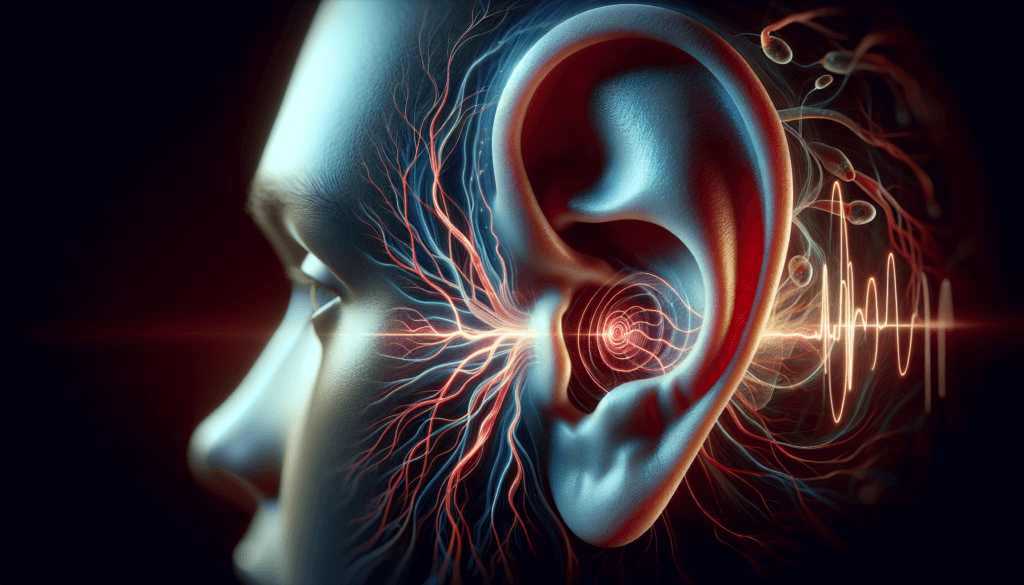
Imagine a constant, rhythmic sound in your ear that syncs with your heartbeat. This is the reality for those experiencing pulsatile tinnitus, a unique form of tinnitus that affects many individuals worldwide. Unlike regular tinnitus, which often presents as a constant ringing or buzzing, pulsatile tinnitus has a distinct pulsing quality that can significantly impact a person’s daily life and well-being.
Understanding pulsatile tinnitus is crucial for both patients and healthcare providers. This article aims to shed light on the causes behind this condition, explore its symptoms, and discuss effective treatment options. By delving into the vascular origins of pulsatile tinnitus and examining various therapeutic approaches, readers will gain valuable insights to help manage this challenging condition and improve their quality of life.
Understanding the Symptoms
Characteristics of Pulsatile Tinnitus
The most distinctive feature of pulsatile tinnitus is the perception of a rhythmic sound that often synchronizes with the individual’s heartbeat. This pulsating noise can be described as a whooshing, thumping, or throbbing sensation, which may be heard in one or both ears. Unlike the more common form of tinnitus, where the sound is constant and non-pulsatile, pulsatile tinnitus has a distinct pattern that follows the rhythm of the cardiovascular system.
The intensity of pulsatile tinnitus can vary from person to person. Some individuals may experience a soft, barely noticeable sound, while others may be subjected to a loud and disruptive noise. The volume of the pulsatile tinnitus may fluctuate depending on factors such as physical exertion, stress levels, and changes in blood pressure. In some cases, the sound may be more prominent at night when external noises are minimal, making it easier for the individual to focus on the internal pulsations.
RELATED: Neurofibromatosis Type 1 (NF1): Diagnosis, Symptoms, and Treatment
Associated Symptoms
While pulsatile tinnitus is the primary symptom, some individuals may experience additional signs and symptoms related to the underlying cause of their condition. These associated symptoms can provide valuable clues for healthcare providers in determining the root cause of pulsatile tinnitus.
One such associated symptom is headaches. Individuals with idiopathic intracranial hypertension, a condition characterized by increased pressure in the fluid surrounding the brain, may experience both pulsatile tinnitus and persistent headaches. These headaches often occur in conjunction with visual disturbances, such as blurred vision or double vision, due to the elevated intracranial pressure.
In some cases, pulsatile tinnitus may be accompanied by hearing loss or a feeling of fullness in the affected ear. This can be indicative of a structural abnormality within the ear itself, such as superior semicircular canal dehiscence syndrome, where a thinning or absence of bone overlying the inner ear canal can lead to pulsatile tinnitus and hearing-related symptoms.
Impact on Daily Life
The presence of pulsatile tinnitus can have a significant impact on an individual’s quality of life. The constant, rhythmic sound can be a source of distraction and annoyance, making it difficult for the person to concentrate on daily tasks or engage in social interactions. The intrusive nature of pulsatile tinnitus can lead to increased stress levels, as the individual may find it challenging to escape the persistent noise.
Sleep disturbances are another common consequence of pulsatile tinnitus. The pulsating sound may become more noticeable in quiet environments, such as when trying to fall asleep at night. This can result in difficulty initiating or maintaining sleep, leading to daytime fatigue and reduced overall well-being.
