and contract easily during breathing.
RELATED: Your Guide to Understanding Merkel Cell Carcinoma and Its Treatments
The Fibrosis Process
In pulmonary fibrosis, the tissue around the alveoli becomes damaged and inflamed. This inflammation triggers a healing response, which leads to the formation of scar tissue. As the scar tissue accumulates, it causes the lungs to thicken and lose their elasticity. This process is known as fibrosis.
Several factors can contribute to the development of pulmonary fibrosis:
- Environmental exposures: Inhaling harmful substances such as asbestos, silica, or metal dusts can cause lung damage and lead to fibrosis.
- Certain medications: Some medications, particularly those used to treat cancer or heart conditions, can have side effects that damage the lungs and trigger fibrosis.
- Autoimmune disorders: Conditions like rheumatoid arthritis and scleroderma can cause the immune system to attack the lungs, leading to inflammation and scarring.
- Genetic factors: In some cases, pulmonary fibrosis may run in families, suggesting a genetic component to the disease.
Alveoli and Gas Exchange
As pulmonary fibrosis progresses, the scarring and stiffening of the lungs impair the function of the alveoli. The thickened tissue makes it difficult for oxygen to pass from the alveoli into the bloodstream, leading to a decrease in oxygen levels in the body. This oxygen deprivation can cause symptoms such as shortness of breath, fatigue, and a persistent dry cough.
Furthermore, the loss of elasticity in the alveoli makes it harder for the lungs to expand and contract during breathing. This reduced lung capacity contributes to the feeling of breathlessness experienced by individuals with pulmonary fibrosis.
Understanding the science behind pulmonary fibrosis is crucial for developing effective treatments and management strategies. While there is currently no cure for the disease, ongoing research aims to identify new therapies that can slow the progression of fibrosis and improve the quality of life for those affected by this condition.
Treatment Options
While there is no cure for pulmonary fibrosis, several treatment options are available to manage symptoms, slow disease progression, and improve quality of life. These include medications, oxygen therapy, pulmonary rehabilitation, and lung transplantation.
Medications
Antifibrotic drugs are approved for the treatment of idiopathic pulmonary fibrosis. These medications have been shown to slow the decline in lung function and disease progression. Other medications like corticosteroids may be used to treat inflammation in certain forms of pulmonary fibrosis.
Oxygen Therapy
As pulmonary fibrosis progresses, the lungs’ ability to transfer oxygen to the bloodstream becomes impaired. Supplemental oxygen, also known as oxygen therapy, can help improve oxygen levels in the body, reduce symptoms like shortness of breath and fatigue, and enhance overall quality of life. Oxygen needs are unique to each patient and depend on the severity of their disease and lifestyle.
RELATED: Muscular Dystrophy Insights: From Symptoms to Advanced Treatments
Pulmonary Rehabilitation
Pulmonary rehabilitation is a comprehensive program that combines exercise, education, and support to help patients with pulmonary fibrosis manage their condition and improve their well-being. It typically includes supervised exercise training, breathing techniques, energy conservation strategies, and counseling. Pulmonary rehabilitation has been shown to improve lung function, reduce symptoms, and enhance quality of life in patients with pulmonary fibrosis.
Lung Transplantation
For selected patients with advanced pulmonary fibrosis, lung transplantation may be a treatment option. It involves replacing one or both diseased lungs with healthy lungs from a donor. While lung transplantation can improve survival and quality of life, it is a major surgery with potential risks and complications. Patients should be evaluated by a lung transplant physician soon after diagnosis to determine their eligibility for the procedure.
In summary, a multidisciplinary approach involving medications, oxygen therapy, pulmonary rehabilitation, and potentially lung transplantation is crucial in managing pulmonary fibrosis. Treatment plans should be tailored to each patient’s unique needs and goals, with a focus on slowing disease progression, reducing symptoms, and optimizing quality of life.
Living with Pulmonary Fibrosis
Living with pulmonary fibrosis presents numerous challenges, but there are strategies to manage symptoms, make necessary lifestyle adjustments, and seek emotional and psychological support.
Patients with pulmonary fibrosis often experience distressing symptoms such as cough, dyspnea, and fatigue. A palliative care specialist can provide personalized side effect management strategies. For cough, patients may benefit from treating underlying causes, using cough drops or medications, and practicing speech therapy techniques. Shortness of breath can be managed with oxygen therapy, breathing techniques, medications, and staying active through pulmonary rehabilitation. Fatigue may be alleviated by getting adequate rest, staying active, eating a nutritious diet, and using oxygen as directed.
Lifestyle changes are often necessary to adapt to the limitations imposed by pulmonary fibrosis. Patients may need to make modifications to their home environment, such as installing ramps or stairlifts, to facilitate mobility. They may also need to adjust their daily routines, prioritizing essential tasks and delegating others to family members or caregivers. Maintaining a healthy lifestyle through regular exercise, a balanced diet, and avoiding smoking is crucial for managing the disease.
RELATED: Effective Home Remedies for Mouth Ulcers You Need to Know
The emotional and psychological impact of pulmonary fibrosis can be substantial. Patients may experience feelings of anger, frustration, anxiety, sadness, and fear. Seeking support from family, friends, and healthcare professionals is essential. Joining a support group can provide a sense of community and allow patients to share their experiences and coping strategies. Counseling or therapy can help patients and their families navigate the emotional challenges of living with pulmonary fibrosis.
Palliative care, which focuses on symptom management and quality of life, can be beneficial at any stage of the disease. It is important for patients to communicate openly with their healthcare team about their needs and concerns. By working together, patients, caregivers, and healthcare professionals can develop a comprehensive plan to manage the physical, emotional, and practical aspects of living with pulmonary fibrosis.
Conclusion
Pulmonary fibrosis has a significant impact on the lives of those affected, presenting challenges that extend beyond physical symptoms. The disease’s progression and its effects on lung function necessitate a comprehensive approach to management, involving medical treatments, lifestyle adjustments, and emotional support. This multifaceted strategy aims to slow the disease’s advancement, alleviate symptoms, and enhance the overall quality of life for patients.
Looking ahead, ongoing research holds promise to develop new therapies and improve existing treatments for pulmonary fibrosis. While a cure remains elusive, advancements in understanding the disease mechanisms and potential genetic factors offer hope for more targeted interventions. For those living with pulmonary fibrosis, a combination of medical care, support systems, and personal resilience is key to navigate the challenges posed by this condition.