Moreover, the psychological impact of pulsatile tinnitus should not be overlooked. The constant presence of the sound can trigger feelings of anxiety, frustration, and even depression in some individuals. The uncertainty surrounding the cause of pulsatile tinnitus and the potential for an underlying serious health condition can further contribute to emotional distress.
Vascular Causes of Pulsatile Tinnitus
Arterial Causes
Arterial causes of pulsatile tinnitus are responsible for approximately 23% of cases. Atherosclerotic carotid artery disease is the most common arterial etiology, where stenosis in the carotid arteries leads to turbulent blood flow that can be perceived as pulsatile tinnitus. Other arterial causes include fibromuscular dysplasia and Takayasu disease, although these are much rarer. Paragangliomas, also known as glomus tumors, of the jugular foramen, middle ear, or carotid body can also result in pulsatile tinnitus due to their high vascularity and proximity to the ear.
Venous Causes
Venous etiologies account for about 28% of pulsatile tinnitus cases, with idiopathic intracranial hypertension (IIH) being the most common venous cause. IIH, also known as pseudotumor cerebri, is characterized by high pressure in the cerebrospinal fluid around the brain, leading to symptoms such as headaches, dizziness, hearing loss, and pulsatile tinnitus. Patients with IIH perceive rhythmic changes in cerebrospinal fluid pressure, resulting in the pulsatile tinnitus. Venous sinus diverticulum, where a small abnormal pouch on the vein wall transmits sound to the ear, is another potential venous cause of pulsatile tinnitus.
RELATED: Neuroblastoma Treatments: A Detailed How-to Guide
Arteriovenous Malformations
Arteriovenous malformations (AVMs) are responsible for approximately 18% of pulsatile tinnitus cases. AVMs are abnormal connections between arteries and veins that disrupt normal blood flow, leading to turbulence and the perception of pulsatile tinnitus. Dural arteriovenous fistulas (DAVFs) are a type of AVM that can cause pulsatile tinnitus. The abnormal connection between arteries and veins in DAVFs allows high-pressure arterial blood to enter the low-pressure venous system, leading to turbulence and the characteristic whooshing sound of pulsatile tinnitus.
In summary, vascular causes of pulsatile tinnitus can be divided into arterial, venous, and arteriovenous malformations. Identifying the specific vascular etiology is crucial for determining the appropriate treatment approach. A thorough diagnostic workup, including imaging studies such as CT angiography, MR angiography, and venography, can help pinpoint the underlying vascular cause and guide management decisions for patients with pulsatile tinnitus.
Treatment Options
Medical Management
Medical management of pulsatile tinnitus focuses on addressing the underlying cause. If hypertension is identified, blood pressure control through medication and lifestyle changes can alleviate symptoms. Anemia, another potential cause, should be treated with iron supplementation or other appropriate therapies. In cases of idiopathic intracranial hypertension, medications like acetazolamide can be used to lower intracranial pressure and improve pulsatile tinnitus.
Surgical Interventions
When anatomical abnormalities are responsible for pulsatile tinnitus, surgical intervention may be necessary. For venous sinus stenosis, stenting of the affected vein can restore normal blood flow and eliminate the pulsating sound. Glomus tumors and arteriovenous malformations may require surgical removal or embolization to resolve pulsatile tinnitus. In cases of sigmoid sinus wall abnormalities, such as dehiscence or diverticulum, surgical repair of the affected area can be highly effective in alleviating symptoms.
RELATED: Ultimate Guide to Nephrotic Syndrome: Symptoms, Causes, and Care
Sound Therapy and Lifestyle Changes
Sound therapy, using external noise to mask or distract from the pulsatile tinnitus, can provide relief for some patients. White noise machines, fans, or even smartphone apps that generate soothing sounds may be helpful. Stress management techniques, such as relaxation exercises, meditation, and cognitive-behavioral therapy, can also play a role in reducing the impact of pulsatile tinnitus on daily life. Lifestyle modifications, including regular exercise, healthy sleep habits, and avoidance of triggers like caffeine and alcohol, may further contribute to symptom management.
Ultimately, the treatment approach for pulsatile tinnitus must be tailored to the individual patient based on the underlying cause and severity of symptoms. Close collaboration between healthcare providers, including otolaryngologists, radiologists, and neurologists, is essential for accurate diagnosis and effective management of this challenging condition.
Conclusion
Pulsatile tinnitus has a significant impact on those affected, causing distress and disrupting daily life. This condition’s unique nature, with its rhythmic sound synced to the heartbeat, sets it apart from other forms of tinnitus. Understanding its vascular origins and exploring various treatment options are key to managing this challenging disorder effectively.
To wrap up, a tailored approach is crucial to address pulsatile tinnitus. This may involve medical management, surgical interventions, or lifestyle changes depending on the underlying cause. By working closely with healthcare providers and staying informed about the latest advancements, individuals with pulsatile tinnitus can take steps to improve their quality of life and find relief from this persistent condition.